Q Exchange
Reducing Inequitable Delays for Procedures for Patients with Learning Disability
- Winning idea
- 2023
Meet the team
Also:
- John Harrison - Programme Director Clinical Service Strategy and Acute Sustainability Programme
- Gary Minto - Associate Medical Director for R&D
- Saoirse Read - Learning Disability/ and Autism Liaison Service Manager, Derriford Hospital
- Mark Hamilton - Chief Medical Officer for UHPNT
What is the challenge your project is going to address and how does it connect to the theme of 'How can improvement be used to reduce delays accessing health and care services'?
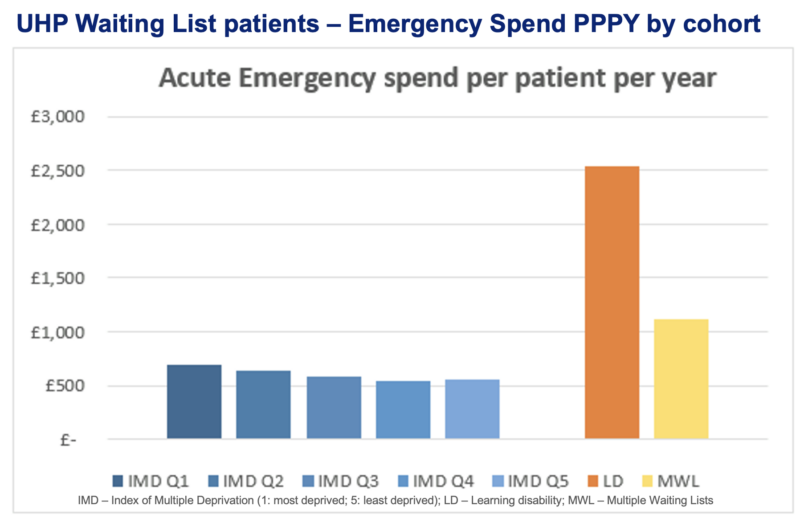
Patients with learning disability (LD) are a vulnerable patient cohort and face barriers when accessing care. At University Hospitals Plymouth NHS Trust (UHP), a recent project has identified that the LD population are experiencing differential access compared to the rest of the population. The data demonstrate that some are waiting longer for their required intervention with increased frequency of admissions to hospital while waiting for procedures.
This project aims to ensure the LD’s population access to surgical or medical procedure services at UHP is equitable. In addition, that the support provided to people with LD is tailored to support a reduction is avoidable access to non-elective care. This can be achieved by understanding the rationale behind differential access, and subsequently work with our relevant partners to develop a systems approach to reduce delays to elective care for the LD population as well as supporting them through a “waiting well” initiative.
What does your project aim to achieve?
The overarching aim of this project is to identify and reduce potential inequality in accessing medical or surgical intervention for the LD population.
Objectives include:
- Identify the rationale behind differential access to care that LD population may face while waiting for their medical procedure or surgical intervention.
- To improve their experience and reduce frequency of emergency admissions while on the waiting list as part of the “waiting well” initiative.
- Develop and implement operational interventions to reduce delays in waiting list for LD population. (extra procedural/ surgical lists, minimise cancellation rates due to unavailability of packages of care for patients with LD at the time of their attendance)
This project will bring positive impact to the LD population’s health outcomes, by enabling them to access the care they need and improve quality of life by reducing the need for admissions.
How will the project be delivered?
Identify rationale for differential access
- Engage with patients with LD, LD support team and service lines to identify reasons for delays.
- Scoping review to understand the barriers of access to care
- Subgroup analysis – Index of Multiple Deprivation
Reducing Delays
- Implement an operational approach to improving equality for the LD patients (e.g. integrate existing priority coding or creating bespoke lists)
Waiting Well Initiative – intervene earlier and provide care at the earliest opportunity.
- Working with LiveWell South-West, LD team and Integrated Care Board to support LD patients to wait well: understanding how to manage exacerbation of their chronic conditions and reduce frequency in admission to emergency care (e.g. identification of options for early identification and intervention for people whose needs may be escalating).
- Create a role to support the LD population – part of the “waiting well” initiative.
Re-evaluation throughout to improve our services for patients with LD and sharing of good practice.
How is your project going to share learning?
Most importantly, this project will be shared with the patients with LD, their families, and carers through accessible means. Additionally, the result of this project will be shared internally via our weekly bulletin and through our social media channels. It will also be formally written up and aim to be published in an academic journal to help shared learning across UK or even globally. The progress of this project will also be shared with the Q community through updates on the Q website and results can be shared via presentations at Q events.
How you can contribute
- The Expert - Expertise from the Q community especially in the area of learning disability and waiting list management.
- The Critical Friend - Support and feedback as this project progresses from the Q community would be appreciated.
- The Promotor – Share this project idea within their own organisation, social media and beyond.
- The Collaborator – This may be a larger national problem and to work together to address the LD patients differential access to care nationally.
Plan timeline
| 1 Apr 2023 | Share & interrogate differential waiting list data with speciality leads |
|---|---|
| 1 Jun 2023 | Meet with PPIE & LD support team to understand barriers |
| 1 Jun 2023 | Recruit less than full time project manager |
| 1 Jul 2023 | Complete Subgroup analysis - IMD, multi-morbidity etc |
| 1 Aug 2023 | Complete scoping review |
| 1 Aug 2023 | Target case notes review: GP/ LD team |
| 15 Aug 2023 | Design interventions and outcome measures based on PPIE/ analysis |
| 1 Sep 2023 | Introduce interventions |
| 1 Jan 2024 | Mid-project review |
| 1 Apr 2024 | Re-evaluation and measurement of change |
Project updates
4 Dec 2023
What have you learned so far? This could be either from the successes you have had or from where things haven’t gone to plan.
1. We have managed to take the comprehensive analysis of local data in house – this reveals consistent inequity of waiting list access according to several protected characteristics including LD classification, race & socioeconomic status.
We have conducted most of our PPIE. We have sent out surveys to nursing home managers and carers, had an event for people with LD where easy read versions of the survey were filled in & are about to conduct some in person focus group workshops in the next weeks.
2. Logic framework compiled & domains rated for importance by multidisciplinary team and stakeholders – to guide project workstreams
3. Our scoping review is finished : showing a paucity of literature on the topic of waiting times for people with Intellectual Disability. In the handful of relevant papers , key issues highlighted were fragmented care and lack of reasonable adjustments. We found no studies reporting the impact of waiting times on People with LD.
4. It is difficult to appoint project managers in the modern NHS ! The purpose of the PM is to maintain momentum for all the workstreams; the admin burden has fallen instead on the project leads – but we have found a solution & are about to appoint a manager who will see the project through to the end.
What could others learn from your experience of working with a range of stakeholders and collaborating across boundaries (geographical, professional, sector)?
Through a positive collaboration we have benefited from the clinical, QI & academic expertise of the CIDER (Cornwall Intellectual Disability Equitable Research ) team based at our neighbouring NHS Mental Health Trust to shape our project and improve our effectiveness at PPIE.
This project has enabled us as academics to work with a wider MDT team including but not limited to community and hospital LD teams, CIDER, hospital management and of course our service users. This also enable collaboration across geographical regions in Devon and Cornwall. This has allowed us to learn from each other’s expertise and hopefully make a sustainable positive change and impact to the care of people with learning disability.
We have heavily relied on PPIE, involving all stakeholders including people with learning disabilities themselves, their families, and carers as well as both community and hospital teams involved in their care. The PPIE events have been held in different formats and enable these stakeholders to have a voice in improving their care.
What are the next steps for your project over the coming months?
Identification of barriers through:
- An analysis of the PPIE workshop & survey results
- Granular detail from note review
- Thematic analysis from comments columns from current waiting list datasets
Then construction & implementation of suite of interventions to improve equitable access for people with learning disability, and to attempt to improve “waiting well” so as to reduce need for contact with ED and primary care ( or smooth the healthcare journey) followed by a period of re-evaluation.
We aim to publish the results of the scoping review in an academic journal (submission imminent)
How can the community get involved in your project?
We have connected with Q members to identify to learn from their project ideas. We would invite contact from the Q community who have looked at their waiting lists to identify barriers or implemented interventions to improve access, to see whether they could be applicable to this project!
28 Jun 2023
Here’s our scoping review protocol, registered with Open Science Framework
Comments
Dr Seema Srivastava MBE 21 Mar 2023
This looks like a great project Adrienne. We in Bristol would love to hear about the operational approach to prioritisation for people with LD. How will you do this? Do you use alerts in your PAS or other methods? Are you involving waiting list teams? Good luck with this fab work. Seema
Adrienne Lee 22 Mar 2023
Hi Seema,
We are currently proposing to create a new system to prioritise LD patients, creating bespoke lists and working with staff to reduce on the day cancellations. We are going to engage with specific service lines where our data shows that LD patients are waiting longer. Additional interventions will all be based on what our further analysis will show and outcomes from PPIE.
Comments are now closed for this post.