Q Exchange
Addressing health inequalities by co-developing change to reduce missed appointments
- Winning idea
- 2023
Meet the team
Also:
- Tim Keen
- Sanjoy Shah
- Adwoa Webber
- Fiona Spence
- Monira Ahmed Chowdhury
What is the challenge your project is going to address and how does it connect to the theme of 'How can improvement be used to reduce delays accessing health and care services'?
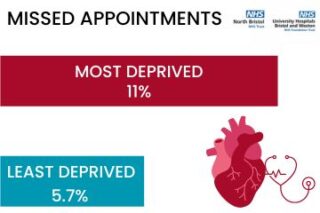
In Bristol, North Somerset and South Gloucestershire (BNSSG) the Cardiology Did Not Attend (DNA) rate for patients from ethnic minority groups is 36% higher than non-ethnic minority groups. The DNA rate is 48% higher for those who live in the most deprived areas, compared to the least deprived areas. There is a strong link between heart health and health inequalities, highlighting the urgent need to improve cardiovascular health in BNSSG.
NHS England suggests that missed appointments lead to worse care for patients, inefficient use of staff and increased waiting times. This can be avoided if we work with patients to deliver healthcare that is more accessible. We will build on our award winning system outreach work during the pandemic, collaborating with patients to design and test interventions, reducing delays and improve access to care.
The key: we want to listen, co-design and act, so patients have better health.
What does your project aim to achieve?
Our aim is to reduce the variance in DNA rate by socioeconomic factors and ethnicity across the BNSSG population. We will do this by:
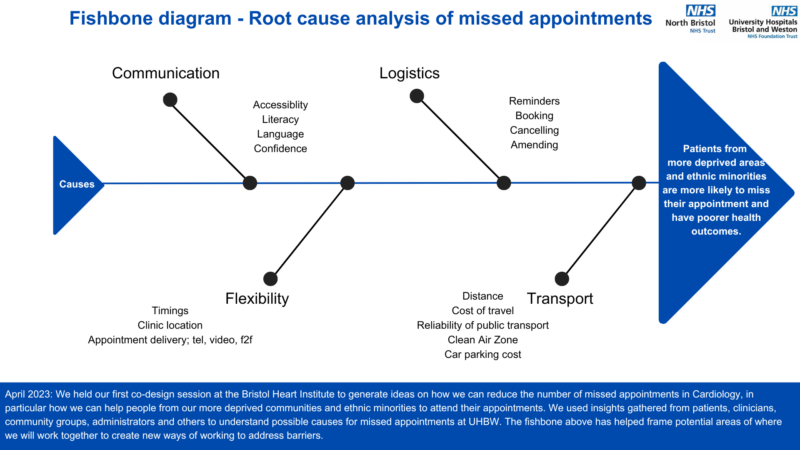
1. Understanding the barriers faced by our target patient group. Direct outreach work with patients, community groups, system partners and clinicians, will provide holistic insights and enable targeted planning and improvement of cardiology service areas that currently may lead to inequity in outcomes.
2. Co-designing improvements with patients and implementing these to test solutions. We will ensure that under-served populations have a voice in the design of healthcare services that directly affect them.
We want the impact of this project to be far-reaching, both locally and nationally. While we are starting with the cardiology service, we anticipate that the relevant solutions we develop could be applied to other specialties locally and more widely.
Clear communication, trust-building, and patient education will be at the core of our approach.
How will the project be delivered?
The project will be led by the BNSSG Elective Recovery Inequalities Integrated Care System Steering Group and the Outpatient Board at the Integrated Care Board. We are working with cardiology patients, community champions, both hospital trusts (NBT & University Hospitals Bristol and Weston NHS Foundation Trust), Voluntary, Community and Social Enterprise sector and clinicians.
Examples of interventions we will test include transport solutions, venue hire, posters and patient communications, translation services, primary care communication and funding to pay for public participants’ time e.g., gift vouchers.
We will measure the impact of intervention through:
o Monitoring Did Not Attend rates for the target patient group.
o Patient satisfaction: regular surveys can be used to measure satisfaction with the cardiology service and identify areas for improvement.
o Staff satisfaction: monitoring the effectiveness of interventions through capturing feedback regularly.
o Cost-effectiveness: we will measure the cost of missing appointments versus the cost of interventions.
How is your project going to share learning?
We will contribute to both a broader shift towards patient-centred healthcare delivery and a culture of continuous improvement, by sharing our findings post-implementation through Q Exchange project page updates. We will leverage the Q community as a key network to engage other healthcare providers to take part; more externally, we will share learnings with NHS England for a wider reach. We will document the evaluated aspects of the project for publication in peer reviewed journals and submit conference abstracts to national and international conferences, while participating in other Q exchange virtual events to share our insights and promote collaboration. Our approach to addressing health inequalities can be replicated across the healthcare system to ensure all patients receive the care they need, in the way that suits them.
We will also encourage our community public contributors to share learning through their groups and networks with specific communications for inclusion groups.
How you can contribute
- We are calling on members to:
- 1) Review what we are doing.
- 2) Share what you are doing.
- 3) Let us know what more we could be trying.
- Some areas you could help us with include sharing ideas on:
- 1) Improving contact access and cancellation/rebooking processes
- 2) Improving communication with patients waiting for care
- 3) Improving provider access policies
- 4) Implementing digital enablers, including tools that could be used to predict likelihood of future Did Not Attends (DNAs)
- How can you help? – Are you:
- 1) The expert? You can share your expertise based on your professional background or personal experience.
- 2) The networker? You can make introductions for us and link up similar ideas.
- 3) The critical friend? You can provide challenge on the idea to help improve it and suggest areas for further exploration.
Plan timeline
| 3 Apr 2023 | Analyse feedback from Cardiology patient survey, grouping barriers into themes |
|---|---|
| 1 May 2023 | Test cardiology clinic SMS reminders. Develop algorithm to predict DNAs |
| 5 Jun 2023 | First phase of community co-design groups. Content creation - translated material. |
| 3 Jul 2023 | Administrator to contact patients in IMD 1 & 2 areas, offering improved access |
| 7 Aug 2023 | 3 months post- SMS intervention data review and feedback |
| 4 Sep 2023 | Second phase of community co-design groups - obtain feedback on progress |
| 2 Oct 2023 | Continued implementation with data-driven iteration. Regular updates to stakeholders |
| 1 Apr 2024 | Undertake final data analysis. Finalise end of year project report. |
| 6 May 2024 | Project completion. Share findings locally and nationally through webinars |
Project updates
22 Jan 2024
Q-Exchange 5 Mid-Project Update
What have you learned so far?
- So far we have been able to identify the main barriers to attendance for patients from more deprived and ethnically diverse backgrounds when given an outpatient appointment.
- We were led by the data throughout – in-depth analysis of our outpatient data enabled us to carry out a targeted approach when engaging with diverse stakeholders across the Bristol, North Somerset, and South Gloucestershire (BNSSG) region.
- By categorising and understanding the problem via geography, we were able to define the individual challenges patients from each local area could be facing when trying to access their healthcare.
- We found common issues around communication – letters were either too complex or often not received in time. There were distinct barriers for others. For example, in the Inner City and East of Bristol, language was a barrier for some members of our diverse community. Other barriers which frequently appeared included transport distance and transport costs.
- When a barrier was presented, we asked the person what they thought the solution would be to that particular challenge.
- We are grateful for these inputs, as we now have a better understanding of the needs of our local population and the opportunities to resolve some of these issues.
- By reviewing best practice and initiatives that have been trialled and implemented across other Trusts and Regions, we were able to proactively identify what works well and what may be feasible for our local population.
What could others learn from your experience of working with a range of stakeholders and collaborating across boundaries (geographical, professional, sector)?
- It is important to tailor your communication approach depending on each stakeholder.
- Through this project we engaged over 300 people: ranging from patients (gathering feedback digitally, over the telephone and face-to-face), relevant NHS colleagues, General Practitioners and GP Managers, local community groups and Community Champions.
- Having a good understanding of different groups across the region allowed us to plan and schedule in time to have discussions with everyone.
- Being intentional about the questions we asked enabled us to have focussed conversations which explored the challenges people face and more importantly what we could be doing as a hospital to resolve these issues.
- Our experience of engaging and collaborating with local communities was very positive. People were willing to share their ideas and invite us into their spaces to discuss the impact of health inequalities.
- Conducting focus groups across Bristol was a brilliant way to capture qualitative feedback which could in-part explain some of the quantitative data we started off with. Patients were engaged, offered their opinion, and produced solutions to problems raised in the focus groups.
- By engaging stakeholders across the spectrum, this project truly feels like a collaborative effort with our local communities.
What are the next steps for your project over the coming months?
- We are currently in the process of recruiting for an administrator, which is trickier than it seems!
- The administrator will call patients in advance of their appointment to help troubleshoot any concerns and signpost to relevant support services required by the patient.
- The aim of this added layer of communication is to improve attendance rates overall.
- We are also in the process of disseminating the findings. An in-depth insights report has been produced, which will be shared with relevant groups, including our community champions.
- We have developed an options appraisal and will be implementing feasible ideas in the coming months.
How can the community get involved in your project?
We will continue to connect with Q members to learn from them. We welcome anybody from across the Q-community who have implemented similar work, including sharing what they found went well and any challenges they tried to overcome in the context of this work.
Thanks for everyone’s support on our project to date!
Khadija
1 Nov 2023
Reflecting on September’s Q-Exchange celebration event for cohort 4 and 5 award winners; we had the opportunity to meet others from across the UK quality improvement community, working on a range of complex challenges. The “Troika consulting” liberating structures technique was a particularly useful method to understand challenges faced by different project teams and generate ideas to address obstacles. Thank you to The Health Foundation for inviting us to this special event.
Since then we have completed our initial project insights phase, addressing our primary aim of trying to understand the barriers faced by our target patient group when it comes to missed appointments. We have already engaged over 300 people through this project. We’ve gathered improvement ideas to reduce inequity in outcomes by directly reaching out to patients, community groups, system partners and clinicians.
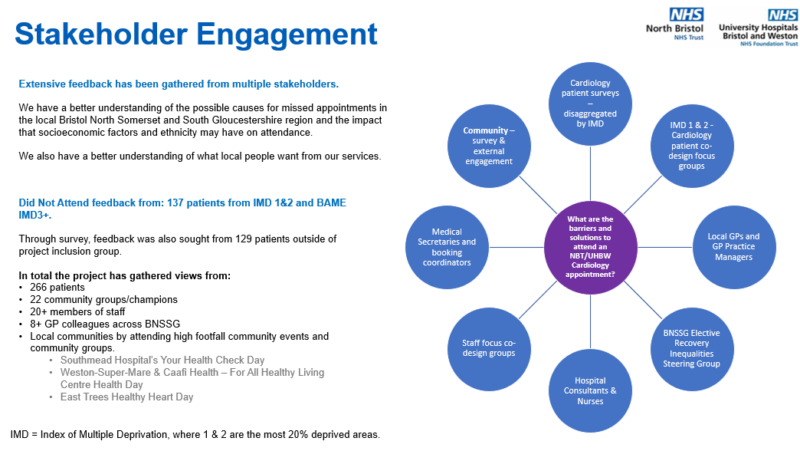
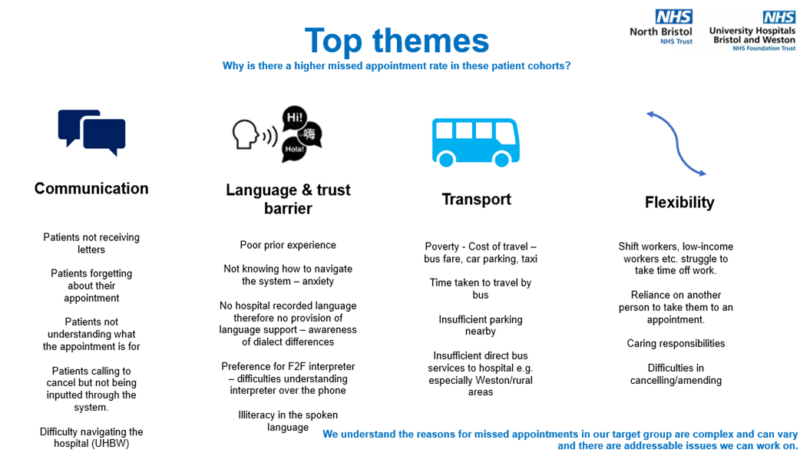
The two slides attached provide an overview of our stakeholder engagement and top themes for missed appointments.

Comments
Nikki Davey 20 Jun 2023
Hi and congratulations - I thought you might like to see this QI project undertaken on our 'Improve 'ONE thing: the Full QIP Course' by a parent learner, Charity Gondwe, https://qiclearn.com/sorry-we-dont-attend-clinic-because-2/ . Any questions - or to contact Charity you can contact me nicola@qualityimprovementclinic.com
Helen Davies-cox 31 May 2023
Great idea, I'd be keen to understand more about your algorithm.
Charlie Jones 30 May 2023
Hi everyone, this sounds such a worthwhile project. I wonder if there could be any link to the aspiration to become a 'trauma informed' Integrated Care System? I wonder about the prevalence of trauma in deprived areas and in minority groups & whether 'trauma informed practice' could add a useful layer of meaning to your project?? Best wishes with it
Khadija Begum 31 May 2023
Hi Charlie.
We hadn't thought about looking at it this way. Thanks for the suggestion.
Tina Yarnton 30 May 2023
Hi Team, would be great to see/hear specialist teams who are also taking clinics to their most deprived communities. If anyone is already using the same space as other health services in the community to target DNA rates in specific ethnic populations, it would marvellous to see the impact this has/could have. If cardiac rehab, or pulmonary rehab are in the community, could your team be there too? Talk to community health providers and find out.
Good luck with your project.
Khadija Begum 31 May 2023
Hi Tina, thanks for your comment.
From our co-design session at the Bristol Heart Institute, a colleague from the Cardiac Rehabilitation team joined to offer community insights. They run community sessions and are looking to improve accessibility for service users across the Bristol and Weston catchment areas. I am liaising with the Lead Cardiac Rehab Practitioner directly to see if there is scope to get involved with this work.
Moving a clinic to local areas for those most at risk of missing their appointment, where possible, would be a good intervention to trial for this project.
Oliver Watson 30 May 2023
Great project, brilliant team and wonderful to see the links here into public health and strong support from the ICB. Look forward to hearing about the progress
Khadija Begum 31 May 2023
Thanks for your support Oliver.
Dr Seema Srivastava MBE 27 May 2023
My colleague Sanjoy Shah (Deputy Chief Medical Officer at North Bristol Trust) and I, presented our system work on reducing Health Inequalities in Elective Recovery, including our Q Exchange project, to the Bristol, North Somerset and South Gloucestershire Integrated Care System Health and Care Professionals Executive meeting this month.
The meeting is chaired by Dr Joanne Medhurst, Chief Medical Officer for NHS Bristol, North Somerset and South Gloucestershire ICB and the feedback from health and care leaders was incredibly positive with offers to unblock barriers to progress.
In response to the shortlisting of our Q Exchange Project, Dr Joanne Medhurst said:
“Tackling health inequalities is a key priority for our health and care system and this project is an excellent example of how partners are working together to explore interventions to improve health outcomes for people from our most deprived communities.
“While this project focuses on missed appointments within cardiology, it could also provide learning and evidence to positively influence missed appointments and elective recovery at a wider scale.”
Christina Gray DPH Bristol 26 May 2023
Really delighted to see the development of this programme, its also excellent to see the two trusts working together on this. I will share with our community health champions and community development work networks and ask them also to comment. I am sure we could facilitate some community conversations with you, it is often surprising what barriers are for different communities. Can we look together at broader communication / prevention messages - appointment take up possibly an indicator of health need / behaviours?
Dr Seema Srivastava MBE 27 May 2023
Thank you Christina. The collaboration with our healthcare providers, Public Health colleagues, community leaders and networks during the pandemic has built a strengthened relationship in BNSSG, through which we can make further health improvements. We are delighted that you as the Director for Communities and Public Health in Brístol, are supporting this Q Exchange project and our ambition to continue codeveloping better access for our population experiencing the widest health inequalities 🙏🏽
Khadija Begum 22 May 2023
Hello Q Community!
Ahead of the next Q Exchange phase: voting, we thought it would be good to share the project's progress since initially submitting our idea.
Progress
Completed the first phase of mixed community engagement including:
For the Q community: This is what we are thinking about doing for our next steps – we would be grateful for your input!
Guddi Singh 23 Mar 2023
This is brilliant! We are also submitting a project to address health inequalities but focussing on learning from young people's perspectives... Please check it out: https://q.health.org.uk/idea/2023/powering-up-co-producing-solutions-to-health-inequality-with-young-people/?nid=61971
I think we have a lot of shared aspirations and I think we could learn a lot from the work that both sides are trying to do. Perhaps we could even combine our learning together at some point?
Regardless, I just wanted to extend a hand of friendship and allyship and hope that our paths cross at some point! ;) Good luck!
Khadija Begum 24 Mar 2023
Hi Guddi,
Thanks for your comment. I'll take a look at your project now - very keen to work with you on the shared aim of reducing health inequalities.
Hein le Roux 21 Mar 2023
This is such an important project as your statistics set out and it is in all our interests to find ways to close that health inequalities gap locally and then share learning so other areas such as ours can take similar measures. In primary care we have just this year collected a great deal of ethnicity data by coding over 90% of our populations which will give us a much more granular view of patient groups which can be cross referenced for projects like yours. Best of luck and please be sure to share learning.
Khadija Begum 22 Mar 2023
Hi Hein,
Thanks for your comment. It’s brilliant to hear about your recent work on coding ethnicity, especially because patients sit on a spectrum of diversity - the barriers to healthcare will of course be diverse too! This piece for example, https://www.england.nhs.uk/aac/wp-content/uploads/sites/50/2023/02/B1905-increasing-diversity-in-research-participation.pdf showed top barriers for underrepresentation in health research were language, access and trust. I imagine we'll see something similar.
We’ve started reaching out to local GPs (in particular those who have referred patients to the hospital and have high DNAs) and there are already different themes emerging. It’s an exciting space to be in as we’re trying to involve a range of stakeholders. Will definitely share around our findings and recommendations.
Iain Smith 13 Mar 2023
Hi Seema,
I think there's some synergy here between your idea and one I've put forward - https://q.health.org.uk/idea/2023/transforming-outpatients-through-coproduction-and-health-literacy/
It would be great to perhaps connect and compare note. Also, a colleague recently shared with me this short article which you may find interesting. https://www.nth.nhs.uk/news/trust-pilot-scheme-to-reduce-missed-appointments-saves-more-than-10000/
Dr Seema Srivastava MBE 20 Mar 2023
Hi Iain
Yes definitely lots of synergy with our projects and enormous opportunities to learn from each other's work. It would be great to connect with you on this. Thanks for the article link.
Parya Rostami 10 Mar 2023
I really like this. The data makes it so clear there is a problem with access to services for some groups, yet we don’t do enough to understand the issues and why. When we do understand it can be so powerful for change. E.g. I recently heard about poor attendance from Pakistani communities to a memory service clinic, when they investigated why it was because it was based in a mental health hospital and because of the stigma attached. They provided another location and attendance went up significantly!
I look forward to hearing more about this work and learning!
Khadija Begum 11 Mar 2023
Thanks for sharing your thoughts Parya. It'd be great to hear more about the work with the Pakistani community if you have it to hand, as this is one type of solution we'd expect to implement for our patients as part of this project. I don't expect there to be a one-size fits all approach, so understanding what others have done would be very useful for the testing phase.
Anna Burhouse 9 Mar 2023
Hi Seema,
what a great idea. If it's helpful I can link you in with the Common Ambition Bristol team who are learning so much about how to improve access to HIV services for African and Caribbean communities locally. There might be great synergy to explore.
warm wishes
Anna
Dr Seema Srivastava MBE 9 Mar 2023
That would be amazing Anna. Thank you.
Dimple Keen 7 Mar 2023
Hi Seema and team,
A really great idea! Focusing on patient education and understanding the 'why' will be really important. I wonder if there could be some budget and time set aside for developing a structured comms campaign, which can be shamelessly stolen by others (!), so that we can use your insights in other specialties and across the UK.
Small thing to bear in mind - you may not necessarily see improvements in throughput and waiting lists, as I imagine clinics are overbooked to allow for the high DNA rates.
I'm working in cardiovascular so would love to hear how you get on.
All the best with your application!
Dr Seema Srivastava MBE 7 Mar 2023
Thanks Dimple for your comment. Really good point about potentially overbooked clinics. I will take this back to our project team to see what impact this may have on our data.
Comments are now closed for this post.