For children with complex medical needs, outpatients, and people with long-term conditions, the role of health professionals is increasingly about empowering families and individuals to manage care at home and to recognise when clinical intervention is needed. Patients, families and carers are the real experts here. They’re the people living with the condition day in, day out, learning what works best for them. So, what if that knowledge and expertise could be harnessed for the benefit of patients and health service professionals alike? Three projects, funded by Q Exchange, are showing just how powerful co-production with patients can be.
Addressing the right challenges
Patients and their carers are a huge – and largely untapped – resource when it comes to redesigning services.
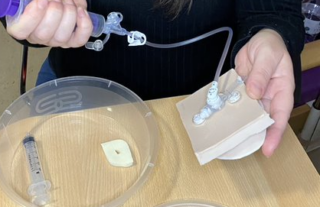
In the area of children with medical complexities, the shift towards self and family-provided care means that health providers also need to become health educators. For Bethan Page at the University of Oxford, who leads the Q Exchange project, the support families needed was a mix of information and training from clinicians and peer support from other families facing similar challenges. Their project set out to develop resources with and for families to train them to do procedures they need to do at home.
At Torbay and South Devon NHS Foundation Trust, the Head of Personalised Care Helen Davies-Cox wanted to tackle the dual challenge of increasing demands on outpatient services and the need to reduce outpatient appointments by a third in the next five years. Recognising that patients and their carers are a huge – and largely untapped – resource when it comes to redesigning services, she and Strategy and Development Manager Liz Procter set about involving patients and carers, along with clinicians, community partners and health improvers, to reimagine outpatient services. They did this primarily through an in-person co-design event that they were able to run in September 2019, before COVID-19.
A similar project from NHS Surrey Heartlands CCG and Royal Surrey County Hospital NHS Foundation Trust, looking at outpatient services, had to refocus their efforts when COVID-19 hit. At this point, the clinicians who were on board with the original project were redeployed to other areas and virtual consultations became an urgent priority in response to the pandemic. The project shifted its focus to working with patients to ensure that virtual consultations would be accessible to everyone.
The project shifted its focus to working with patients to ensure that virtual consultations would be accessible to everyone.
Rheanna Mitchell, Head of Planned Care Commissioning G&W ICP at NHS Surrey Heartlands CCG said what was important for the project’s success was to do something where there was enthusiasm and support from the clinicians and other stakeholders involved.
“Our reflection was to carefully think about whether there is support within that setting; if the project is fundamentally linked to priorities within that setting. Otherwise it loses momentum,” she said.
Involving patients, clinicians and community partners
Co-producing with a range of stakeholders including patients, carers, families, clinicians, allied health professionals, statutory bodies, charities and community groups was common across all the projects. Each used different techniques to gather information and involve patients and the community.
These included:
- conducting an evidence review to understand successful co-production
- conducting stakeholder interviews, surveys and online workshops
- bringing people together face-to-face in a non-hierarchical, non-judgemental setting
- working virtually using social media, email and video
- testing ideas and gathering feedback.
For all the projects, giving patients and carers a voice and placing them on an equal footing with clinicians was key. Often in health care the power dynamic is strongly in favour of the clinician. Co-production is able to turn this on its head.
Bethan Page said that even before their project was funded, they wanted to get the right mix of people together, including community nurses, clinicians and families.
“You need to have a few families you can work with right from the start – from conception, before funding. We had two parents that were happy to come to the meetings – had equal input into it and weren’t afraid to cut across senior clinicians. They kept it really focused on what other families needed,” she said.
Giving patients and carers a voice and placing them on an equal footing with clinicians was key.
Torbay and South Devon NHS Foundation Trust’s Liz Procter also talked about the importance of creating a non-judgemental, safe space where patients felt their views were valued:
“What we saw was that clinicians weren’t used to working with patients on an equal footing…It was so important that we had clinicians there listening to what patients were actually saying.”
The responses from patients bear this out.
“You’re given a voice, and I think that’s so essential,” said Rachel Tucker, patient and volunteer on the HOPE programme at Torbay and South Devon NHS Foundation Trust.
A parent involved with the project supporting parents to care for children with medical complexity said, “I think the balance between parents/carers having first hand experience and also clinicians is really important and done very well.”
Learning from the projects
Helen Davies-Cox said that while involving patients was recognised as a key part of redesigning services, not everyone had the skills and knowledge – or the time – to do this well.
It was important to get the power dynamics right from the start. “Do people actually feel able to speak up and that they’ve got equal share?” Bethan Page asks.
Providing different ways for patients to feed in their views means that projects can hear from a wider range of patients. While some patients are happy to attend meetings, others will prefer providing feedback via email, filling in surveys or conversing on social media. It’s most effective to contact families where they are, for example on Facebook or in a clinic, and build the relationship from there.
A particular challenge in all the projects was engaging clinicians throughout the process and initial enthusiasm could quickly be overtaken by the demands of the day job – especially during a pandemic. Finding ways to align co-production with clinical priorities and resources to support the change process within trusts is key.
Providing different ways for patients to feed in their views means that projects can hear from a wider range of patients.
Rheanna Mitchell identified one of the challenges with co-production was that it raised patient expectations and while the solution often sounded simple it could take a really long time, working with multiple stakeholders, to make the changes. Patients and other stakeholders can become frustrated with how slow this is.
“This type of approach cannot be done in a silo by any one person. It’s most successful when you listen to the experiences of others and take the best bits from their examples and, actually, it’s iterative. Things will change and it’s about rolling with it and developing it each day,” Rheanna Mitchell said.
Outcomes
Outcomes from the projects ranged from practical changes for patients, such as offering an email option as well as a telephone call to make contact accessible for people with hearing difficulties, to a series of 19 videos and a set of 30 part-simulators co-produced by parents to support families with learning how to care for their child’s gastrostomy (a type of feeding tube).
A parent involved in the project for children with medical complexities said, “This was so normalising and reassuring. It helped us to imagine our lives when our daughter has her [gastrostomy] button in place. [The videos] were incredibly empowering.”
The evaluation with 33 healthcare professionals (HCPs) and 42 families from that project showed:
- 100% of HCPs & 98% of families would recommend the videos to other parents
- 100% of HCPs and 100% families agreed the information in the videos was easy to understand
- 100% of HCPs and 98% of families agreed the videos would help families to feel more confident.
The video consultations project at Surrey Heartlands CCG is ongoing and being tested with health care professionals. So far it has enabled a review of approaches to co-production with best practice that can be shared widely, multiple contact options for patients, longer appointments for patients with dementia and data sharing with the local Healthwatch.
The solutions are different to what you as a clinician think they will be.
The co-design workshop for outpatient services at Torbay and South Devon NHS Foundation Trust involved 135 patients, 10 carers and 35 clinicians across four secondary care specialties. It has informed a series of improvements to services, from the development of an app to help patients manage multiple conditions to volunteer peer health and wellbeing coaching, which is now being rolled out across outpatient services.
Helen Davies-Cox said their co-design methodology is now being incorporated into improvement work in both primary and secondary care:
“Because of the learning, the co-design is now part of the health and care strategy and quality improvement projects within teams. People still ask us how we did it. It’s socialised the need for this, especially within secondary care. Within community care it exposed people to the pure power of working with real people. The solutions are different to what you as a clinician think they will be.”
Interested in finding out more about the projects? Get in touch with the people behind them on the project pages in related links to the right of this article.
Comments
Helen Lee 16 Aug 2021
Great article Jessica - thank you for sharing. Would love to catch up and chat sometime. I work in the national Experience of Care Team at NHSE/I and co-production is in my portfolio. If you'd like to catch up let me know some dates that would work for you.
Take care
Helen Lee
Jessica Rose 17 Aug 2021
Hi Helen,
Great to hear from you and glad the article is useful. I'd be happy to chat - will email you.