Q Exchange
Count it out. Avoiding waste and preventing deaths in asthma.
- Proposal
- 2024

Meet the team
Also:
- Dr Anna Murphy, Pharmacist - Leicester University
- Dr Fran Gilchrist, Respiratory Paediatrician - Keele University
- Mrs Sadie Clayton, Consultant Nurse
- Professor Rob Horne, UCL
- Dr Simon Lea, UHNM
What is the challenge your project is going to address and how does it connect to the theme of 'How can we improve across system boundaries?
Asthma affects 1 in 11 people in the UK.
Children and adults with asthma rely on inhalers to keep their asthma controlled and treat flare ups. In the UK, most people use puffers (pressurised metered dose inhalers) to treat their asthma. However, patients, carers and people who help look after individuals with asthma don’t know enough about puffers.
Puffers still puff when the medicine is gone.
Inhalers will ‘puff’ for 60-70 times after the medicine is gone.
Puffers contain powerful greenhouse gases.
This propellant has a significant impact on climate change. Returning puffers to pharmacies allows safer disposal, limiting their climate impact.
A survey of n=508 asthmatics shows the scale of the problem. 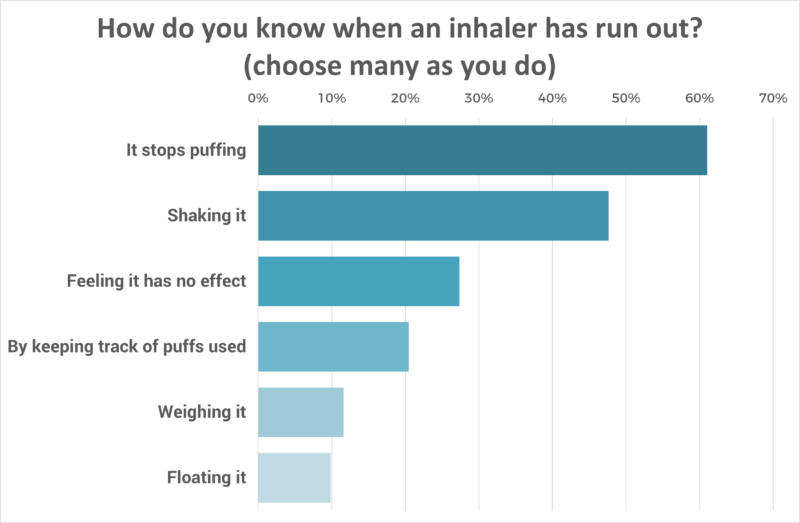
The answer is better cross-sectoral education.
We have launched the ‘count it out’ campaign. This is assisted with cheap monitoring devices. We want to work across system boundaries with schools and pharmacists to amplify these messages and measure our impact.
What does your project aim to achieve?
Objective 1. Reduce salbutamol usage and waste
In the UK, we use an astonishing 30 million salbutamol puffers annually. 36% are disposed of with more than half the doses unused.
By teaching children, parents and carers how their inhalers work and how to know when they are empty (or not) we hope to reduce the number of puffers used in our communities.
Objective 2. Reduce healthcare utilisation
This will also keep our patients safer, and reduce the risk of flare ups that lead to extra visits to the GP, ambulance call outs or hospital attendance. Using an empty preventer inhaler will worsen asthma control.
A child attempting to treat their asthma attack with an empty reliever inhaler is also likely to fail. 12% of children attending hospital have empty inhalers. This is dangerous.
Objective 3. Reduce health inequality
As asthma disproportionately affects children and adults from less advantaged backgrounds, then improvements will help address health inequality.
How will the project be delivered?
Our team.
Includes doctors, nurses and pharmacists with a track record of working and publishing in this field. This includes leading national work on creation of a Greener Prescribing Guide for Children with Asthma and the NHSE Children and Young Persons’ National Asthma Bundle.
Our partners.
Alongside the sponsor, we are already working alongside the NIHR-Schools Network to deliver research in schools. We have successfully collaborated with partners (Smart Respiratory) to secure low-cost dose tracking devices and develop Android and Apple compatible software that is already in use.
Low risk, high value.
All our costs are low. This makes scalability possible.
Accurate scales that allows us to check the amount of medicine left in a puffer cost £12. A reusable dose-counter costs £25. Education can be delivered to a school for less than £500.
We will use data from weighing returned inhalers and the new NHSE CYP Asthma dashboard to measure our impact.
How is your project going to share learning?
Sharing learning.
Our project has the potential to make a big difference if we can share the learning and replicate our model. It would be rapidly scalable.
The 30 million salbutamol inhalers used each year in the UK contribute the equivalent of 3.4 Billion miles of car journeys to climate change.
This number alone captures the imagination and attention of the media. We have already published in the Lancet on this topic. (1)
Demonstrating the power of cross-system collaboration.
By working with schools and pharmacies we will provide a blueprint for other Q members who hope to take a similar approach.
Harnessing technology.
Simple answers are often the best. People have not been counting out their medicine because this is difficult. We hope that by making it easier, we will succeed.
Reference:
- Carroll WD, Gilchrist FJ, Horne R. Saving our planet one puff at a time. Lancet Respir Med. 2022 May;10(5):e44-e45. doi: 10.1016/S2213-2600(22)00089-3. PMID: 35490695.
How you can contribute
- Do you like our idea? Please tell us if you do and how we can make it better. We like the words, 'Even better if'.
- Can you help us spread our message? We know how to tell if a reliever inhaler is empty, but lots of our colleagues and most of our patients do not. The Q community has an important role to play here.
- Do you know schools in the Staffordshire area who would like to take part? We are keen to talk with them about how we can make this proposal fabulous.
- Do you know any pharmacies that would be interested in working with us on this? We have contacts in the Midlands but would love to hear from colleagues across the UK.
- Are you generally interested in sustainable healthcare? If so, do you want to join our team and help?
- Do you have video or IT skills?
Plan timeline
| 1 Jul 2024 | Recruitment of schools and pharmacies via existing networks and NIHR |
|---|---|
| 1 Aug 2024 | Analyst to retrieve previous 12 months data from CYP Asthma dashboard |
| 17 Sep 2024 | Launch event for pharmacists at Wade Hall NSMI |
| 1 Oct 2024 | Rolling three month programme of training within schools |
| 5 Feb 2025 | Check in with Asthma dashboard are data present |
| 6 Mar 2025 | Check inhaler return rates and weight data with pharmacists |
| 10 Apr 2025 | Check in with schools - feedback from children and teachers |
| 11 Jun 2025 | Healthcare utilisation - Asthma dashboard interrogation |
| 16 Jul 2025 | End of year report from Schools - effect on asthma absences |
| 10 Sep 2025 | Sharing the data with colleagues across events |
Comments
Nuala Hampson (she/her) 28 Feb 2024
This is a great project to help people who need to remain on MDIs to use them more effectively. Will any element of your project include consideration of inhaler technique and whether patients would be more suited to DPIs, which have a much lower carbon impact?
In terms of sharing learning, you could consider approaching CPPE to get the learning about about how to tell if an inhaler is empty to their Inhaler technique programme for pharmacy professionals. This would help to ensure that learning is sustained beyond the project lifetime.
Best of luck!
Jenny Marshall 21 Feb 2024
This sounds like a really great idea. I haven't suffered asthma myself, but I have experienced friends with this condition, and I've often seen a blasé attitude towards their puffer. As you've identified, this is probably due to a lack of thorough education and explanation when first starting using a puffer as a child. I wonder if another low cost option to educate wider populations could be online teaching/videos? Maybe bitesize versions as reminders, and they could be age specific? I'm sure the Sheffield Children's Hospital would be interested in hearing about your work. Best of luck!
William Carroll 22 Feb 2024
Thank you so much. Yes, many good friends in Sheffield - and I will be reaching out to them.
Michelle Beattie 20 Feb 2024
Brilliant idea. I would be happy to help spread your message by incorporating it into our UG nurse curriculum in the Highlands of Scotland. Good also to see the consideration of impact on climate change. I think your pitch would be even better if you were clearer about which aspects of this work you would specifically be doing with the Q Exchange funds as it sounds like you are already doing lots in this area. Good luck with the work.
William Carroll 22 Feb 2024
Thanks. As you can probably tell - I was pushed for time in completing this and the budget plans remain very sketchy. I am hoping to add a lot more polish - and bring onboard a lot more team members.
Comments are now closed for this post.