Q Exchange
Engineering out errors across critical care
- Proposal
- 2024
What is the challenge your project is going to address and how does it connect to the theme of 'How can we improve across system boundaries?
The lives of patients on intensive care are dependent on a wide variety of drugs and devices, resulting in a complex multidisciplinary environment. Inevitably errors do occur, some of which result in death or serious harm. Regional and national efforts to reduce reoccurring risks focus on sharing learning from events, but this has a limited lifespan as staff move between hospitals and are overburdened. Unfortunately, similar events continue to occur across the UK[1]. Solutions to mitigate risk must go beyond learning and embed the designing of safer systems into the working environment, using expertise from academia and industry. This project aims to develop a process to engineer out risk from commonly occurring high-consequence events, by bringing together experts from across traditional boundaries; as adopted during COVID 19[2]. This approach will be modelled nationally to be applied with support from the Q community in local units.
[1] https://www.hssib.org.uk/patient-safety-investigations/the-use-of-an-appropriate-flush-fluid-with-arterial-lines/
[2] https://ergonomics.org.uk/resource/design-guidance-for-ventilators.html
What does your project aim to achieve?
The project aims to demonstrate a method to address a high-consequence, high-frequency safety event. Having selected the incident (4 have been preselected using national data), the national group will work collaboratively and cross traditional boundaries to develop a process to identify and design risk mitigation solutions. The design process and solution should be implementable in every intensive care unit in the UK. This process will recognise the complexity of the environment, the interaction of staff with patients and devices, and the ease, cost and reliability of implementation at a local level. Introducing a sustainable design solution will aim to reduce the frequency of the event, the risk for the patient, and medicolegal costs to the wider system. Appropriate data will be gathered to support the project. Whilst this project is based around high-consequence risks in intensive care, the methodology and process will be applicable across wider healthcare and community settings.
How will the project be delivered?
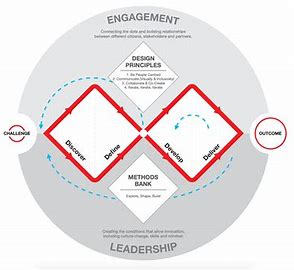
A team has been assembled including: intensive care doctors, nurses and allied health professionals with quality improvement expertise supported by the Faculty of Intensive Care Medicine, the Intensive Care Society, a research team from the University of Bath Centre for Healthcare Innovation and Improvement, an expert systems engineer, and a human factors expert. The group has pre-selected four potential risks and will develop a selection criterion to choose one for the first stage of this project. An initial exercise in data identification and evaluation will inform the process and measurement of impact, whilst considering health economics and evidence of risk mitigation. An iterative and user centred approach to the development of the design solution will ensure full stakeholder engagement and manage the risk of unintended consequences; further supported by rigorous testing through simulation in participating pilot intensive care sites, prior to a full national roll-out.
How is your project going to share learning?
As we already have engagement from the two national bodies representing intensive care in the UK, we have easy routes for communicating the methodology and the risk mitigation solution itself. We have a pre-arranged a slot in the safety section of the State-of-the Art intensive care meeting in 2025 and intend to publish the methodology and experience in developing and designing safety solutions; reaching across clinical and engineering boundaries. This will share the learning for future projects. More broadly, our diverse group will identify suitable routes through their own professional bodies to share the experience of this project also including: universities, systems engineering, human factors and quality improvement pathways. Finally, we hope that the incredible breadth of collaboration in this project and the methodology employed may be a blueprint for healthcare improvement outside of intensive care, and the Q community will be a fundamental part of that process.
How you can contribute
- Propose criteria to consider for the selection process
Plan timeline
| 1 Jul 2024 | Define and agree the problem to be addressed |
|---|---|
| 2 Sep 2024 | Develop through system engineering and participatory engagement strong system solution |
| 1 Oct 2024 | Develop and identify requirements for implementation |
| 4 Nov 2024 | Iterative design process to formalise solution |
| 4 Feb 2025 | Evaluation and testing |
| 2 Jun 2025 | Team engagement and project milestones and processes confirmed |
| 4 Jun 2025 | Reporting |
Comments
Clare Crowley 12 Mar 2024
Great to tackle some of the know wicked problems from a design approach reflecting the setting and context of use. Great idea.
Nicholas Seaton 1 Mar 2024
This looks like a brilliant project with some top experts in the field! I hope this project is successful and would be really keen to follow its progress.
Laura Pickup 4 Mar 2024
Thank you Nick
Comments are now closed for this post.