Q Exchange
AHP led ACRT saves time, money and reduces health inequalities
- Proposal
- 2024
What is the challenge your project is going to address and how does it connect to the theme of 'How can we improve across system boundaries?
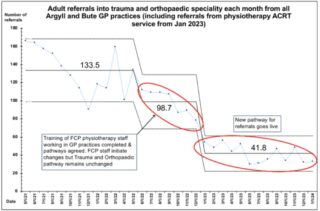
The accepted clinical pathway for orthopaedic services is a linear one from GP to consultant working in a siloed manner with tasks such as conservative management, imaging, injections etc. initiated one by one from consultant clinics, normally after repeated, prolonged waits. Active Clinical Referral Triage (ACRT) – a process ensuring that all referrals into secondary care services are triaged by a senior clinical decision maker to locally agreed, evidence based pathways can be managed better by AHP services working in partnership with orthopaedic services. This process has been implemented in A&B HSCP in partnership with NHS GG&C across health board and professional boundaries. This has reduced orthopaedic referrals by 69% and delivered a local, more timely service for patients. 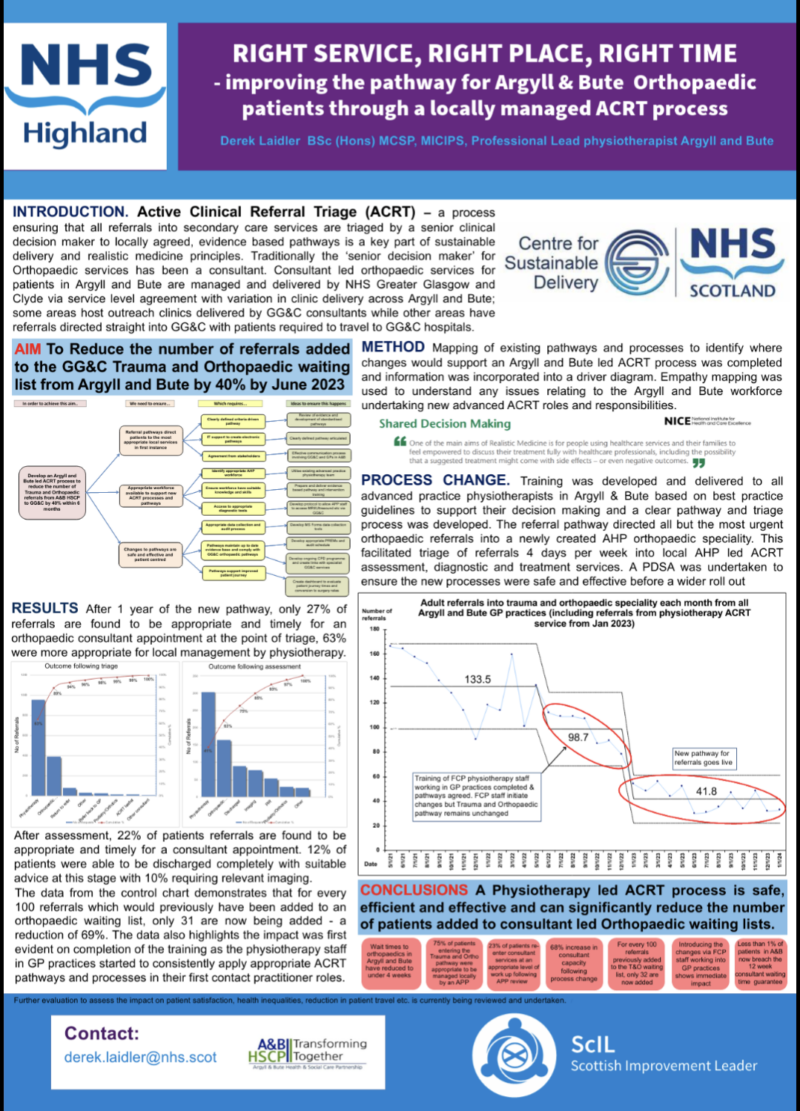
What does your project aim to achieve?
The project has demonstrated a huge reduction in consultant referrals but there is more work to do to improve and streamline the integration and expand the service to include other areas which could be undertaken by AHP services. The specific aims of the project are
- Develop a business case and training plan to include a locally led AHP fracture clinic service in collaboration with NHS GG&C orthopaedic services
- Develop an agreed collaborative process to support direct referral into NHS GG&C surgical waiting lists, reducing the requirement for consultant led clinics further
- Undertake further socio-economic and health-economic evaluation of the impact of the changed pathways on patient travel commitments, health inequalities and wider financial savings to support ongoing improvement and wider spread of the pathway
How will the project be delivered?
The project will be delivered by freeing up 2 days per week of dedicated time from an experienced clinician who has been involved in developing the work to date. Their QI support will be from myself and specialist evaluation input will be sourced from local HEI services.
Each element will be approached using the same QI methodology that was applied to the initial project.
How is your project going to share learning?
The project development has already been presented at a Q network event (Glasgow) and was well received. The steps required to replicated the pathway changes are readily transferrable and provide a clear model of collaborating across professional and institutional boundaries whilst incorporating a wide variety of key stakeholders.
the initial project has also been highlighted as an example of good practice by the centre for sustainable delivery in Scotland.
How you can contribute
- QI mentorship - I'm still relatively new to this
- Specialist evaluation skills/advice
Plan timeline
| 22 Apr 2024 | Scope of further evaluation completed - additional support sourced |
|---|---|
| 6 May 2024 | Scope of project finalised with driver diagram for each element |
| 27 Sep 2024 | Evaluation of initial project completed |
| 20 Oct 2024 | Proposal and plans for implementation of wider scope activities completed |
| 10 Nov 2024 | PDSA cycle for improvements/developments |
Comments
David Elder 18 Mar 2024
This is a great project. The work already undertaken shows clearly the impact this work can have. It would be really helpful if the next phase you are applying for could capture clearly the benefits to patients and overall savings (in time and cost) and insights to how easily this can be applied to other settings. The evaluation focus you suggest will be key to demonstrating this. Looking forward to hear how it goes.
Derek Laidler 19 Mar 2024
Thank you so much for your kind comments - yes I completely agree that we need a more rounded evaluation, what we have now is a simple framework and we have some basic data which, while positive, needs further investigation.
Michael Canavan 18 Mar 2024
Hi Derek, It's really heartening to see your commitment to build upon the improved orthopeadic referrals and apply improvement methods for sustainable change. Reducing waiting times and improving access are challenges which require a long-term approach and committed application of improvement methods. Wishing you the very best of luck and I will be very interested to watch your progress if successful.
Derek Laidler 19 Mar 2024
Thank you Michael for your comments - hopefully this is just the very start of our project which does now have some support from the National Centre for sustainable delivery. I'm confident that the methods we have used are easily reproduceable but you are correct that changing an accepted and long established process/pathway will required a continuous improvement and methodical approach with data to demonstrate value & I'm hoping this application will help me to achieve that. Thanks
Michelle Beattie 22 Feb 2024
What a good idea to use AHP expertise in this way and, ultimately, reduce patients wait. As well as reducing Consultants time it would be interesting to gather patients feedback of the service as well. It can be tricky to do a lot with 40K so I wonder if it would be more doable to develop and implement an agreed collaborative process to support direct referral into NHS GG&C surgical waiting lists for (specify condition/s) by then end of this project (?June 2025). I guess doing this could also inform a larger business case and test some measures for further funding around socio-economic and health-economic evaluation of the impact. Best luck and looking forward to hearing how it goes.
Michelle
Derek Laidler 23 Feb 2024
Thanks Michelle for your kind and supportive comments. Referring directly onto surgical lists for some conditions is already part of the new pathway and we anticipate that this will become widespread involving a wider range of conditions once GG&C consultants are reassured that our triage and patient management is 100% accurate. This sometimes depends on the views of individual surgeons and will probably be more evolution than revolution. What I am keen to explore if how we apply the current principles to some trauma services as well as the elective work we are doing and to have a really thorough evaluation and review of our current process and pathways so we can apply an informed continual improvement approach. I'd love to have a catch about the work and welcome any advice and support.
Comments are now closed for this post.