Q Exchange
Using QI to tackle health inequalities in Primary Care Networks (PCN)
- Winning idea
- 2019
Meet the team
Also:
- Julie Sunderland
- Maureen McGeorge
- Mary McEnhill
What is the challenge your project is going to address and how does it connect to your chosen theme?
Primary care has been slower to adopt QI methodology than other sectors due to the fragmented nature of its structure.
In 2016 NHSE launched ‘Releasing Time for Care’ and recommend developing QI expertise, although the RCGP tells us that not all GPs think QI reduces workload.
A programme of QI training for practices has seen 76 staff from across 14 practices complete the training but no practices have taken up the offer of coaching to start their QI projects.
The NHSE PCN contract from 1st July 2019 will ensure general practice plays a leading role in every PCN and introduces QI modules for the first time. The King’s Fund tells us that where this model has been successful there was a clear agreement on the role of the collaboration for quality improvement.
The biggest challenge is embedding QI methodology. GP practices have varying approaches to QI within different cultures.
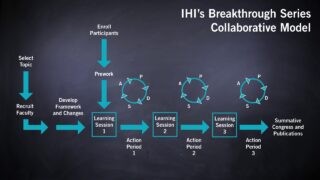
Running a BTS Collaborative in a PCN would build improvement capability across the boundaries between practices.
What does your project aim to achieve?
The PCN in the BTS collaborative will identify a high priority health inequality for its population. We aim to tackle this by utilising the skills across several GP practices, along with community services, third sector, pharmacy, public health & patients. The improvement, process and balancing measures used will relate to this objective. It will focus on improving a system rather than solely on improving skills of individuals. The primary aim is to build an understanding of QI across Huddersfield and give PCNs a framework which can be applied to all future QI projects.
The impact on increasing QI capability across boundaries within a PCN will be measured using the NHSE PCN maturity matrix, supplemented by a survey based upon Kirkpatrick’s framework for evaluating educational interventions.
Sustainability is designed in at the start, using well researched methodology and a well-established infrastructure that can adopt the lessons from the project to scale up at a relatively low cost.
How will the project be delivered?
The project will be delivered as a partnership between MHH, and QI consultants. It will be led by a project steering group with representatives from all key organisations, plus wider stakeholders including the Yorkshire and Humber Academic Health Science Network (Y&HAHSN). We will seek to find a patient or patient representative group.
BTS is a tried and tested change model. The project group is very experienced in delivering BTS, including in Primary Care.
Dr Bibby is a Q.
Maureen McGeorge is qualified as an Improvement Advisor with the IHI.
Lisa is a Q.
Sally, Julie and Mary are practice managers. Sally is a Q.
The team will link into Kirklees Community Voices who engage with the local population.
One PCN will be involved and each practice/organisation in the PCN will be invited to send a minimum of two reps.
Engagement and recruitment to collaboratives can be challenging as can fidelity to the programme. The strong relationship between MHH and the networks will reduce these risks.
What and how is your project going to share learning throughout?
BTS collaborative is not a new concept, but running one in Primary Care and with the newly formed PCNs is new.
BTS collaborative is a learning process with four learning events to share lessons and experiences between participants. Initially learning will be shared among the other PCNs in Huddersfield.
We have Q’s from York and Bradford involved in the project who will be taking the learning back to their organisations. We will update the wider Q community via the Q platform.
With the backing of Y&H AHSN the lessons will be shared with the Integrated Care System Improvement and Innovation Board to be included in their programme covering 2.6m people.
Lessons will be shared with the Yorkshire and Humber Quality Surveillance Group led by NHSE.
In terms of spread, we have agreements with two other CCGs in Yorkshire and Humber to become involved at the spread stage.
MHH and the project steering group have a strong social media presence with wide reach and influence.
How you can contribute
- Welcome the thoughts of other Q’s either:
- 1) Working in primary care
- 2) Previous experience in working in primary care
- 3) Involved with Primary Care Networks (PCNs)
- Has anyone else run a breakthrough series collaborative in a primary care setting?
Plan timeline
| 14 Nov 2019 | Ask PCNs for expressions of interest (EOI) to participate |
|---|---|
| 2 Dec 2019 | Deadline for EOI |
| 12 Dec 2019 | Project steering group meet to decide which PCN |
| 6 Jan 2020 | Start to enroll participants |
| 9 Jan 2020 | Project steering group meet to plan learning sets |
| 19 Mar 2020 | Learning set 1 full day |
| 30 Apr 2020 | Learning set 2 half day |
| 11 Jun 2020 | Learning set 3 half day |
| 23 Jul 2020 | Celebration event and next steps |
Project updates
30 Jun 2020
After a little pause in activity due to Covid-19, I am delighted to say we have started work on this project again over the last couple of weeks. We are having to adapt the way we deliver the collaborative and this in itself is a huge learning curve, but in true QI style we are testing and adapting as we go! The GP practices so far have been very receptive and keen to get cracking with this work. I think they are all pleased to be doing something other than Covid related work!
We’ve started with a series of individual practice update sessions and specific coaching session have followed this. Most practices are still at the diagnostic phase of trying to properly understand the problem and what the data is telling them.
We’ve also re-established the project steering group and the next meeting is 15th July.
Watch this space for more updates soon!
Lisa
9 Mar 2020
Learning set 1 done! Well, what a day! Had a fantastic introduction to Quality Improvement from Dr John Bibby including a patient story to really help us understand why this is so important. We talked through the Improvement Model itself and our experiences with QI projects in the past and what made these a success or not! We discussed our shared problem and began to think about how to express our project aims.
After some not-so-great-coffee and a cookie, Maureen followed up with some learning form a QI project she had been involved in with a Mental Health Assertive Outreach Team and shocked us with the statistic that life expectancy for people with severe mental illness such as schizophrenia is reduced by 25 years and that the major cause of death is not suicide (as we may have imagined) but cardiovascular disease! Maureen covered each of that teams challenges and how they overcame them as well as their key factors in success – something we need to replicate – team motivation and backing from top management and medical staff.
Dr Bibby then took us through a more detailed look at our data which had been taken from our clinical systems by the Data Quality Team and showed Q3 2019/20 achievement against each of the indicators and the overall specifications. We then discussed this on our tables and what we thought it meant. Overall each practice had similarly low figures in certain areas, particularly around bloods and we also highlighted some issues where interventions appeared to be lacking following the identification of an area for improvement, we were unsure how much of these were coding issues.
Lunch was good, although very beige, and happily received by all – we so often don’t get fed at events anymore so it really makes you appreciate it when there is food – and people stay in the room to keep the discussions and relationship building going! Win-win!
Our next session was on measurement and Dr Bibby talked us through run charts and how to recognise improvement in figures as well as the danger of selecting the wrong measures with a hilarious picture of undies on a washing line as proof of global warming – you’d have to see it to understand.
We then talked about what we needed to do to cleanse our data, ensuring the appropriate patients were on the register with some drug to diagnosis searches, CQUIN data from our Mental Health Trust, as well as looking at patients who may have been coded as in remission but were not or maybe shouldn’t be for this. Then there is the issue where problems or interventions may have been freetext and not coded. It was recognised that our data would never be perfect but that we could do some work to make it more accurate.
We next reviewed what we might need to do in the way of further information gathering to properly diagnose our problem. We have our hunches but were trying to learn QI processes to analyse the problem and not jump to conclusions! Do we need to do a short patient survey, the 5 Whys, brainstorm, process map or use the fishbone and then once we’ve done this using the Pareto principle to get the biggest bang for our buck.
We agreed our measures, most of us the same 3, and Maureen tasked us with our homework during the action period. Each team was a assigned a coach to help support them and meetings planned for 3-4 weeks hence to review progress and support the baseline data gathering and aim-setting. Each team will present their baseline data and aims at the next learning set on the 28th April.
Dr Bibby then introduced the idea of a culture survey and this was really well received. As a developing organisation, our PCN are eager for this breakthrough series to build trust and familiarity within our Network particularly as we learn to work together in new ways. Some of us met staff in the additional roles and allied healthcare professionals for the first time today; learning these new skills and celebrating our success at improving the quality of care for this vulnerable group of patients together should be a great bonding experience.
The feedback has been fantastic – I mean, it felt positive and enthusiastic on the day, but it’s great to see that reflected in the feedback forms, particularly as some attendees were a little unsure of what this all involved when they first walked in that room on Thursday.
Some of the most standout comments were; “Thought it would be medical/over my head but it turned out not to be. Understood all that was being spoken about. Well worth meeting with others today.” “Interesting and in-depth. Shocked to think I haven’t covered issues in consultations/reviews. Very informative and gave practice staff a chance for brainstorming these issues.” “Well paced presentation. Very relevant to job role and helping progress”, “Structure worked very well and format was excellent. Content was clearly presented and explained. Helped consolidate earlier learning”
Sally
24 Jan 2020
At our first steering group meeting we discussed getting some data, and appropriate data so that we could use it to analyse the problem further. We posed questions such as: are practices not seeing these patients? or are some of the checks not being done? is there a problem with the templates that’s failing to record everything needed for this check; is there a lack of understanding among clinicians of what is actually involved in this check?
The initial data we had from our primary care dashboard, created by the CCG for “Quality Assurance” and contractual monitoring, showed all 8 of the practices in the PCN to be pretty poor at doing physical health checks in SMI patients, but we felt it would be interesting to compare this to our Quality Outcomes Framework (QOF) data to see if we were better at checks required for that. QOF, however, is looking for far less measures plus, and not to by cynical, has £ attached. Serious Mental Illness (SMI) checks historically did not. Also for consideration is that where a patient has something missing that needs recording for QOF, the clinical systems used in our Primary Care Network, Emis and Systmone, make this really visible with alerts and easy to action data entry, telling you exactly what you need to record and how to do it. These alert a clinician with a patient in front of them that they needed to check something. Also admin teams when they are making contact with the patient for prescriptions or other recalls can easily see what else the patient needs.
Unfortunately there are currently no system alerts that tell us when items are missing from the SMI checks. Perhaps that’s something we could potentially test out, but here we go, jumping to solutions before we have properly analysed the problem!!
We have a local Data Quality Team, commissioned by our CCG, who can run searches on our systems and extract them for us and I contacted the local team for assistance with this. Initially they needed sight of our data sharing agreement from the Primary Care Network (PCN), where each practice had agreed to share information to make the business of being a PCN possible. After a few emails I was able to track that down and get some overall data for each practice, the size of their SMI register and their achievement for each part of the health check.
I also investigated some options for searches we could use to cleanse and validate our SMI register. Arden’s templates provide a case finding search that shows patients that seem to have a serious mental illness due to their medications but no SMI diagnosis on record. We also need to research for recording of codes for remission or resolved to check this is still the case. If someone was in remission but now back on an antipsychotic, they need putting back on the SMI register.
Unfortunately the SMI register requires patients with a very specific diagnoses or on lithium medication to be eligible for the register, which in discussions with clinicians seemed a little restrictive as some patients with severe depression and multiple inpatient stays would not qualify as being on the SMI register. Maybe that’s a problem for another day!!
Sally
14 Jan 2020
We had our first project steering group meeting yesterday where we chose the Primary Care Network (PCN) we will be working with in Huddersfield. There was a great deal of excitement and enthusiasm in the room!
Tolson Care Partnership is the PCN we will be working with. They cover 8 GP practices and have a combined population of just over 50,000. They are quite diverse and atypical compared to the other PCNs in Huddersfield in that one practice is the University Health Centre; another practice predominantly looks after asylum seekers; and another practice has a very elderly population with a large number of their patients living in care homes.
Despite this diversity, they have identified using their population health management data packs, that the care of patients with mental illness could be improved. Their proposal is to use QI to test out different ways of undertaking physical health checks for patients with Serious Mental Illness (SMI).
Work to drill down and understand the data better will happen over the next few weeks before the first full day learning event on the 5th March.
Exciting times in Huddersfield!
Comments
Cheryl Natasha Davies 14 Oct 2020
Really interested in hearing the outcomes and next steps - speaking to a PCN Clinical Director colleague this morning and there is definitely an appetite for this - would be great to be able to share the learning?
Neil Chadborn 24 Feb 2020
This looks like an interesting project and I wonder how you're progressing with setitng up QIC?
I'm a researcher at University of Nottingham and currently reviewing literature about how GPs get involved in quality improvement in care homes. Care homes has come up as a priority in the Primary Care Network GP contract (DES) so I would be interested in your thoughts on how GPs in your network are getting involved in improving care in care homes? Does your project include care homes (for older people)?
More generally - I'd be happy to share our findings as we progress with the review. Also it would be great to talk with one or two of the GPs in your network about their views on Quality Improvement?
Thanks
Petra Bryan 26 Nov 2019
Hi, Great idea about embedding Qi into PCNs at an early stage of their development.
I've recently started as Transformation & Qi Lead at Locala Community Partnerships who provide community services across Kirklees, working closely with primary care & PCN colleagues. If this proposed work involves PCNs in our patch I'd be happy to support and be actively involved in any way that would be helpful
Look forward to hearing more,
Petra
Ed Kingdon 21 Oct 2019
Great ideas
Liz Fisher GP and Q from the Primary Care SIG may well be able to add useful insights
Really intrigued to hear about primary care BTS
PCN structure may offer an opportunity to embed QI in works as delivered and to demonstrate QI as a means of doing fewer tasks without value as well as new valuable tasks
Sue Goodfellow 14 Oct 2019
Congratulations on being shortlisted.
We have lots to learn in Primary Care in improving QI capacity and capability. The fragmented nature of our service, with relatively small organisations ( individual Practices) makes the challenge of embedding QI skills more difficult.
Happy to contribute as a GP QI enthusiast facing a similar challenge!
Natalie Parkinson 8 Oct 2019
We thought of something similar so would be really interested to be updated on progress and see if we can spread to other areas i.e. ours!
Lisa Jamieson 8 Oct 2019
Thanks Natalie, will keep you updated
Helen Crimlisk 8 Oct 2019
Keen on hearing more about this. So important to get QI into primary care network
Lisa Jamieson 8 Oct 2019
Hi Helen
Yes absolutely essential if PCNs are going to be able to deliver everything they are being asked to deliver. I notice you are in Sheffield so I might be in touch to talk to you about spread!
Thanks
Lisa
Stephen Lock 7 Oct 2019
Love this idea. The team I manage at the National Institute of Health Research has done some work using behavioural and data science to map health inequalities. Our experience has shown that careful design of relatively simple tools can encourage people to engage with the topic. I'd be very happy to show this to you if it might help your thinking.
Stephen
Stephen Lock 8 Oct 2019
Great Lisa. You can get me at stephen.lock@nihr.ac.uk. I live in Kirklees (work in Leeds) so perhaps I can pop over and show you what we've done.
Look forward to hearing from you, Stephen
Lisa Jamieson 7 Oct 2019
Hi Stephen
Thanks for the comments. I'm very interested in the work you have done. I'll message you directly so we can arrange a call.
Many thanks
John Lodge 1 Oct 2019
This is certainly a subject area that requires a lot of attention and the learning from it will be really useful nationally
Lisa Jamieson 8 Oct 2019
Thanks John and thanks for introducing me to Hexitime.
Chipfunde Elijah 23 Jul 2019
Brilliant ideas good project.I am proud to learn a lot.
Tony Jamieson 18 Jul 2019
Hi Lisa,
Y&H AHSN has a project to help PCNs identify and prioritise health Inequalities. Looks like the timing should be right to help out as your project kicks off. It would be amazing if our PHM tools could be used in one of your early Learning workshops.
Tony
Lisa Jamieson 23 Jul 2019
Thanks Tony, be more than happy to incorporate this. Be interesting to see if the data tells us what we think we already know. Essential that we are working on the right things.
Sarah Fiori 10 Jul 2019
Really valuable idea and one with transferable learning for other PCNs who are engaged in this approach. The opportunity to help PCNs address their identified health issues alongside increasing QI capacity within frontline teams is fantastic and can only be of benefit to all but primarily the patients.
Jem Ramazanoglu 9 Jul 2019
Great idea - I would be keen to see how this works out. I am a fan of the BTS approach and wonder whether this might work in tandem with our Quality Coach development programme bid which is looking to develop local QI capability to support QI initiatives in PCN/ICS development?
Perhaps, if both bids are successful, we might use the Quality coach programme to develop local staff that can provide the sustainability for the BTS work?
Lisa Jamieson 10 Jul 2019
Great idea Jem, I can really see how these two projects could work in tandem.
Carole Hallam 9 Jul 2019
This will be a value project and has the potential to grow QI skills and motivation with PCN for further work. I look forward to being part of this project
Sally Oldbury 28 Jun 2019
Brilliant idea, looking forward to working with you on this!
Anna Burhouse 26 Jun 2019
Welcome Lisa, looking forward to hearing your idea.
Lisa Jamieson 27 Jun 2019
Thanks Anna
Comments are now closed for this post.