Q Exchange
Defining and producing examples of how to document interface Processes
- Idea
- 2024
Meet the team
What is the challenge your project is going to address and how does it connect to the theme of 'How can we improve across system boundaries?
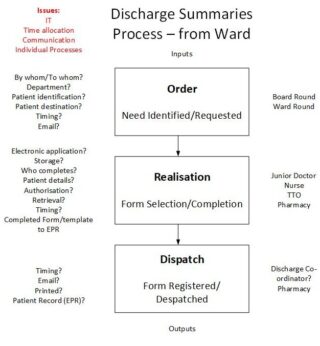
This idea involves many parts of the health and care system and focus on improving the quality and efficiency of the interface between different sectors. For example: Discharge Summaries; the interface between Primary and Secondary care. Defining and producing examples of how to document NHS Standard Processes (WAD) that cross interfaces in different sectors of the healthcare system. Example documentation sets will be produced, of WAD, for process that cross boundaries/interfaces e.g. the Discharge Summary process. How tasks in a process link to IT systems is too often overlooked yet it is so important, particularly systems that cross boundaries.
What does your project aim to achieve?
Process clarification, training and improvement. To show what a ‘process’ is and how to document it. Many processes in the Patient Pathway cross system boundaries and it is important that required patient information also crosses these boundaries at the right time.
How will the project be delivered?
Initially, use the QI methodology and tools to map (Flow Chart) the relevant inter-operational processes (WAD). Followed by using The Model For Improvement to improve the individual processes. All documentation produced will be compliant with the requirements of BS ISO 7101:2023.
How is your project going to share learning?
Prior to the start of the project an effort will be made to explain what process documentation is and, importantly, how to do it. This effort will continue throughout the project. For the first session see: https://q.health.org.uk/event/how-to-overcome-todays-lack-of-nhs-process-documentation-to-support-effective-improvement/
How you can contribute
- Would you like to be involved in this idea?
- Can you suggest any cross area processes that could be included? We are already looking at Discharge Summary. Is your Trust reviewing it's Discharge paths?
- What about blood test requests/sampling/testing/results? Do you have any issues Primary/Secondary Care?
- Please add a comment and/or a Like
Comments
Thomas John Rose 18 Mar 2024
Unfortunately no Trusts are willing to support this Idea. Thanks to those that did show some interest.
Thomas John Rose 13 Mar 2024
This idea requires the collaboration of at least one Trust. Is there a Trust out there that is interested in participating?
Thomas John Rose 13 Mar 2024
Have a look at this: https://www.nhsconfed.org/improving-interface-working-across-primary-and-secondary-care
Flow seems to be just one way so no mention of discharge summaries!
Lawrence Brad 11 Mar 2024
a long standing interest in this and the incredible amount of variation we see in discharge summaries at the secondary / primary care interface
Medication changes are particularly difficult at the interface when there is often such a rapid turn around of patients with acute illnesses . Often we have found when it comes to meds reconciliation at our primary care side , ongoing changes and titrations up and down are needed quite quickly (and often before we get the formal discharge document )
I do think we need to consider the patient facing interface through the NHS app as these letters can be seen, as can GP (but not hospital ordered )results so often there is hidden info and potential to not give the patient the complete picture through the NHS app as it stands
hope this makes some sense and very happy to be involved if can be of any help!
Thomas John Rose 13 Mar 2024
Thanks for you comments Lawrence. I do think that IT, medication and speed of response are all very important areas for consideration. It's a difficult task but it needs to be addressed. I'm sure that a systematic process approach will provide results.
Paul Rylance 23 Feb 2024
Nice idea Tom. Happy to support if able
Thomas John Rose 23 Feb 2024
Thanks Paul. I'm sure your help will be very helpful. Keep you eye open for Idea page updates as there is much yet to add.
Nigel Coles 21 Feb 2024
That looks like a great project, I would certainly like to get involved in a project looking at the process of patients receiving results of diagnostic procedures. We can't rely on the old "if you don't hear from us the results are ok and nothing to worry about". We need to work on the process to reduce stress waiting for results and prevent deterioration in the patients condition when waiting for results. Results should be accessible to patients.
Regards
Nigel
Thomas John Rose 21 Feb 2024
Thanks Nigel. Yes I've been on the receiving end of that message a few times. I'll add you to the Project Team.
Rollo Moore 12 Feb 2024
I would ask whether the idea can apply to advancing safer radiotherapy in terms of dosimetry audit involving multi-disciplinary team, and how patients might choose to be informed of this approach to safety.
Thomas John Rose 12 Feb 2024
Rollo, Certainly. Communication between the Department and the Outpatient/GP involves two or more parts of the health and care system and will focus on improving the quality and efficiency of the interface particularly if you ask for feedback.
Emma Stinton 9 Feb 2024
Great idea Tom. I did some work on hospital discharge summaries a few years ago and as mentioned above there was a lot of value in mapping the (more complex than anyone thought) current state. As important fixing the process issues were they didn't work without consideration of human factors. As much as I agree that agreeing and documenting processes is really important I hope there's room to consider how to ensure people do the right thing at the right time, and our experience was that needed a behavioural insights lens. I'd like to be involved you're successful.
Thomas John Rose 9 Feb 2024
Thanks Emma. I agree that human factors and behaviour are very important and are often overlooked. I think that documenting the process is just the start, behaviour issues can be address during staff training and human factors addressed during trials. On going process management will ensure that the process and staff remain effective. Your involvement will be most welcome.
Michelle Beattie 9 Feb 2024
Great idea - so many issues with discharge and I've seen mapping of steps and processes work well as a starting point to identify problems, solutions and standard work. You have likely thought of this already Thomas but the only thing that springs to mind is even within the interface of discharge there is so much variation i.e. discharging home, discharging with social care package or to a care home. So would you focus on a particular interface for the project or more high level? Not sure if I could help but I've done a few QI projects and I'm a nurse by background and interested to see how your ideas evolve.
Thomas John Rose 9 Feb 2024
Thanks for your interest. For the Idea to go ahead I need to find some Trusts to work with and the exact Discharge destination would be their choice. Ideally with several Trusts participating in the project a number of processes to different destinations could be documented. Please keep your eye on the development of this idea and keep on commenting. I'm sure your help will be valuable. Thanks
Thomas John Rose 8 Feb 2024
Thanks Hilda. There are so many aspects to healthcare processes. Professional reporting is certainly a key element. Failings in this area can impact the patient for many years to come. Timing is also very important. The patient is often in front of the transfer of information. Just as important though is the needs of the individual patient. These needs are so often outside the scope of the process design and documentation. This feature of a process was considered in the first Q Lab. That also included aspects of mental health. Culture, training and process and people management are important here. Implementation trial must include patients were specific patient issues can be identified and addressed. I'm sure that any examples of co design would be of value.
Thomas John Rose 21 Feb 2024
In reply to your last post of the 12th Feb., sorry it's a bit late. A simple process map illustrating the key steps taken improves communication no end. It also allows people to concentrate on improving the process without looking too deeply into individual tasks in the process and visa-versa. It enables people that are not directly concerned with the nitty-gritty of the process to make an informed comment on the process inputs and outputs and how they could be improved from the view as a supplier or customer to the process. Unfortunately there is a lot of miss understanding regarding processes and process mapping. Done well it can make such a difference. Additionally process documentation is a pre-requisite of a Quality Management System and also a Safety Management System. Thank you for your valuable comments.
Hilda Campbell MBE 12 Feb 2024
Morning Tom
I think this is why I like your idea so much, as if I understand correctly, its not just the system in one trust/department/team, but how they connect to others and where this works/could be improved. I know from my experience in nursing, we worked a two shift system, 12 hours a day so many on, so many off and unless you were on overtime you didn't meet the other side of the shift in person, so all they had to go on was reports. Depending on who was in charge each side of the shift often impacted on WAD. There was a change and the creation of ward managers which I was for a while and we could work both sides of the shift. This made it a lot easier to improve communication between both sides of the shift as well as capture ideas from both sides to improve outcomes for the residents of the ward and students on placement as this was another issue when there was no clear communication the student experience was different each shift.
I was also involved in my current role around primary care transformation, and when GP's were able to meet with addiction services and each explain to the other their processes and the impact this had on referrals then they were able to make changes which led to improvement. The same when they met third sector and community groups and understood more of their systems their confidence increased to work closer with them and one practice went on to support its own peer support group.
There are so many examples. In a time when people are pushed for time it can be hard to promote why taking time out to understand our systems, and also how they link and connect to others is important, but it is, as when we do this we can then clearly see what is happening, what we can learn and what can be improved.
My own experience of any activity like this has been, while a time investment was needed initially, as a result of that things improved for people and those delivering services.
I can also think of a time when significant budget changes were planned and like a broken record I kept saying, ''we need to do an impact assessment'', it didn't happen. The changes happened (how the third sector was funded by a particular funding pot) and well, lets just say, things are still being worked out. If an understanding of how the various sectors complemented each other and supported communities then changes could have been planned differently.
My own charity recognised we needed to change and over a period of 3 years focused on building capacity within the communities we served so the need for our service was less and we could withdraw, meaning there was one less charity seeking funding from that pot. Not an easy decision as that was our core funding. Our mission now over the next few years is to share what we have learned for others to use as helps the work they are doing and then we shall close all together.
This is the challenge when looking at systems and change, sometimes we need to stop doing one thing to be able to do something else and those conversations are not easy. The communities, partners and people we served understood what we were doing because we spent time talking, sharing, looking at alternatives, this is why improvement needs to involve those who do the work. We still visit the community we came from, using our own resources which we generate from pieces of work, later this month we are offering a session to a group which will touch on how they all interrelate with a variety of other stakeholders and systems.
I do hope you move to putting in the fuller application as I think its a great idea and if I can help you, then please just ask. We have never been a charity which follows the pound but the principle and what you are seeking to do, will be a challenge, but, one worth taking on,
Kind regards
Hilda
Thomas John Rose 11 Feb 2024
Hilda, this is a great story. I love the thought of everyone on their hands an knees following the patients journey round the room on a rolled out roll of wallpaper. An example of people working together and creating a visualisation of a Service so that everyone can got an understanding of the whole. Certainly technology can replace the roll of wallpaper but what I like about your story is that it worked and people gained the understanding of the full extent Service being offered, with all its issues and areas to be improved. My current approach to visualising a healthcare Service, which has evolved from initial activities like the one you describe, is to break the pathway down into discreet processes and produce more detailed visualisations of those processes and work on improvement ideas. Of course process inputs and outputs have to be considered so that all the individual processes in a pathway work together. Often these individual processes are undertaken by different work-groups or teams/shifts or even different department. It is necessary to work with relevant FLS to get a true picture of WAD. I don’t underestimate the difficulties in doing that!
Hilda Campbell MBE 9 Feb 2024
Hi Tom
I remember, we secured funds for the whole team to undertake lean management training together. There were many parts of this were helpful. One activity we all found helped us review our systems and processes was getting a roll of wallpaper! getting down on the floor and starting from how do people find out about our service, where are they coming from, who told them, what do they expect, to what happens when people leave the service we charted that journey, sticking our marketing, assessments, tools/resources/approaches/details of partners etc so you could see from start to finish the journey through the system and the actual tools/materials being used, it was also helpful as it enabled you to go off track e.g. people do not engage so we need to improve our pathway there and find out why .
We then repeated the exercise with representatives of people using the service, then compared the two. This helped us make improvements in promotion, the information people received about the service once they engaged co designed with the public, and so much more, it also led to the change in assessment and resulted in a peripatetic service as in charting people who did not engage, cross referenced with their postcode we realised that although not that far away in distance it was two bus journeys which had additional costs and time for people, when we offered a day a week service at another location more convenient for people engagement improved significantly and that area became our second highest postcode for engagement. It was also simple things like having hankies in the room to offer someone if they were upset rather than having to leave and get them a piece of toilet paper! having a water flask and cups if someone's throat dried up as often speaking about things can be anxiety provoking, and while we offered people tea on arrival not everyone took it, so having fresh water meant if someone did need a drink again, you were not leaving the room to go and find it.
I know there are probably online systems which can create flow diagrams better than a role of wall paper and hard copies! but there was something about seeing it all spread out in front of us (as it was very long and wound round the whole room!) which was so helpful, also when we cross referenced with people's experience of the service we learned so much.
What is so sad, is it was a constant battle for funding to keep that service going, an exhausting amount of effort in trying to find people to listen to what we had learned that may be of value to them to help address the challenges I heard they said they faced! I do sometimes wonder, that while on the one hand its all about talking about making things better, that challenging what exists means change and deep down there is a resistance to the level of change we need to take the actions needed to move forwards. If I can be of practical assistance with what you are seeking to do, please ask, as I do see the value in it.
Make sure and look after you too as being a change maker can be exhausting work, know though, there are people listening
Hilda :-)
Hilda Campbell MBE 8 Feb 2024
Hi
I am not sure if the contribution I could make would be of value. It comes from a holistic assessment co designed with the voices of lived experience around the goals they set for using the service cross referenced with the interventions offered to help support those goals and how we know they had been achieved. The professionals using the assessment and system of recording were part of the co design process to ensure the final system created also met their professional reporting needs. This was a service for people experiencing mental/emotional distress. Part of the overall package of support was also linking to other services where what we offered was not enough but in a way that support was integrated to avoid duplication and minimise the amount of time someone had to invest in appointments.
I am not sure if my contribution would be helpful as it focuses on the wider needs of individuals out with their medical condition, but which if not met can impact on recovery. But if you think I have anything to offer to help you put together your idea, please just ask
Kind regards
Hilda
Comments are now closed for this post.