Q Exchange
Improving Outcomes for Vulnerable People with Inflammatory Bowel Disease
- Proposal
- 2024
Meet the team
Also:
- Vicky Buckley, Lived Experience representative, CCUK South Yorkshire
- Sam McCormick, Patient coach, Sheffield Microsystem
- Anu Agrawal, Consultant Gastroenterologist
- Priya Mothey, Consultant Gastroenterologist
- Sarah Harrison, Senior IBD nurse specialist
- Tim Wilson, Consultant Surgeon
- Kevin Randall, Analyst
- Kelly MacKenzie, Consultant, Public Health
- Rachel Hawkins, PhD student
- Louise Millington, GP South Yorkshire ICB
What is the challenge your project is going to address and how does it connect to the theme of 'How can we improve across system boundaries?
Inflammatory Bowel Disease (IBD) causes debilitating symptoms and significant psychological impact. It requires personalised, integrated care. Services fail vulnerable people through poorer access, outcomes and experience.
Despite advances in treatment, emergency admission rates have doubled in a decade – a system failure potentially preventable by integration across primary and secondary care, community assets and better supported self-management.
Deprivation, hospitalisation and mortality are linked (a “health inequality gradient”) in general and in two target areas, Sheffield and Doncaster (HDR UK):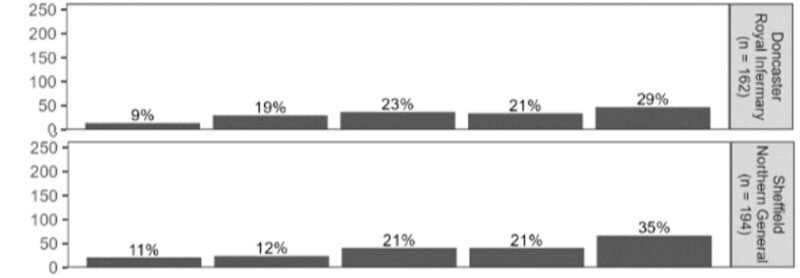 In our Health Foundation-funded AWARE-IBD programme we learnt from patients about values and priorities, co-designed a patient-reported experience measure (PREM) and engaged marginalised communities to understand barriers to care (In press; doi 10.1111/hex.14004). Uniquely, a patient-coach led a microsystem co-producing changes improving access, personalised care, communication, self-advocacy.
In our Health Foundation-funded AWARE-IBD programme we learnt from patients about values and priorities, co-designed a patient-reported experience measure (PREM) and engaged marginalised communities to understand barriers to care (In press; doi 10.1111/hex.14004). Uniquely, a patient-coach led a microsystem co-producing changes improving access, personalised care, communication, self-advocacy.
We want to spread this learning to Sheffield and Doncaster’s 20% most deprived IBD patients using co-production to improve transitions between hospital, primary and community care.
What does your project aim to achieve?
- Understand access barriers and experiences for vulnerable IBD patients across Sheffield and Doncaster’s health and care systems
- Identify priority areas for improving transitions and integration between hospital, primary and community IBD services
- Patients will lead changes to achieve benefits including: reduced waiting times, better self-management, appropriate hospital use and more personalised care.
- Support those from underserved communities to co-design and trial changes which connect care across sector boundaries
- Facilitate care consistent with evidence and patient preferences
- Empower patients to manage their health
- Measure impact on equity, access, experience, appropriate hospital use and supported self-management including use and adaptation of our newly developed PREM
- Share learning on working across system levels to reduce boundary issues for vulnerable groups
How will the project be delivered?
- A patient oversight group will ensure providers, patients and communities are engaged as partners
- Identifying patients at highest clinical and social risk from routine data
- Identifying, in a regular multidisciplinary forum, barriers in clinical and social care reducing engagement with primary care or specialist IBD services, worsening the impact of the condition (access, experience, emergency admission)
- Experts in co-production and marginalised group engagement will work with the 20% most deprived IBD patients to understand experiences across care boundaries, identifying priority integration issues.
- Our team is constituted to develop cross-sector partnerships with the Integrated Care Board, primary care networks, community organisations and peer support networks to co-produce solutions
- Patients co-design ’Plan Do Study Act’ cycles of change
- Measuring impact: access, experience, appropriate hospital use, supported self-management, barriers for underserved communities identified from our published experience (doi 10.1111/hex.14004).
- Spread considered from the start, with project partners representing every level of the local system.
How is your project going to share learning?
We will share learning in multiple inclusive ways:
● National and regional conferences/webinars
● Publish open access papers detailing methodology and impact
● Create accessible photo stories and animations of patient experience
● Policy briefs for local, regional and national systems
● Build a ‘how to’ toolkit for marginalized co-production across care boundaries
● We will actively seek input from other Q members throughout and encourage wider adoption of effective changes through our spread networks.
How you can contribute
- Advice about who to engage and how to intervene at the intersections of these boundaries between health and social care
- Examples or advice about population based approaches for long-term illnesses
- How to assess the need for and impact of changing the venue of care delivery from the perspective of all stakeholders
Plan timeline
| 1 Oct 2024 | Project start. Introduction and clarification of team roles. |
|---|---|
| 14 Oct 2024 | Identification of initial cohort at risk at intersections of care |
| 4 Nov 2024 | Contact initial cohort; Support Patient Reported Experience Measure (PREM) submission |
| 13 Jan 2025 | Baseline PREMs from initial cohort completed; review ongoing recruitment |
| 13 Jan 2025 | Completed analysis of challenges affecting individual patients; interventions planned |
| 7 Apr 2025 | Review of outcomes from initial cross-sector interventions; adjust if necessary |
| 5 May 2025 | Commence semi-structured interviews of patients and stakeholders |
| 31 Jul 2025 | Compile themes across cohorts; analysis of changes in PREM |
| 31 Jul 2025 | Review of outcomes for whole cohort; final adjustments if necessary |
| 30 Sep 2025 | All results analysed (themes, change in PREM); Project report |
Comments
Dawn Eustace 4 Mar 2024
I am a parent of an adult child with Crohns and UC, so I am always interested in the delivery and sharing of information and care to this patient group and their support networks.
I think 'Health Literacy' has a part to play for communities whom we may not be connecting with and therefore, their care and support can be compromised. In Croydon, we are considering the literature we provide and the appropriateness of methods of communication at the earliest opportunity to encourage engagement and understanding of health conditions.
An area of collaboration in Croydon is with people who have had a Stroke. Working with the Stroke Society, signposting families, friends and advocates and aligning information; sharing information in a range of methods, (language line, large print, visuals ) to ensure access to information is readily available to all affected by long term health conditions. Providing options for them to engage where they feel comfortable and have trust.
I will be interested to hear how you progress with your project and wish you every success.
Alan Lobo 5 Mar 2024
Dear Dawn,
Thanks very much for your interest and comments. You have raised a number of important issues. Health literacy is a really important contributor to the people we are looking to support in this project. We are trying to put 'what matters to you?' at the heart of clinical encounters and will do so in this project. We have co-designed a 'toolkit' with VoiceAbility - a peer-support organisation which helps people to articulate this, The link is here. Issues relating to language and literacy were identified in the outreach work we undertook with underserved communities and which has just been published. We will use all the learning from that to co-design support. Thanks again for your comments and interest. We'll make sure they are represented as we design the support.
Holly Smith 4 Mar 2024
This sounds like a very interesting project, patient led coaching and patient/carer involvement is key in understanding barriers and inequalities.
How do you plan to engage patients from the underserved and deprived communities?
Alan Lobo 12 Mar 2024
Thanks Holly. We have thought a lot about this and would co-design the interactions. Our experience in the AWARE-IBD programme has given us important feedback about the being flexible in our approach and aware of issues relating to language, literacy, choice of venue and trust. We designed meetings with advice from the communities and their leaders. We would draw on considerable experience within the proposed project team including a GP who has developed programmes to address underserved populations and health inequalities in her area. One of the team is a Public Health Expert to give a population based perspective and with experience of developing innovative ways to reduce health inequalities including the inclusion of system navigators and community connectors in a service.
Helen Crimlisk 23 Feb 2024
A really wide ranging project with ambition for impact across the care pathway with a clear QI methodology and an explicit inequalities angle. The involvement and leadership of patients and families is critical and flips our thinking about power relationships and ownership.
How will you engage with local and national self help groups?
Have you thought about the training /CPD needs of primary care staff in supporting appropriate patient education across the pathway - especially in light of the changing nature of primary care?
Alan Lobo 26 Feb 2024
Thanks Helen. Crohn's and Colitis UK have been key partners with us so far - both nationally and through the local group (which extends across South Yorkshire). They will continue to be at the heart of this and developing interventions for the vulnerable groups we are addressing. Your point about primary care training is really important. We will take this up with the GPs in the group - including those serving deprived areas in Sheffield. There may also be other community-based opportunities for support that we would co-design in this project. Thanks for that steer!
Tom Downes 22 Feb 2024
Love this idea - builds on the Core20plus5 national policy focus on inequality. Crohn's and Colitis UK had the 'Weeks not years' to diagnosis campaign last year - this is the next step. Improving access and patient activation to support self management is crucial for sustained impact.
There will be many members of the Q community who either have a family member or friend with IBD - this creates the opportunity to spread the work further.
Alan Lobo 26 Feb 2024
Thanks for such a positive response, Tom. The tools we have developed have had supported self-management in mind. The work we have done with underserved communities has given us a real insight in to the support that is needed for that.
Anna Burhouse 20 Feb 2024
This looks like a brilliant idea and will allow the learning from your work to date to be spread. How do you think the work will evolve and what help would you like from Q members?
Great to see your ambition nd drive to push this forward :)
Alan Lobo 26 Feb 2024
Thanks Anna. We're really keen to utilise and spread the learning from our project. We hope that what we learn and develop in this project will be applicable to other teams. There is clearly a huge amount of experience in the Q community that clinical teams could learn from. We'd be particularly keen to hear from teams where they have looked to support people with other long term conditions in terms of wider determinants of health and how they interacted with agencies to secure that support. This has been described as supporting health behaviour for a group of people with long term conditions who face a debilitating combination of unpredictable flares and pscyhological impact - mainly hidden from those around t hem.
Comments are now closed for this post.