Q Exchange
Medication Safety App: Empowering Patients to Keep Their Medication Lists
- Proposal
- 2023
Meet the team
Also:
- Bernie O'Reilly, Ciara Kirke; Mila Whelan, Sheila McConnell, Anne McCabe Kelly
What is the challenge your project is going to address and how does it connect to the theme of 'How can improvement be used to reduce delays accessing health and care services'?
Research from the WHO, HSE and others show that unsafe medication practices and medication errors are a leading cause of avoidable harm in healthcare across the world – a huge burden of harm.
Currently, patients experience delays in accessing healthcare services due to poor communication between patients and healthcare professionals about their medicines. A complete medicines list improves the efficiency and effectiveness of paramedics, hospital admissions and outpatient appointments – indeed all appointments.
Research confirms that empowered patients who know and understand their medications, dosage, frequency, etc. reduces adverse events arising from medication errors. Sharing information with healthcare professionals at the point of care enables HCPs to act more quicky, knowing the patient’s current medications – prescribed as well as over-the-counter.
In Ireland, an initiative is underway to circulate a medication list to patients. Feedback from patients and healthcare professionals is that an app is easier to keep up-to-date and will increase uptake/adoption.
What does your project aim to achieve?
WHO World Patient Safety Day 2023 Theme: Patient Engagement. PFPSI aims to empower patients with the WHO Know, Check, Ask message. https://cdn.who.int/media/docs/default-source/world-patient-safety-day/masters-a2-patients-posters-v1-ok.pdf?sfvrsn=abd895b4_1.
We will design, develop and deliver a free, low-complexity, accessible, engaging and easily navigable mobile app that meets patient needs – empowering patients to understand their medications, dosage, frequency, etc . The app is based on existing HSE Ireland leaflets and meets WHO guidelines for an app: data stored locally (no cloud element) and free for patients globally.
The proposed timeframe is 6 months from design to delivery of the app, followed by 6 months of project team PDSA cycles and questionnaire-based user testing, piloting & enhancing the app with patients as a proof of concept.
Patients using this app will report improved communication with healthcare professionals and increased confidence to discuss medications with healthcare professional teams; the ultimate goal to reduce medication errors under three scenarios:
- High risk situations
- Polypharmacy
- Transitions of care
How will the project be delivered?
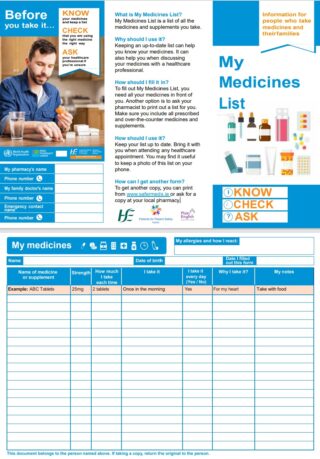
The app will be based on solid research on Medication Without Harm and an existing paper leaflet being distributed to patients (see attachment).
Unlike any other app currently available, the app will be free, available in the relevant marketplaces to anybody with Android or iPhone smartphones. Following WHO guidelines, data is only stored locally on the mobile phone.
An existing PFPSI-led, diverse group on Medication Safety – including patient representatives, advocacy groups and healthcare professionals – will meet fortnightly to provide oversight. The team has significant experience in Quality Improvement, project risk and resource management, and evaluation.
A prototype has already been built, designed for Android and iPhones. The main requirements are for further testing, accessibility testing and user testing in a series of PDSA cycles, with patient groups providing patients for user testing and rigorous accessibility testing.
General Availability plan will include a campaign involving advocacy groups, healthcare professionals and pharmacies
How is your project going to share learning?
Patients for Patient Safety and the Health Service Executive in Ireland – across community health and acute hospitals – are collaborating closely on this initiative and sharing learnings on patient empowerment and increasing patient safety when accessing care. These learnings – as well as the app – can also be shared within the Q community. The project will be presented at a QPSTalktime session and updates shared via twitter & website. The WHO Global Patient Safety network, including Patients for Patient Safety groups around the world.
The app will be fully documented. An paper will be published to share our findings to support shared learning across the UK & Ireland. We will also design a poster for local and international conferences, including the International Forum on Quality & Safety in Healthcare and IHI.
The app will be built to WHO standards and will be made available free of charge to the WHO and anyone that will benefit.
How you can contribute
- The main request is for resource to take the app from prototype to general availability, so we would welcome input from Q Community members to further enhance medication safety using this app:
- Are there any barriers to adoption by patients/caregivers or healthcare professionals?
- Expert – Have you expertise in the development of mobile apps to support HCPs in improving the quality & safety of their services? Can you contribute to our understanding of the impact on workload and ‘work as done not work as imagined'?
- Critical Friend – What are the challenges we might face in developing and promoting this app to patients and HCPs?
- Collaborator - what is the most effective way to promote this app for maximum take-up among patients and healthcare professionals?
- Networker - do you know of any other Q projects or similar relating to this?
- Advocacy Groups and Patient Safety Advocates - can we work in partnership to improve patients safety?
A simple action such as using a medicines list can help people who take medicines regularly to stay safe. It also helps the family, carers and health and social care professionals who support them.
— HSE Ireland (@HSELive) September 19, 2022
Download a medicines list template here: https://t.co/LOjyJOPqAp @NationalQPS pic.twitter.com/XFdZWWANmY
Plan timeline
| 13 Mar 2023 | 10-week period, consulting with Q Community seeking input and feedback |
|---|---|
| 1 Jun 2023 | Kickoff. Stakeholder forum to identify barriers and receive input |
| 8 Jun 2023 | Identify outstanding items for testing |
| 14 Jul 2023 | Complete development of prototypes |
| 18 Aug 2023 | Commence PDSA and User Testing Cycles- Questionnaires for User Testing |
| 29 Sep 2023 | Test for cross-platform performance |
| 20 Oct 2023 | Handover to accessibility testing |
| 24 Nov 2023 | Publication to Apple and Android marketplaces |
| 1 Dec 2023 | Test after marketplace publications |
| 8 Jan 2024 | 6 months of PDSA tests of change refine and make improvements |
| 8 Jan 2024 | Communications period between Jan and June wider group of participants |
| 4 Mar 2024 | Research on effectiveness; Learning and development |
| 21 Jun 2024 | App Launch Campaign |
Comments
Catherine Hand 18 May 2023
This is an excellent project which will really help safety medication management and I fully support it. Well done to Tibbs and all involved in this great work.
Maureen Flynn 28 Mar 2023
I am reading back and smiling at the Q community's members generous comments and suggestions - thank you. This has really helped refine our proposal. Figures crossed for the final submission - short listing and voting stages.
Tiberius Pereira 28 Mar 2023
100% agree with you, Maureen! The comments have been very helpful - every one has been incorporated into the proposal before submission. Thank you all 👏
Parya Rostami 28 Mar 2023
I absolutely love the sound of this idea, It's only when you have to start taking medicines yourself that you realise how confusing it can all be. We know that medication-related harm is one of the biggest causes of preventable harm worldwide and I really do think your idea will help to improve medication safety and uneccesary access to services.
I look forward to hearing more!
Tiberius Pereira 28 Mar 2023
Thank you, Parya. Proposal submitted, hopefully we can count on your vote 😉!
Allie Bone 24 Mar 2023
Great initiative. One i will definitely use for my elderly mother on many medications. Is there any way to link the app with the pharmacies to validate the information. Is there a risk of incorrect medication information input into the app and ?? how to mitigate against this risk.
Tiberius Pereira 28 Mar 2023
Thank you for confirming the need and the benefits, Allison. As a patient group, we too agreed that simple ideas can make a difference. Fingers crossed that we can make the app a reality in the year when Patient Engagement for Patient Safety is the theme for World Patient Safety Day!
Allison Bone 28 Mar 2023
That is great Tiberius. Transcription - known cause of medication errors. You have considered all angles. Best of luck.
Tiberius Pereira 28 Mar 2023
Hi Allie, thank you for your comment. We wanted the app to be of benefit to all patients wherever they are, following the WHO guidelines of no Cloud component. However, the app will encode the medicines list into a QR code, which a pharmacist can scan to review the list of medicines. We welcome any further comments and suggestions.
Thomas John Rose 22 Mar 2023
The best way to reduce medication errors is to ensure that ALL relevant processes and procedures are documented, understood, managed and continually improved. In my experience many processes are not clearly defined/understood never mind my other points.
Tiberius Pereira 22 Mar 2023
Provided a loong reply, but in the wrong thread. See previous thread.
Thomas John Rose 22 Mar 2023
You could be a bit clearer on your testing cycles. What are the criteria? PDSA is not really a resting cycle. A test questionnaire may be more appropriate.
Tiberius Pereira 22 Mar 2023
100% agree with your comment. We recognise that this app, in isolation, is not a fix. Patients for Patient Safety is a small group, engaging in partnership with healthcare agencies on measures to improve patient safety. In addition to joining advisory groups as patient safety advocates, we also pick a very small number of initiatives - KeepYourMedicinesList being one. Below is a potted history that may provide some context.
We started in the run-up to World Patient Safety Day, working off the WHO's Know, Check, Ask campaign and call to action. We are receiving great support from the Health Service Executive - with access to existing resources to support our campaign. We have also had good engagement across the Acute Operations and Community Health, as well as pharmacies. PFPSI are attending as many events as we can!
One of the research that has influenced our plans is a study published in BMJ Open Access: "Everyone should know what they’re on’: a qualitative study of attitudes towards and use of patient held lists of medicines among patients, carers and healthcare professionals in primary and secondary care settings in Ireland.
This is an initiative that we intend to sustain, not a short-term campaign. So we will continue to drive this message and influence processes, procedures, educating patients and healthcare professionals. In some parts of the country we now have co-ordinated initiatives across Acutes, Community and pharmacies. We are growing our stakeholder relationships every week, it seems like we're making some progress - the leaflets will be in all pharmacies across the country from next month, and we hope to measure the impact.
Apologies for the long reply. There is more to the story. Happy to provide more detail as required. Thank you again for all your feedback - it is very useful - please keep it coming.
Roisin Egenton 22 Mar 2023
Thanks Tom, that is a great suggestion and makes eminent sense!
Tibbs has managed to squeeze in a few more words in the proposal to include questionnaire-driven user testing, and the approach you have suggested will be built into the more detailed project planning behind this proposal. Thanks again for the suggestion!
Thomas John Rose 22 Mar 2023
Roisin, Thanks for your reply to my comment. During the initial design phase the PDSA cycle could be used for testing initial design updates within the design team. Once potential user groups are testing the app. then a review of their questionnaire responses will provide you with areas requiring design change. Again these design changes can be tested internally using PDSA cycles (quick and easy) followed by more user testing resulting in further ideas for design improvement (more lengthy in terms of time). This is a more efficient approach to design.
Roisin Egenton 22 Mar 2023
Thanks for this suggestion, and something for the team to reflect on. Unfortunately the tight word count limitations in the proposal don't allow us the breadth of going into a lot of detail, but if you have suggestions for how we may better reframe this in the proposal it would be most welcome!
We were aiming to use the PDSA cycles as quick iterative tests of change on a small scale to examine at how the app, and communication around the app, can be improved before it goes out to a wider audience. The PDSA cycles will test elements such as how we can effectively train people on the app (user guide? videos? demonstrations?) , and will also inform refinements to the app visuals and content. We have looked at test questionnaires as well as focus groups as tools for "Studying" each of our PDSA cycles.
Dave Milliken 16 Mar 2023
This sounds like a really great idea. Having a standard way to access a list of medications a person might be taking has several benefits. From a personal point of view, I often forget the names and doses of my meds so this would save a massive headache - currently, I save them in an online document (which takes me time to find) or I have to find out through the online portal of my doctor's surgery which is very slow and a bit hit or miss. Certainly, nothing I think I could do quickly in an emergency.
Maybe looking a bit into the future, but would it be possible to link these to the ICE (InCase of Emergency) feature on mobile phones?
https://en.wikipedia.org/wiki/In_Case_of_Emergency
(sorry to use Wikipedia)
This would be particularly useful for extreme allergies and time-dependent medication.
Tiberius Pereira 17 Mar 2023
Thank you, Dave, for taking the time to provide that feedback. Your profile was exactly the one we used when designing the app! And the challenges you mention are the ones stated by the WHO. Great minds etc.
Linking the app to ICE is a great suggestion, and one that we will include in our feasibility and design phase. Off the top of my head I wouldn't expect it to be particularly onerous. We're also considering alarms - some of our members, myself included, set alarms to take our medicines at particular times.
Please keep the ideas coming!
Maura Smiddy 15 Mar 2023
A fantastic idea. I would also perhaps be worth linking with a patient cohort that would be using the app. Certainly the elderly community and family carers are likely to have experience in terms of multi-morbidities and polypharmacy and therefore may be an appropriate groups to engage with to explore accessibility and acceptability as part of public and patient involvement for the project.
Tiberius Pereira 15 Mar 2023
Very useful feedback, thank you Maura. We will approach Age Action and family carers Ireland - those groups are generally more experienced in the three key scenarios that we are trying to address - High Risk Situations, Transitions of Care and Polypharmacy. We will also identify other advocacy groups through the National Patient Form and engage with them too, in the design phase as well as during accessibility testing. Much appreciated!
Caroline Lennon-Nally 15 Mar 2023
A medicines list has always made sense to me since the time that I worked with the Safer Meds team. I'm so pleased to see this proposal to develop a Medication Safety App.
It may be worthwhile getting a broad range of perspectives from the people using such a list to ensure a well grounded understanding of people's needs in using a list.
Tiberius Pereira 15 Mar 2023
Thank you, Caroline. As a result of your feedback we have built in a consultation phase with different groups - our members represent a number of different conditions, and we will add to that consultation with advocacy groups between now and the 1st of June. Any further input much appreciated.
Evelyn Prodger 12 Mar 2023
It will be really interesting to see the output of this - such applicability
It may be worth a stakeholder event with e.g. community nurses, palliative care teams, paramedics including non-medical prescribers to give a forum to identify barriers to use early on
Tiberius Pereira 15 Mar 2023
Thank you for the great suggestion, Evelyn. We will set up one or two events to seek input. Perhaps we can have such an event as a call to action at a Q Community event? We would appreciate any ideas on how best to identify and engage stakeholders to identify and overcome barriers.
Comments are now closed for this post.