Q Exchange
Get by with a little help from your friends
- Proposal
- 2024

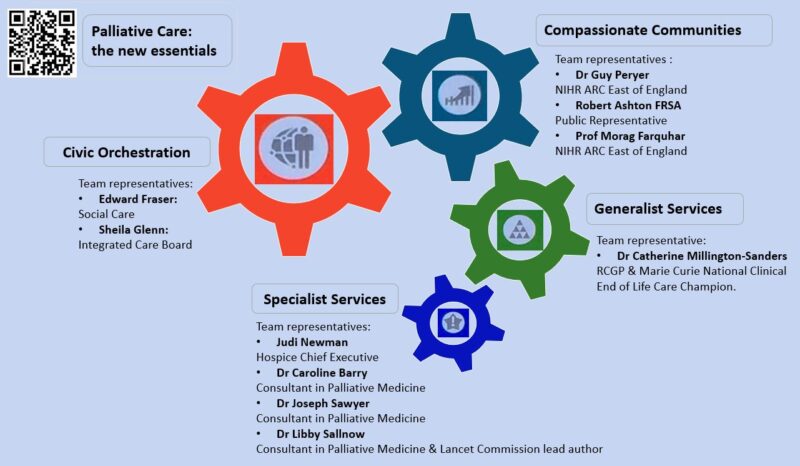
Meet the team
Also:
- Judi Newman (CEO, St Elizabeth Hospice)
- Dr Caroline Barry (Consultant in Palliative Medicine)
- Robert Ashton FRSA (Public Involvement Champion)
- Dr Caroline Millington-Sanders (RCGP & Marie Curie)
- Dr Joseph Sawyer (Consultant in Palliative Medicine)
- Professor Morag Farquhar (Professor of Palliative Care Research)
- Dr Libby Sallnow (Consultant in Palliative Medicine & Lancet Commission).
What is the challenge your project is going to address and how does it connect to the theme of 'How can we improve across system boundaries?
- Palliative and end-of-life care (PEoLC) are public health concerns. Demography suggests that more people will die annually over the next 15 years. It will place further pressure on depleted clinical workforces and strained statutory services.
- NHS England has adopted an ‘Ambitions Framework’ to improve PEoLC. Ambition six states: ‘Each Community is Prepared to Help’. If we do not increase levels of support in community settings we will see more, potentially avoidable, hospital admissions, more cases of carer exhaustion, and higher rates of disabling bereavement.
- This initiative will support Death Literacy learning capabilities across system boundaries.
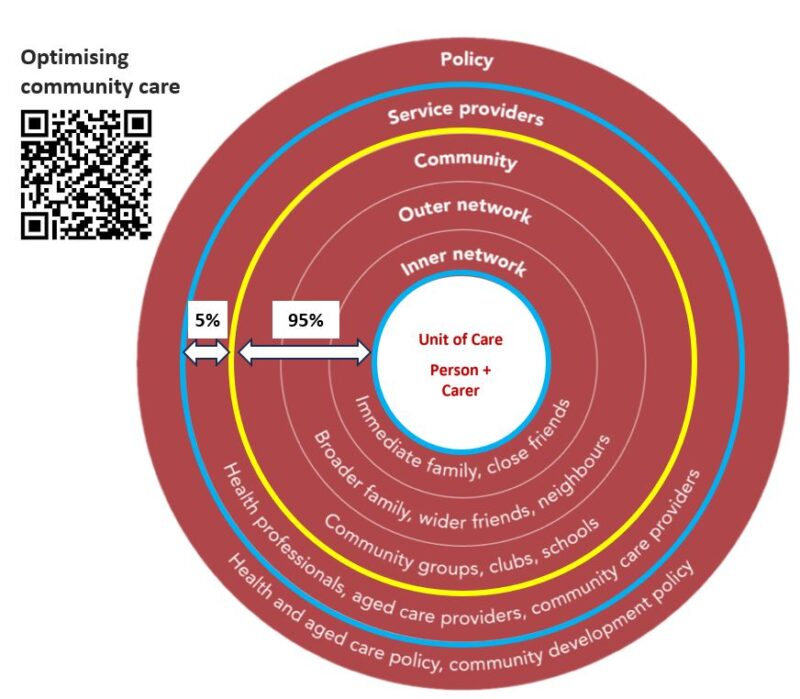
- Expanding community involvement in PEoLC will enhance the resources, connections, and benefits that individuals and groups gain through their social networks and relationships. This is where 95% of PEoLC occurs. Social comorbidities that often coincide with serious illness: loneliness, social isolation, anxiety, or depression can be prevented or reduced.
- We have, ‘one chance to get it right‘.
What does your project aim to achieve?
‘Gather my crew‘ is an established socio-technical innovation developed in Australia that creates a personalised support network for individuals and families experiencing serious illness. It provides a user-friendly platform to translate goodwill from supporters into active participation in practical tasks: respite care, household chores, transportation, and care system navigation. Supporters are invited to join a closed social network that ensures privacy and data security.
Objectives of ‘Gather my crew’ across five sites in the East of England:
- To engage and involve supporters who are familiar with a person’s unique PEoLC context.
- Provide educational resources to improve death literacy knowledge and skills for those included in the closed social network.
- Monitor interactions, and potentially fewer transfers, across care system boundaries.
- Identify support and care needs.
- Coordinate informal care tasks.
- Evaluate the innovation’s impact in meeting users’ needs and improving their wellbeing via regular ‘check-ins’ using Patient Reported Outcome Measures (PROMs).
How will the project be delivered?
- We have assembled a diverse team across system boundaries to enhance learning and share expertise.
- The project lead works within the National Institute for Health and Care Research Applied Research Collaboration. Co-applicants are situated in Social Care and Integrated Care. Additional team members include representatives from Acute Care, General Practice, the Hospice Sector, Palliative Care Research, and a Public Involvement champion.
- St Elizabeth Hospice is well equipped to be the host organisation; it has a reputable Compassionate Communities programme that promotes death literacy in the local area. Four other sites have requested participation: two hospice charities and two community-based social support hubs across Norfolk, Suffolk, and Essex. All families supported by their services will be invited to use ‘Gather My Crew’.
- Impact evaluation will be assessed using: regular well-being PROMs, staff interviews at all sites, Ripple Mapping, and participant reports exploring the frequency of GP appointments, and hospital admissions.
How is your project going to share learning?
Three strategic impact pathways are enabled by existing connections held by the project team:
- Regional: The NHS Strategic Clinical Network will be the first place to disseminate the findings. The network includes the six Integrated Care Boards in the region (overseeing >6.5million people), hospice partners, and members of the Citizen Assembly. This pathway can cascade the findings to NHS England and more local place-based and partnership boards.
- National & Q Community: The project lead will present the findings at the Health Services UK conference in 2025, and inform clinicians at the Royal College of General Practice via the ‘What Matters Most’ think tank. We will engage Q members via the SIGs, including the Systems Convening and Network Mapping SIGs.
- International: The project lead will disseminate as a council member to Public Health Palliative Care International (PHPCI). The team will also co-author an open-access article for a high-impact journal (e.g. Palliative Medicine).
How you can contribute
- We would appreciate any help and suggestions in developing our idea. What do you like about it? How could we improve it?
- We would also like to hear from local Q members who would like to join our team. In particular, General Practitioner Q members, and Health Economists.
- We would like to engage further with Q Special Interest Groups (SIG), in particular the Systems Convening, Network Mapping, and Network Weaving SIGs as well, as the Evaluation SIG.
- At the dissemination stage, we would like to produce a video of the project. We have a videographer in mind, but we would love to put a soundtrack to it as well. Are you a keen Q musician and would like to provide a score? Please get in touch
- We would also like to engage other Citizen Assemblies across the UK to share the results from our 'Gather my Crew' project.
Plan timeline
| 1 Aug 2024 | Contract approvals |
|---|---|
| 1 Aug 2024 | Ethics approval for service evaluation from UEA ethics committee |
| 1 Aug 2024 | Project steering group meeting |
| 1 Sep 2024 | First participants using the intervention in lead site |
| 1 Oct 2024 | First participants using the intervention in second site |
| 1 Nov 2024 | First participants using the intervention in third and fourth site |
| 1 Dec 2024 | First participants using the intervention in remaining site |
| 1 Feb 2025 | Project steering group meeting to discuss interim data analysis |
| 30 May 2025 | Final participants recruited across all sites (8 weeks data collection remaining) |
| 16 Jul 2025 | Presentation at Health Services Research UK conference in July 2025 |
| 1 Aug 2025 | Interviews commence with site leads exploring staff experiences |
| 1 Aug 2025 | Project steering group meeting to discuss data analysis and dissemination |
| 1 Nov 2025 | Project report preparation (3 months remaining) |
| 31 Jan 2026 | End of project |
Comments
Libby Sallnow 19 Mar 2024
This is an exciting and much needed project looking at two topics requiring urgent attention in palliative and end of life care - social networks of carers and people at the end of life, and the complex systems these processes take place in.
This project will provide really important insights about how networks function in practice and help people understand how to build them. It is a great example of what we advocated for in The Lancet Commission on the Value of Death. Look forward to seeing some of the results!
Guy Peryer 20 Mar 2024
Thank you Libby! We hope that you will accept our invitation to join the team. Your experience with the Lancet Commission and Compassionate Communities will be invaluable.
Sarah Yardley 15 Mar 2024
Great to see this idea here. I'd definitely be interested in seeing how it works out in practice and am particularly curious in whether you have considered boundary crossing between the so called informal and formal networks or crew - see Rosemary Leonard's work. As you know Guy, I am especially interested from my research in how we dismantle the ambiguous positioning of carers with respect to legitimacy and responsibility by professionals - always expecting too much or permitting too little! Let me know if I can be of meaningful use at all.
Guy Peryer 15 Mar 2024
Thanks for the suggestion Sarah. You're right, Rosemary Leonard has been a pioneer in considering social capital in the context of the Compassionate Communities movement. It was Rosemary's work that I first learned about the importance of social network mapping. Having recently gone through two very different experiences with the deaths of my father and father-in-law I experienced firsthand what you're talking about: the interface between formal and informal networks of care. The reality for us was that we benefitted from support from periodic care visits from statutory services, a 24/7 phoneline in the final stages, and the support of our friends and neighbours (especially in the weeks and months leading up to their deaths). Service constraints meant that we were often left waiting for a home visit. It was during those times friends and family helped most. We also picked up useful bits of information from our friends by listening to their previous experiences and acting on their recommendations. In the words of my wife, "often you don't know what you need to know until you're exhausted and stressed out". Thinking about the 95% rule, if there is a structured platform to involve a friend who has offered their support to act on something you need - we feel it's worth exploring if it could make a significant difference to the experience of care, and system resource use across boundaries. If we can seek multiple ways to increase Death Literacy, we are more likely to see a shift in what the Lancet Commission describes as 'the value of death'.
If we can encourage more social network mapping to become a routine exercise, there is more likelihood to engage informal networks of support where they are available. For people who do not have robust means of informal support - through a mapping process - it may help identify support needs from services.
I hope we can keep in touch about this as your take on the implementation of this project would be really helpful. Thanks again.
Morag Farquhar 15 Mar 2024
This project could enhance support for unpaid/family carers who provide the majority of PEoLC at home by helping them better navigate EoL care experiences for both themselves and those they support. Very happy to contribute if helpful.
Guy Peryer 15 Mar 2024
Thank you so much Morag. I have read about the Carer Support Nurse initiative you lead: https://www.ecch.org/news/posts/carer-support-nurse-service-wins-nhs-parliamentary-award/
Thinking about interface and improving care across system boundaries we would value your contribution to the team. I look forward to working with you.
Joseph Sawyer 13 Mar 2024
This is a fantastic idea and something that can make a huge difference not just in the short term but also in contributing to cultural change that is needed to reclaim death and dying as socially mediated and spiritual processes.
I would be particularly interested in how establishing networks like this helps build death literacy at a community level. Ripple effect mapping might be an interesting method to try and demonstrate how and if this works? It may spawn more research into barriers and facilitators to collective accumulation of death literacy.
Always interested in how responsibility and accountability is negotiated and how processional services work at this interface. Would be really interested in talking more and contributing to this work, well done on taking the initiative and moving things forward!
Kind regards, Joe
Dr Joseph Sawyer, Consultant in Palliative Care, PhD in Public Health approaches to Palliative Care
Guy Peryer 15 Mar 2024
Wow, yes please Joe.
I've read some of your publications in this area. We would love to welcome you onto the team. I think your idea of ripple effect mapping is a really good one. I know through NIHR ARC connections that the team in the West has some great learning resources on this. It seems like it would be a great way to engage and visualise details that can't be anticipated ahead of time. I'll be in touch. That's again for your support.
Joanne Smithson 11 Mar 2024
Very happy to have a chat. We’ve done quite a bit on wellbeing at the end of life https://whatworkswellbeing.org/resources/supporting-employees-with-terminal-illness/#:~:text=As%20there%20is%20no%20quality,Consistency
Guy Peryer 15 Mar 2024
Hi Joanne,
I was looking at the link you sent - so helpful - thank you. I'd love to talk about this more with you. I especially liked this part on the 'what works for wellbeing' site viewed from a 'friends and family' perspective.
Three principles for effective action:
Compassion
Communication
Consistency
Hilda Campbell MBE 4 Mar 2024
Wonder have you heard of the 'Death Cafe's' https://deathcafe.com/
''At a Death Cafe people, often strangers, gather to eat cake, drink tea and discuss death.
Our objective is 'to increase awareness of death with a view to helping people make the most of their (finite) lives'.
A Death Cafe is a group directed discussion of death with no agenda, objectives or themes. It is a discussion group rather than a grief support or counselling session.
Our Death Cafes are always offered:
- On a not for profit basis
- In an accessible, respectful and confidential space
- With no intention of leading people to any conclusion, product or course of action''
- Alongside refreshing drinks and nourishing food – and cake!
Guy Peryer 4 Mar 2024
Another great suggestion, many thanks. Yes, they're a useful addition to our local compassionate communities network. They occur throughout the year, especially during Dying Matters week in May in more prominent spaces. I also really like the 'departure lounge' initiative. https://acmedsci.ac.uk/policy/policy-projects/the-departure-lounge
Hilda Campbell MBE 3 Mar 2024
Hi Guy
My career has been spent working with people living with conditions to explore what matters to them and needs to change, then seeking to bring about that change. On a micro level this can often be achieved as there can be a lot of self determination around what next, how to use resources, develop ideas etc, however, on a macro level it can be hard to influence the larger systems to change and this is where issues can arise as people may want something that is not immediately available nor is there a clear route to make it available any time soon, or sustain it where it is there.......... how many great ideas go the way of the dodo sacrificed on the altar of the next new 'thing'
People may not have the time (Literally) to wait until the system changes, so part of any network needs to include what is possible what is achievable, what is desirable and pathways for each. Integration offers opportunities however, in my experience often statutory bodies need time to work out how to work together, then think mmmm how does this link with the third sector and community groups, then how does this involve (In a meaningful way, people receiving services............ lived experience groups are helpful, but often they have access and an influence the wider population never experience, so how do you make a system responsive to everyone's needs and not just a select few, whose opinions are valuable but it is not the same as a service led by the needs of those who use it, right from new referral what are people looking for, what do we offer, who else do we need to involve, what needs to change, how do we get feedback from people about how we have helped them achieve their goals/do we even take the steps to work on identifying what they are, or, do we respond with a pathway already pre determined which the person then needs to fit into ?
Happy to have a chat if helpful, my direct email is hilda@cope-scotland.org
Kind regards
Hilda
Guy Peryer 4 Mar 2024
Thank you Hilda. I appreciate your response. I'll certainly be getting in contact.
In reading your message I'm reminded of the 95% rule that drives the compassionate communities movement. If you are living with a life-limiting illness in a community setting you may come into contact with services up to 5% of any day. Ideally, in thinking about system boundaries we need to think about where the greatest amount of caring happens and by whom. I agree with your comments about services. I also see the need for increasing what the Australian team has termed death literacy and working in schools, workplaces, and across all sectors of society to equip people for what is on the horizon for us all. I like Alison Bunce's description of compassionate communities. "It's ordinary people looking after ordinary people." We saw glimpses of what can be achieved in terms of social capital during the pandemic, but in the wake of it the level of uncertainty seems to have set us back [I liked this report on this: https://hdr.undp.org/content/human-development-report-2021-22].
In combination with providing people with opportunities to be more involved, like with Gather My Crew, and increasing public awareness over what to expect there is significant potential to reduce the prevalence of trauma, or at least ameliorate harm for the people who witness the death of someone they care about.
I really liked your comments around inclusivity and the importance of considering interface design between sectors. Lots to think about.Thanks again.
Saskie Dorman 2 Mar 2024
Great idea!
It will be really interesting to see how ‘Gather My Crew’ translates from Australia to the East of England. What kind of benefits people using it experience (whether the person themselves who is nearing the end of their life, or the people in their ‘crew’) - and whether there are people who find it harder to use for whatever reason.
Guy Peryer 2 Mar 2024
Thanks for the comment Saskie. You're so right, the data generated around user-experience and what features of the platform people choose to engage with most will be really valuable: e.g. coordinating care tasks, communicating and sharing tips as a social closed group, signposting to other means of support, navigating the care system as a group, the factsheets that are available to learn more about specific health conditions, practical care advice, or future care planning.
The platform can be managed by family, friends, or care professionals. Data from a range of users will undoubtedly help future iterations and support increased flexibility for localised approaches to implementation. The aim is to support autonomy so the person with serious illness and those involved in day-to-day care feel more in control of what is happening when and by whom.
Hilda Campbell MBE 1 Mar 2024
I have often thought that some of the ideas for network weaving could be used to help individuals create their own effective networks to support managing health challenges and improving quality of life, including end of life care. To date, my charity has not had the resources to explore this further so the work remains around wider networks as opposed to the individual. There are parts that cross over though and happy if helpful to discuss further. As the convenor of a SIG looking at tools and resources for network effectiveness and leadership I would also be happy for you to post and share ideas in that space to harness ideas from Q members. Let me know how I can be of service.
Kind regards
Hilda
Guy Peryer 1 Mar 2024
Thanks Hilda, that's so helpful. I'd love to talk with you further about some of the stories that have come back when families have been facilitated to optimise their own support networks. I'm as guilty as the next person in using the phrase "Let me know if there's anything I can do", which ends up never materialising into anything. This method helps people make a significant and sustainable contribution to help lighten the load. It's sometimes seen as soft. My personal experience is that without the soft stuff, the hard bits that go hand in hand with supporting someone with serious illness get even harder.
Comments are now closed for this post.