Q Exchange
Patient led peer support initiative to promote medication safety
- Shortlisted idea
- 2018

Meet the team: East of England Citizens’ Senate
Also:
- Mary Newton
- Joanna Yellon
- Paula Wilkinson
- Adrian Pensose
- Tracey Johns
Researchers from Manchester, Sheffield and York universities, estimate that drug errors cause 700 deaths a year and could also be a factor in between 1,700 and 22,300 other ones.
Ø 237 million drug mistakes are made each year
Ø 28% could cause moderate or severe harm
Ø 22,300 more deaths could be related to mistakes
Proposal
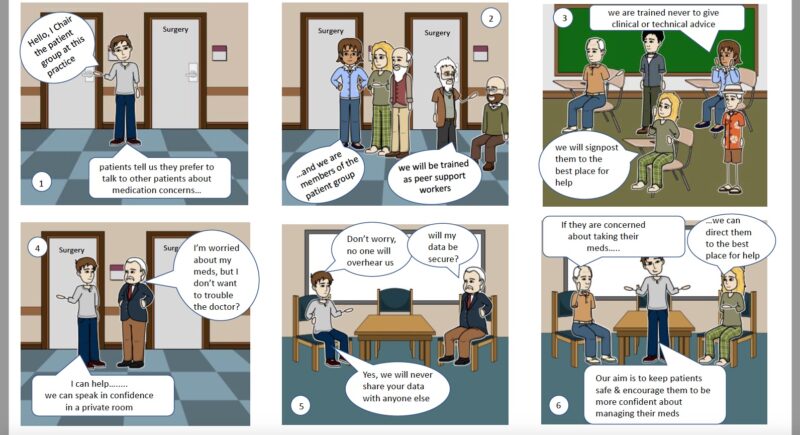
Our proposal is to obtain funding for a pilot study to assess feasibility of this peer support initiative to reduce harm by misuse of medication.
A rapid review commissioned by the Eastern Academic Health Science Network (EAHSN) in April 2018 revealed that there was little evidence about the best way to recruit and train peer support workers. In addition, only limited research has been done to compare the pros & cons of different types of training. An evidence scan commissioned by the Health Foundation in 2013, evidenced that patients were apprehensive about challenging and questioning clinicians about their medication and were more likely to talk openly about their fears and concerns to their peers. In line with the Royal Pharmaceutical Society’s best-practice guidance for medication optimisation, we propose an innovative approach to working with Patient Participation Group (PPG) representatives to help embed medication optimisation into clinical practice. The peer support workers will not give clinical advice, but will help patients understand the importance of taking their medication as directed. They will signpost them to access the most appropriate source of advice.
We intend to draw on the existing Medication Waste campaign, developed by Mid Essex CCG. We will integrate medication safety and waste, in order to optimise medicine use to achieve our objectives and health benefits. We will identify potential peer support workers from the PPGs with the right skills to coproduce the training programme. They will also develop a learning and support package, which will include informational leaflets, booklets and posters. Patients attending GP surgeries will be offered the opportunity to talk to a peer support worker and discuss any concerns about their medication. The peer support worker will not offer any clinical advice but will make an assessment of their level of knowledge and confidence about their medication. They will then be signposted to appropriate services if necessary e.g. pharmacy for Medicine Use Reviews and practice Nurse Prescriber etc.
Benefits
- Reducing harm caused by misuse of medicines
- Promoting shared decision making and understanding medication risks & benefits
- Enhancing patient experience and empowering patients to better manage their condition
- Avoiding waste and improving cost efficiency
- Contributing to the learning and benefits of peer support through empirical evidence
- Developing and testing methods of measuring the effectiveness of peer support and coproducing effective tools for training peer supporters
- Reducing demand for GP appointments and pressure on services
A full evaluation report and robust recommendations will inform and develop the campaign, which will be tested with the PPGs, before campaign launch. A medication safety toolkit will then be developed which will also include the key materials required to support the peer workers. The PPGs at selected GP Practices will be involved with co-designing and developing the campaign, which they themselves can deliver. The pilot will explore optimum measurement criteria e.g. qualitative questions and POET/PAM/Wellness measures.
Further Benefits
- It embeds patient views and involvement at the heart of the campaign
- It promotes NHS values and objectives
Collaborators / Partners
- Eastern Academic Health Science Network will provide guidance on governance and improvement methodology
- NIHR Collaboration for Leadership in Applied Health Research & Care (CLAHRC EoE)
- Mid Essex CCG (TBC)
- Cambridge & Peterborough Foundation Trust, expertise in peer support, training and evaluation (TBC)
- Paula Wilkinson, FRPahrmS, Chief Pharmacist & Deputy Director of Primary Care, NHS Mid Essex
- COPE (Scotland)
Challenges
Over the course of several workshops, members of the Citizens’ Senate identified the most common risks for causing patient harm in primary care, particularly improper use of medication and poor knowledge about their medicines. This was consistent with findings published by researchers in 2018 from Manchester, Sheffield and York universities.
Benefits to the Q Community
The project will build on the findings from the first Q Improvement lab, which explored ways to make peer support available to all. The initiative will provide evidence about the best way of utilising a structured and formal peer support model to empower patients and increase their ability to self-manage. The programme is replicable and can be modified to reflect locality needs, as Sustainability & Transformation Partnerships (STP) and commissioners integrate primary and social care. The benefits and lessons learnt will be shared with the Q Community to promote more widely. We intend to publish our progress and challenges through webinars, QSIGs and Q events for easier learning, adoption and spread.
Resources
InvolvingPatientsInImprovingSafety
Training peer supporters – rapid review
Brainbox report final July 2016
Meet the team
How you can contribute
- Does anyone know of any research evidence in primary care that informs models of peer support in medicine safety?
- Is there any expertise or advice you can bring to our proposal?
Further information
Peer Support OutlinePlan v1.3 Aug 2018 (PDF, 806KB)
Reviewer feedback
This is a great project because…
The team propose an interesting way to use peer support in this important area of patient safety. It is well linked into national initiatives which should help it have wider impact.
By the time of the event we encourage the project team to think more about…
This is an exciting proposal and we are interested to see whether the concept actually works! It is ambitious for the amount of funding so there will be need to be a clear focus on how the project is delivered and making sure the learning is captured as it progresses.








Comments
Hilda Campbell 8 Jun 2018
Hi Sarah
Super, I am pleased it was helpful and am sure Volunteer Edinburgh will be too as they want it to be taken up by others. It is good to share as none of us can do this alone, but working together then I believe the change can happen :-)
Hilda Campbell 12 Jun 2018
Hi Trevor
Would be happy to join a conference call in future, if that's helpful. My direct email is hilda@cope-scotland.org if you want to send me some potential dates for us to chat. Think that's what is great about Q there are so many pieces of work going on all over UK we can share, saves having to start everything from scratch as we can build onto what already exists :-)
Sarah Rae 8 Jun 2018
Thanks, Hilda. I've just started checking out the Volunteer Edinburgh series of Good Practice Guides. It's hugely helpful to have access to these resources for our type of project. The advice will help us to consider and plan for some of the issues we might have overlooked when involving volunteers. Thanks again for flagging up this website and providing your support. .
Hilda Campbell 5 Jun 2018
received this email, not sure if info of use?
Volunteerwiki
For many years Volunteer Edinburgh has made available a series of Good Practice Guides on volunteer involvement and management on their website. Initially working with colleagues at Volunteer Glasgow to update the guide content, they have now, in their own words, dragged the guides firmly into 2018.
Based on the Wikipedia platform that you are all probably familiar with, this new tool will enable them to provide quality information on involving volunteers in a flexible and evolving way.
Using the ‘wiki’ model gives better flexibility and articles contained within the wiki can be as short or as detailed as needed, links can be made between articles and downloadable resources have been included, with more to follow. This launch really is only the start. Volunteer Edinburgh's ambition is for this to build into the “go to” place for good advice on involving volunteers.
While this is a Volunteer Edinburgh product their ambition is that it becomes much bigger than them. To encourage maximum use by other agencies it has been given it a unique URL www.volunteerwiki.org.uk to which people are welcome to link to from their own websites. Additionally the Volunteer Edinburgh branding has been kept deliberately minimal to allow it to grow and to encourage contribution from other trusted sources.
We at VAF wish them every success with this and hope that you can make good use of the resource and contribute where you can.
Trevor Fernandes 11 Jun 2018
Hilda, I agree with Sarah, this will be extremely beneficial to our project. I didn't know about Volunteer Edinburgh - I'm realising how little I do know!! The info will help us develop best practice for our Citizens' Senate volunteers, not just for this project, but other improvement activity too. Once we get our AIMS application finalised and submitted (by 20/6) we should organise a conference call, assuming your availability? It would be worthwhile obtaining your advice & guidance on the detail....
Thanks once again.
Hilda Campbell 4 Jun 2018
Hi
I just wanted to pick up on the point of Risk. Recognising what maybe a challenge, isn't a reason not to do it, which i think we all agree. In fact, Risk assessing the process is essential for any new piece of work as once assessed the risk you can then look at how to manage it. When I was in general nursing, it was routine, if anyone was on Digoxin, we checked their pulse before administering their medication. The number of people I spoke to since working in the community, who were on Digoxin but didn't check their pulse, nor totally understand what Digoxin did was interesting, this included people caring for an older relative. Often people didn't know how to check their or another's pulse (First aid courses aimed at helping people acquire skills for improved self medication management is perhaps another area for development? We invested in baby/children first aid for parents and it was really popular, just an idea.....run by St John's Ambulance). I recommend people or someone caring for someone on Digoxin speak to their GP, practice nurse or other health care provider and offer if needed to make that appointment, so they could get more advice. You don't scare the person, you simply share its a good idea and something they should learn and people are okay with this I have found. NOW you are not advising the person to not take their medication if their pulse is low, you are educating the person what to do to take Digoxin safely and if they think their pulse is low who to contact, you are not saying don't take it, just making people more aware. Now its over 30 years since I worked in general nursing and I no longer directly support people so I know new medications are on the markets and Digoxin maybe prescribed less, I share it as an example of where a peer supporter could be useful to someone e.g. person on Digoxin loathes needles so avoids regular blood tests, a peer supporter could help person understand importance of the regular blood test, maybe go with person and afterwards go for a nice cup of tea or something so person is more likely to keep appointment as has support. Yes there are risks with anything new, but there are also risks when we do nothing, so its finding a way to manage the risks and trust that people with support can learn more about self-managing their health and that peer supporters are a crucial part of this journey for people. So while Peer supporters would not offer advice on medication, they would need an awareness of some of issues so they could share with person why they need more info from GP, or practice nurse or community pharmacists. E.g. their are some foods and medications don't mix. E.g. if person on MAOIs (Monoamine Oxidase Inhibitors) they need a diet which is low in Tyramine, now if person loves a pepperoni pizza with extra Parmesan cheese washed down with some beer, and don't feel the day gets off to a good start without a roll on bacon, then they are most likely going to run into some serious health challenges very quickly. Again MAOIs are prescribed less now, but I share this as an example of risks people can take if they don't understand why they need to take precautions on certain medications. Peer supporters don't offer advice, they re enforce the message the health professionals have shared and help person seek more advice from a health professional if they need it. Even something like sunscreen, people can overlook. Yes there are risks with peer support, BUT, I think we have enough skills and experiences to draw on from all those who have shared ideas to find ways to reduce the risk and to recruit, train and support a group of people who could make a real difference in the lives of others, and maybe even improve their health outcomes. There are so many areas e.g. someone starting chemo, yes there are professionals who offer support, but speaking to someone who has came out the other side of the chemo journey have a unique perspective e.g. asking for the speed to be reduced on the IV as hurts your veins less, or ask staff to put your hands in hot water as makes easier for cannula to go in, or things to do at 2am when your arms hurt so you can take your mind off it and keep going with the treatment when you really want to stop. People with lived experience are experts too, remember peer supporters are a group of experts to be enlisted to help people make the most of the medication they are prescribed. Just sharing some thoughts, we do need to consider all risks, including the risk of doing nothing, then take our time to put things in place to reduce risk
Have a lovely week all
Hilda
Wasim Baqir 3 Jun 2018
Hi Team
This is a really good initiative. Patient involvement in decisions about medicines is key to ensuring that medicines prescribed are used (not wasted) and that we don't 'force' medicines on to people. I would suggest that there is a link in this project to the prescriber.
Also, have you seen the THINKSAFE work done by Professor Thomson et al - http://www.thinksafe.care/file.aspx?id=48 ?
Good luck.
Hilda Campbell 6 Jun 2018
Hi Wasim and Trevor
I was wondering, are you aware of the realistic medicine work in Scotland? http://www.gov.scot/Publications/2018/04/6385/4 , there is a section of interest The Imbalance of Information
The gradient of power and knowledge imbalance between patients and clinicians needs to be recognised and its implications understood. Often the choices are not straightforward. When people are making decisions about treatment options with a serious condition, they may be frightened and vulnerable; at the time they may seek to be guided by the doctor. It is afterwards that they may question the merits of the treatment decision or experience regret, if their expectations are not met.
This is another occasion perhaps where having time with a peer to reflect on what the doctor has said, think about the questions the person wants to ask, make a list of points they want to cover then go back and speak to the doctor again. There is also the point of 'health literacy' again something we are looking at in Scotland. For people to have meaningful,confident conversations about their medication and condition, they need to have a level of health literacy otherwise the person may feel overwhelmed, agree to whatever is being offered, but not really understand the options. Again, someone in a peer support role can act as a bridge to support the person to have meaningful conversations with their health team about their medication and any challenges to compliance e.g. some medications require you to eat something first, then wait so many minutes, some people are using foodbanks so don't always have food, and/or, don't have a watch or clock, or maybe confused so forget the timing. If they are on many medicines all being taken at different times, and different times of the day, chances of issues arising are higher. Having that peer support means a person maybe more likely to share the real life challenges they have to complying, so they can then feel more comfortable to come back and speak to their medical team about how realistic the chances are of them doing what has been prescribed. Part of realistic medicine is also about asking the right questions, and again, I see links with peer support to ask those questions, this is another extract from the paper: Asking the Right Questions Matters
To help ensure you have all the information you need to make the right decisions about your care, please ask your doctor or nurse:
Is this test, treatment or procedure really needed?
What are the potential benefits and risks?
What are the possible side effects?
Are there simpler, safer or alternative treatment options?
What would happen if I did nothing?
NHS Borders, Lanarkshire, Forth Valley, Borders and Dumfries and Galloway are all piloting the 5 questions and we encourage the remaining Boards to follow suit.
Evaluation of the 5 questions approach is under way so that we can understand their impact on patient care and determine how useful they are.
One role for peer support could be encouraging people to ask these questions and promoting prompt cards
kind regards
Hilda
Trevor Fernandes 4 Jun 2018
Hi Wasim, thanks for your helpful & encouraging comments. You are right, there is a link and we have seen evidence of errors in prescribing and dispensing, but we want to keep the scope quite tight, to make it achievable. So focusing only on the peer support model. Yes, I have heard of ThinkSafe, but will have another look at the link.
Thanks once again
Trevor
Sarah Rae 2 Jun 2018
Thanks, Hawys. You’re right, we’ve thought long and hard about the issue of peer workers giving advice and patients receiving mixed messages/being misled. A large part of the peer workers role will be sign-posting to community resources and making suggestions, such as telling patients about medication reviews etc. However, it’s still a risk which is why the subject was given a lot of careful consideration when we were brainstorming our AIMS application yesterday. One of the safeguards we’re going to put in place is to have a dedicated peer supervisor who will offer the peer workers support and supervision. They will be briefed and get ongoing feedback on this issue. We will also factor in reminder sessions and training reviews for the peer workers.
In addition, we plan to find out how others how have dealt with this problem, such as the Recovery College East which as you know delivers accredited training to peer workers. Luckily, Hilda Campbell who is CEO of COPE Scotland, has joined our project team. Hilda has a huge experience from the work she has done with an organisation which is led by the voices of lived experience. She's already shared some very useful documents with us, such as a confidentiality agreement, supervision policy and code of conduct as well as giving us advice on costings.
Going forward, we aim to get confirmation from GPs re: the parameters they are comfortable with. We should also be able to gain info/feedback from a survey which asks patients about the scope and extent of the advice they received.
Karen Machin 5 Jun 2018
Hi Sarah, I'm interested that your reply has moved from 'peer support worker' to 'peer worker'. Is this because their role is moving away from the mutuality and reciprocity of true peer support, to one of signposting and advice?
Hawys Tomos 31 May 2018
Great to see your peer support bid here – and that it’s drawing and building on some of the Q Lab work. You’ve pulled together some excellent resources too, which are really interesting to read. Thank you for sharing the rapid review.
I would mirror Hilda’s and your own concerns about ensuring that there are very clear guidelines and training in place to ensure safety. One of the things that came up multiple times during the early research interviews (I’m pretty sure we even spoke about it, Sarah) was specifically about medication discussions on online peer support groups and how there are sometimes blurry lines with regards sharing personal experiences of medication versus giving medication advice. It might appear to be a clear-cut division; however, I have heard a doctor explain that some advice might be useful to come from a peer if the risks outweigh the benefits – for example, advice on how to correctly use an asthma inhaler. I would suggest this is worth considering, and if there are exceptions where a peer might be empowered to give advice, this should be very clearly defined.
It’s clear that you’ve already given this topic a lot of thought, as Trevor mentioned that “this is an area that will be covered during the training, which will also include role play and developing appropriate scripts” and Sarah you mentioned it would be “explained at the start of the recruitment process and reinforced throughout the course” as well as partnering with another organisation that expertise in this area. I was wondering if you’d also considered longer-term reinforcement of this message or moderation of working practices, after all of the initial training is completed? We can all fall into bad habits over time, so having some ongoing training or occasional peer moderation might be something to consider, for example? I believe recovery college East hold alumni events for graduates of the peer education programme, that allowed peers to support each other, voice concerns and brush up on training.
I look forward to seeing how this develops!
Trevor Fernandes 4 Jun 2018
Hi Hawys, you raise some interesting points about sustainability, some of which we have discussed during the early question 'is this idea worthy of investment & effort to improve medication safety'. If a successful model for peer support does emerge, we would consider an ongoing programme which could be picked up by the CCG, for example...
Regarding risk, this is an ever present encumbrance in our health service. Simply, we need to balance risk with benefit. The statistics highlight the extent of harm caused by medication errors, which goes a long way to justify taking the risk. Our plan will further mitigate risk by thorough training and supervision, together with measures we have already mentioned to manage the risk. If we do nothing, we will never improve the quality of care for patients and we will never become agents for change.
As a heart failure patient, I have seen many lost opportunities to improve quality of life, because of an over cautious attitude to risk. This is understandable, given the prevailing blame and liability culture which seems to have infiltrated the NHS over the last 20 years. However, from a patient perspective, we sometimes feel the risk is worth taking. It takes courageous decisions & actions ( to coin a phrase!) to overcome this culture - and it is starting to happen!
You may remember the Accelerated Access Review commissioned by the Government in 2016? I was just one of a number of patient representatives who worked on the report and subsequent recommendations. Whilst the review was primarily about exploiting emerging technologies and innovation to create a faster pathway, observations were made about our approach and attitudes to risk. The AAR recommended relaxing business rules and taking measured risks, rather than being over cautious. The report recommended deferring to ALBs, specifically to remove decisions from the NHS and not distract them from their core function. Clearly the more agile business organisations and partners, such as AHSNs and NIA will manage risk such that adoption and diffusion of innovation is prioritised and streamlined.
We are informed by overwhelming evidence to show that peers support in the context we are considering, is beneficial. The Brainbox report highlights empirical evidence that patients are more likely to respond better to fellow patients, for various reasons. Insights from Q Lab study also states ' all those who responded agreed that peer support is mutually beneficial and can be condition agnostic' - and ' there is growing evidence of the economic benefits of peer support and its wider social value'. Further evidence from the most recent Q Lab essay regarding peer support, state 'one in five people have used it to manage their health needs as people tend to place more value on something if they know other people do too'
So given the extent of harm caused by medication errors, together with overwhelming evidence of the benefits of peer support, together with our measures for mitigating the risk, we feel this idea is worthy of investment and our effort.
Sorry for the long read...
Trevor
Sarah Rae 30 May 2018
Thanks, Barbara. Trevor and I are convinced that peer support has the potential to help older people to have a better understanding of the importance of correct medication usage. We were strongly influenced by members of the Citizens' Senate who have experience of living with one or more long term conditions. They highlighted key concerns many of which are supported by research. Their suggestions for avoiding patient harm have shaped our ideas and helped us to develop this person centred approach. In fact, only last week the Pharmaceutical Journal reported on a study which investigated medication harm in older adults following hospital discharge. ('Medication-related harm in older adults costs the NHS £400m each year, study finds' https://www.pharmaceutical-journal.com/news-and-analysis/news/medication-related-harm-in-older-adults-costs-the-nhs-400m-each-year-study-finds/20204894.article) The authors concluded that there was “considerable scope for improving patient safety"
Barbara Hercliffe 22 May 2018
anything we can do to enable people to be more confident and able to manage their own medication has got to be positive particularly for the older people who often are confused. Developing peer support and information for older people in the community is an interesting concept to support people in their own home environment to better understand their medication.
Tim Bryson 21 May 2018
I think that this is such an important patient safety project. When I was working as a director of nursing, many incident investigations showed that patients needed to be much more involved in decision-making about their medications, and in giving feedback on how these were affecting them. This intervention would help through peer support in gaining awareness and in gaining confidence to play an active part in this way and to make it more likely that professionals will listen and respond. It is a vital aspect of enabling people towards self-management and being in charge of their own recovery.
Hilda Campbell 22 May 2018
Hi Tim
I think that is a point well made. If people are to have more confidence and support to self mange their health, then its important that understanding and being involved in decision making around medication is part of this, and where people need support to have those conversations with health professionals Peer Supporters can act as a bridge to support those conversations. One of my roles many years ago was supporting people who had been in hospital for many years to prepare to live in the community, a big part of this was around self-medication; as for years, people had received their medicine from the trolley. Part of this was helping people understand why they took the tablets they did, also what potential side effects there were to watch out for and report, also to discuss how easy the person would find complying with their regimen. We also had an excellent psychiatrist and pharmacist who worked with people to look at what medication best suited their needs and times and doses which made self medication easier for people. This was almost 30 years ago, but its interesting, even back then, we had residents meetings and tapped into the voices of lived experience for people closer to discharge to reassure people who had just came into the rehabilitation unit that their opinions mattered and people would be listened to. If we work together all sharing our experiences, including the voices of lived experience, then we can I believe, create better systems for people which are even more effective
Karen Machin 21 May 2018
Thank you for sharing the rapid review of peer support training, which I'd not come across before. We've trained several hundred peer supporters over the last nine years, but haven't written up all the anecdotal evidence from across England.
In mental health, medication is a difficult topic where people have very strong views. We have noticed that peer support can enable people to have conversations with prescribers. Just having a peer supporter alongside someone can give them the confidence to ask questions and make changes.
Karen Machin 23 May 2018
Hi Trevor - one of the organisations I work for is the Institute of Mental Health in Nottingham where we have a peer support module that is validated by the Open University. We've been delivering that training since 2009 so I've worked with many organisations and hundreds of peer supporters, both paid and voluntary. We also offer team readiness, support with recruitment, supervision and refresher masterclasses, to give a full package of support to organisations who want to implement peer support. We've worked across sectors - including peer support within the police force and for university students, as well as organisations in both voluntary and statutory sectors who are more directly related to mental health. We recognise that this offers us continuing learning opportunities and we share that learning with future cohorts. Hope that helps - but do contact me if you want more information.
Trevor Fernandes 22 May 2018
Karen, thanks for your comments. Really interested in your training regime for peer supporters. Which organisation/dept and what area of work are you in? Are your peer supporters volunteers or paid?
Sarah Rae 21 May 2018
Hi Hilda, thanks for your support and encouragement. I just wanted to pick up on the important point
you raised in your first post re: peer workers not providing advice about
medication. This would be explained at the start of the recruitment process and
reinforced throughout the course. I was involved in a 3 year psychiatric
medication management pilot which was run at the Cambridgeshire and Peterborough
Foundation Trust. One of my roles was to deliver training on shared decision
making to Care Coordinators. I always emphasised that they could support patients
to make decisions about their meds, such as providing suggestions about the
type of questions to ask their psychiatrist but never to offer advice about
what meds to take/not take. We’ve already given this some thought and would
like to partner with an organisation that has expertise in this area. Eg the
Recovery College East which runs an accredited training course for peer workers
locally. A whole day is devoted to SDM to ensure the students understand their
role. Over 40 peer workers are currently employed by CPFT and I’ve not heard of
any poor practice. Thanks too for your offer to connect and for letting us know
about COPE. Kind regards, Sarah
Hilda Campbell 21 May 2018
Hi Sarah
Thanks for that additional info, I really think you have a great idea, have sent on the Brain Box report to local GP cluster lead and shared with them exciting work you have planned as think it would be great to have a pilot we can all learn from then look at adopting and adapting.This is what makes the Q Community so valuable as it provides a way to connect with people we may otherwise never meet, and be able to share ideas, challenges and solutions
I hope your idea is funded and look forward to learning more
kind regards
Hilda
Trevor Fernandes 20 May 2018
Dear Hilda, this is really insightful and informative – and much appreciated. You have covered some of the issues and challenges raised during our patient workshop sessions – so we must be on the right track! You have also given us food for thought…. We would welcome any suggestions and/or contribution from your primary care colleagues to review our proposal, or to inform our pilot study, if you have experience in this area?
The important distinction between our proposed model and the ones you mention, is that we are focusing purely on peer support for optimising the patient’s medication only, rather than supporting the condition. Well-being, quality of life, waste, cost efficiencies and self-management are the benefits here.
We are aware of the condition specific peer support groups that you highlighted and there is a role to play in the wider social and primary care landscape, however peer supporters in this environment tend to be ‘paid workers’ and are integrated with current services for specific conditions e.g. cancer, diabetes, MH etc. Initial views from patients involved in support groups, suggest this area is quite well covered, although it can always be better. Also, in some areas there is additional risk due to radical transformation driven by STPs, whilst commissioners struggle just to provide day to day services. This is certainly an area that may be a natural progression for our model, at some stage in the future and as GPs confederate.
Our proposal is unique (we think!), in that it utilises voluntary peer supporters from existing GP practice PPGs. They will operate in a ‘contained’ and safe environment within the practice, which will be relatively stable and where there will be plenty of support from health professionals. Yet, we want to introduce a more formal structure to the model, so that we can measure and continuously refine and improve. Our aspirations are to develop a model that is replicable. Having said all that, we are cautious that objectives may be too ambitious, although the next steps and direction will be informed by the pilot study.
There have always been concerns about peer support workers giving advice, rather than assessing and signposting, so this is an area that will be covered during the training, which will also include role play and developing appropriate scripts. However, each patient is different and the training will focus on developing peer support worker’s assessment skills to determine the level of understanding and confidence the patient has about their medication regime. Pilot studies for the Medication Optimisation campaign in Mid Essex have indicated a positive risk/benefit outcome – but the proviso is that peer supporters are properly trained (see Brainbox Report). There will be no clinical advice given and we will be supported by the pharmacy and nurse prescribers.
The A key finding in the attached evidence scan, ‘Involving Patients in Improving Safety’ is that patients may feel more comfortable when they do not need to speak directly to a health professional about their concerns – patients do not want to appear to be challenging professionals or to be seen as difficult. This is consistent with the ‘Brainbox’ report which indicates that patients are sometimes intimidated by the health professionals and do not know what questions to ask. They are worried about looking foolish and would rather just get on with it. The East of England Citizens’ Senate workshops have also identified patient concerns about similar medication safety, so we believe the evidence is overwhelming and there is a huge gap here to fill by developing a voluntary peer support model to improve patient safety around medication.
In the former report, ‘Involving Patients in Improving Safety’, the most evidence is available about initiatives to help patients take an active role in their own safety (34 studies). Examples include educational leaflets, videos or posters to help patients feel more confident questioning professionals about hand hygiene, for example, comment cards to help identify individual safety issues and encouragement to tell staff if the patient has any concerns. So, we feel our initiative will also play a big part in self-management, education and raising levels of confidence and awareness - some of the criteria you have also mentioned.
Thanks once again for your comments
Hilda Campbell 21 May 2018
Hi Trevor
Thanks so much for that reply, I think what you are proposing is really exciting and actually would meet some of the needs people expressed at our consultation, as although people said more time with a community pharmacist there is still some people who don't ''like to ask'', ''be a bother'', ''be seen as not knowing''. Having peer supporters is a way perhaps which will enable people to begin to have the conversations they need to have around asking for more help, or information.
I hope you are successful as this is a great idea and something I think we all can learn from as i think it could be rolled out. I am happy to continue sharing ideas on developments we are looking at around support for people in primary care and communities who have chronic but mild to moderate mental health issues, who often can find accessing the long term support they need a challenge. Also wider developments in primary care around community wellness. My email is hilda@cope-scotland.org and for more info on COPE Scotland visit www.cope-scotland.org
kind regards
Hilda
Trevor Fernandes 18 May 2018
Thanks Rob, appreciate your support. Can you login to Q and click on the 'support' button on right of our submission.
Robert Johnstone 17 May 2018
Hi Trevor
I can only endorse the need for this
Let me know if I can do anything to help
Robert
Nathalie Delaney 14 May 2018
This is a really interesting proposal -- are local community pharmacists involved? We've found the Local Pharmaceutical Committee super helpful in our region for linking community pharmacists into our safety work, particularly around the medication use review and new medicines reviews they carry out. Our colleagues over in Wessex AHSN also have a brilliant patient campaign called Meet Mo which would be worth checking out... http://wessexahsn.org.uk/projects/171/meet-mo
Trevor Fernandes 14 May 2018
Hi Nathalie, thanks so much for looking over our proposal, you raise a good point about involving the community pharmacist, I hope we have covered this. Paula Wilkinson is a member of our project team and will be providing advise and direction as we develop the detailed project plan. She is Chief Pharmacist and Deputy Director of Primary Care Mid Essex, so we will obtain sound advice. Once we clear all the hurdles, we hope to co produce the project implementation plan with the Pharmacy and Practice Manager for the chosen pilot site. I will definitely have a look at Wessex AHSN to see if we can draw on any synergies. Thanks once again.
Trevor Fernandes 13 May 2018
Thanks Anne, how often do we hear the same thing or similar. You are right, I think generally, the older generation don't want to bother anyone and will not always ask for help. Its ok if they have a partner/family who can help keep an eye on their medication, but some people don't have any level of support. We are thinking of providing a contact from each PPG, who will be a friendly and reassuring voice on the telephone, who can help direct them accordingly - or even arrange a liaison with the health professionals. However, we don't have this element included in our peer support model yet.
Thanks for your comments
Anne Crawford-Docherty 13 May 2018
A very interesting proposal. I can relate to the possible 'overwhelm' of some older adults with the amount and complexity of the medications they have to manage, as my 77 year old mother has to manage the meds for my step-father further to his kidney transplant and Wegener's Disease condition. They have huge parcels of medications delivered to the house, sometimes in medi-packs, but often need support to organise and feel confident in administering it, especially as meds change colour and shape from month to month depending on pharmacy stock. My parents are of the generation where they 'don't want to bother' the staff, so a peer they could contact and access to easy-read resources would be invaluable. I do think having a person as a supporter would add so much power to the project - I think clear information is only a small part of the reassurance required to manage meds and avoid errors.
Hilda Campbell 18 May 2018
Hi
I think this is an interesting proposal and well thought out. What I would add in support of this is recently we held a community consultation on the new GP contracts in Scotland, however, it became more a conversation around primary care services in general and how they could be reviewed. People were invited to think about what a perfect primary care service would look like. The participants were older adults, people with multi morbidity issues and people who suffered from mental distress. The feedback did included issues of medication, these are suggestions:
· More time with a community pharmacist to show how to take medication
· Make time so people feel more comfortable to say I don’t know how to do something e.g. use an inhaler, as if don’t use it correctly it won’t work, maybe ask pharmacy to show you, also have an appointment with pharmacist if complicated medication regime so you know how to follow it, don’t waste money having prescription end up not taking
· Self-management advice what else is there apart from tablets
people also wanted to see more peer support groups including:
More formal peer support groups being supported, linked to primary care, on common conditions, doesn’t need to be practice which facilitates e.g. have better inks with other bodies who e.g. offer support around arthritis to have peer support groups locally, everyone with that condition on GP list told of the group, ideas people had for peer support groups included:
· Diabetes
· Asthma
· Heart conditions
· Coeliac
· Depression
· Bi polar
· Pregnant parents
· ME
· MS
· Arthritis
· Autistic spectrum disorders
· Dementia and Alzheimer’s
· Diet and activity
I think there is a role in enabling people feel comfortable to ask questions and to say I don't know, and I think peer support can be a way for people to realise they aren't on their own, others have similar challenges. My only point would be and sorry if this is covered. Any group would need clear boundaries around medicine safety and medicine prescriptions. I have heard horror stories of people advising other people to stop taking medication, or commenting negatively on what another person's GP has prescribed, who have no formal medical training.
I am totally supportive of the essential value of lived experience in planning services and peer support, however, this needs balanced with the safety of ensuring people discuss any concerns about their medication to their GP, community pharmacist and don't seek advice from a lay person. The peer support is around encouraging people to say its okay to ask for more time for something to be explained.
It maybe the bigger issue for further discussion is looking at prescription patterns, can they be simplified, are there other things which can be offered. This would need the involvement of the relevant health professionals, but it maybe something for the future to think about.........Interesting piece https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2267940/ .....
Prescribing for older people
James C Milton,specialist registrar in geriatric and general medicine ,1Ian Hill-Smith,general practitioner,2andStephen H D Jackson,professor of clinical gerontology1
Kind regards
Hilda
Comments are now closed for this post.