Q Exchange
Understanding Delays and Busting Myths to Achieve Safe, Reliable Care
- Winning idea
- 2023
Meet the team
Also:
- Alison Lovatt, Director of Nursing, Improvement Academy
- Precious Keta, Person Centred Care Practitioner, Rotherham NHS Foundation Trust
- Dr Zuneera Khurshid, Implementation Research Fellow, Improvement Academy
- Alice Cunningham, Research Fellow, Improvement Academy
What is the challenge your project is going to address and how does it connect to the theme of 'How can improvement be used to reduce delays accessing health and care services'?
Organisations often focus efforts to improve access on discharge processes because it is difficult to fully understand where constraints lie within the system.
Delays are often accepted and normalised based on the capacity of the system to deliver rather than patient need. Not all delays are known, and known delays are not always reported or challenged.
Teams make assumptions about the causes of delays, believing them not within their gift to address which makes it difficult to empower and engage teams to improve delays.
ARCS is an evidence-based intervention developed with frontline teams at Doncaster Hospital. It brings all aspects of the patient’s plan in one place, highlighting what each patient needs and when they need it. ARCS captures each and every delay to patient care, exposing myths about where inefficiencies lie. Teams highlight delays earlier, contributing to a culture where delays are no longer accepted as the norm.
What does your project aim to achieve?
ARCS was used to plan the care of 2610 patients across nine wards at Doncaster Hospital. As a result patients spent less time in hospital and teams achieved a reduction in length of stay (range: 12% to 31%).
Our project aims to:
- Support frontline teams at Rotherham Hospital to adapt and adopt the ARCS intervention;
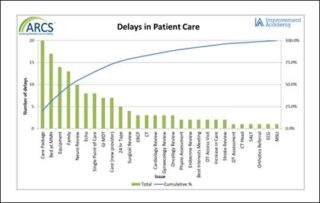
- Collect detailed information about each delay experienced, to understand constraints across different parts of the system. We will use the pareto principle to enable the organisation to direct attention to those areas causing the biggest delays;
- Empower and engage teams to address causes of delays that are within their gift to address and reduce length of stay;
- Evaluate the impact on outcome measures, including team working and safety climate and patient experience;
- Understand the barriers and facilitators to implementation, using the Theoretical Domains Framework, and share learning about how ARCS can be adapted using a bottom up approach.
How will the project be delivered?
The project will be delivered in partnership with the Improvement Academy and the Rotherham NHS Foundation Trust. We are a team of skilled improvers, supported by improvement and implementation experts with experience in supporting teams to adapt and implement interventions.
This project will be delivered using a bottom-up approach to engage frontline teams who will co-design tests of change (PDSA cycles) to adapt the ARCS intervention for their environment. This will be supported by executive leadership who will provide encouragement, assistance to unblock any barriers to implementation and share learning across the organisation.
Using the Stanford Lightning Report method (Brown-Johnson et al., 2019), an evidence-based, rapid qualitative analysis and feedback method, we will capture ‘what works’, ‘what needs to be changed’ and ‘insights’ to support adaptations.
Weekly operational meetings will monitor our risk log, with outcome measures being monitored at monthly steering groups to allow us to respond to problems efficiently.
How is your project going to share learning?
The ‘Lightning Reports’ produced through our evaluation approach will be shared at our steering group meeting every month which will act as a forum to share and respond to emerging evaluation findings in real time to fully support teams with their implementation efforts.
Teams are supported to embed data collection into routine practice which is then shared in a meaningful and accessible way to help engage front-line staff.
Achievement will be celebrated with frontline teams and wider within the Trust through their communications team.
We will share learning regionally through the South Yorkshire Integrated Care Board and wider through presentation at Improvement Academy’s Improvement Fellow’s network.
We will share learning nationally through updates on the Q website, membership of special interest groups and at Q events.
We plan to write up the project for publication and provide cases studies to share through social media and the Improvement Academy’s website.
How you can contribute
- We would like to hear from Q members that have experience in engaging patients, in particular evaluating their experience of waiting for care in hospital.
- We would also like your input as a critical friend.
Plan timeline
| 1 May 2023 | Communication campaign to engage and recruit 3 teams to Cohort 1 |
|---|---|
| 1 Jun 2023 | Cohort 1 Pre Implementation (Initial training and testing with team leaders) |
| 31 Jul 2023 | Cohort 1 Implementation (Cascade training and implementation with multi disciplinary team) |
| 14 Aug 2023 | Communication campaign to engage and recruit 3 teams to Cohort 2 |
| 28 Aug 2023 | Cohort 1 Sustaining phase (Capture and respond to delays in care) |
| 28 Aug 2023 | Cohort 2 Pre Implementation (Initial training and testing with team leaders) |
| 25 Sep 2023 | Cohort 2 Implementation (Cascade training and implementation with multi disciplinary team) |
| 6 Nov 2023 | Communication campaign to engage and recruit 3 teams to Cohort 3 |
| 20 Nov 2023 | Cohort 2 Sustaining phase (Capture and respond to delays in care) |
| 20 Nov 2023 | Cohort 3 Pre Implementation (Initial training and testing with team leaders) |
| 29 Jan 2024 | Cohort 3 Implementation (Cascade training and implementation with multi disciplinary team) |
| 26 Feb 2024 | Cohort 3 Sustaining phase (Capture and respond to delays in care) |
| 1 May 2024 | Complete evaluation report and disseminate learning |
Project updates
3 Apr 2024
Our Mid-Project Update
What we have learned so far – things that have gone well:
- We have a supportive Clinical Lead who has a great understanding of ARCS and who’s enthusiasm has helped us to recruit teams to the project.
- We have recruited a nurse who is an experienced project manager to support the implementation on site.
- We have nine Ward Managers that have volunteered to test ARCS with their teams.
- Of these teams we have one that has implemented ARCS and is currently using it to collect delays in patient care for all their patients. We are testing ARCS on a further three wards, including a short stay ward where the tool is being adapted to also support the introduction of criteria led discharge.
- Part of our evaluation uses the Patient Experience Toolkit (PET) to understand how ARCS affects the experience of patients. Patient interviews and thematic analysis have been completed with two wards.
- The Stanford Lightning report method has been extremely helpful in providing rapid qualitative analysis and feedback about our implementation approach. A research fellow, independent from the project team captures ‘what works’, ‘what needs to be changed’ and ‘insights’. This has helped us to adapt our implementation approach to provide more intensive support to teams in the testing and implementation phases.
What we have learned so far – things that have been challenging:
- Two of the wards that are testing have had a change in leadership due to unforeseen circumstances. The other two wards have also experienced annual and sick leave which has affected the availability of staff to lead the implementation locally. In hindsight, we spent too much time with teams that were not in the position to fully support implementation.
- The availability of key stakeholders has led to a loss of momentum. Delays in implementation mean that teams have not seen any tangible results from using the tool and this has influenced motivation.
- Integration with current processes is a significant barrier to engagement. Some teams already use whiteboards to keep track of some aspects of their patients’ care and the Trust also uses electronic whiteboards. Some staff perceive the ARCS board to be additional work that doesn’t seem to add value.
What others could learn from our experience:
Our project can provide learning opportunities for others looking to adopt initiatives that have been successful within other teams or organisations. There is a misconception in healthcare that if something works in one area of the system that it will be easy to implement and have the same impact in other areas. We knew that we needed to adapt the ARCS tool, but had assumed that it could be implemented in the same way. In practice we have found that we need to adapt our implementation approach not just the intervention itself.
Our next steps:
Our next steps are to evaluate the barriers to implementation. We will interview and survey members of the team currently using ARCS to get a deeper understanding of what is working well and what can be improved.
Based on our learning so far, we will test a modified approach:
- We will provide more intensive physical support on the ground to support teams. This will involve reassessing capacity and supporting fewer teams than initially planned.
- We will explore further opportunities to integrate ARCS into current systems and processes. This could mean adapting existing white boards to incorporate the principles of ARCS in order to collect information about delays in care.
- We will develop a ‘readiness checklist’ to help us to recruit the next team.
How the Q Community could get involved:
We would be interested in hearing from members of our community that could share:
- Any tools they use to assess readiness to improve.
- Any approaches they have found helpful when working with busy frontline teams who have competing priories for their time.
Comments
Vivian Ryan 11 May 2023
Hi Liz,
This looks really interesting. Would you be able to explain what the acronym ARCS stands for. I am looking at good tools to support with in hospital flow so would be interesting to understand a bit more about it.
Many thanks
Viv
Liz Watson 31 May 2023
Hi Viv
ARCS stands for Achieving Reliable Care for Safety. It is a tool based on Lean methodology which helps apply a standard approach to planning patient care. Rather than focusing on flow, we put the patient a the heart of the intervention, and promoting person centered care by focusing on 'what the patient needs AND when then need it'.
It is a very low tech intervention, which (to be honest) sometimes goes against it. The advantage of this approach is that aspects can be adapted to help teams to adopt it as their own, it is very cost effective and can be implemented quickly. Here is a link to a video which shows you it in action: https://youtu.be/p3NdmDcT64I
Please message me direct if you would like to learn more :)
Helen Crimlisk 23 Mar 2023
I love this project. The right care for patients when they need it and where they need it. Especially with a population with increasingly complex needs and comorbidity, a linear approach to follow up and care is inefficient and not good for patient experience (or the environment)
I'm interested to hear more about how you will capture experience and also whether there are sustainability gains to be achieved here too (and can we measure them?)
Liz Watson 28 Mar 2023
Hi Helen
We have given a lot of consideration to the question of how to measure patient experience. We have decided to use the evidence based, Patient Experience Toolkit (https://improvementacademy.org/programmes/patient-experience-toolkit-pet/) on a sample of our wards before and after intervention.
The toolkit will be used by our Research Fellow and to ask patients about their general experience of care on the ward. Thematic analysis will help us to identify for any themes specifically relating to waiting for care and communication of the patient's plan. We will then repeat the process after implementation of the ARCS tool to see if these themes have changed or improved.
I think there are sustainability gains to be made, especially as the organisation starts to build a visual picture about where the constraints lie across the while system and is able to respond to the areas of greatest concern. I think is will be difficult to measure, but the ARCS tool in itself can become a measurement for improvement. As interventions are developed and tested to address issues within the system, the success of this should be seen in a reduction of delays being reported by the frontline teams. For example, redesigning social worker processes should result in patients waiting less time in hospital for initial assessment as measured by ARCS. I hope that makes sense and that we are able to provide real examples through this project.
Joy Furnival 18 Mar 2023
I love this idea, and what results already from Doncaster! I really appreciate seeing a ‘spread’ idea in this list and I like th3 idea of your Evaluation Dress Rehearsal.
im curious if you could go further with your spread idea and cinder how you might be able to partner with other settings in your locality to test the same principles perhaps in a smaller way, eg in a mental health ward or community care setting too.
Good luck!
Liz Watson 28 Mar 2023
I also forgot to mention that we have adapted our evaluation approach. We will now be using the Stanford Lightning Report method, which provides even more rapid feedback to the implementation team. This means that rather than having quarterly dress rehearsals, 'lightning reports' can be shared at each monthly steering group meeting so we can respond efficiently to emerging findings.
Liz Watson 27 Mar 2023
Thanks Joy
We are keen to partner up with other healthcare providers to develop a greater understanding of the barriers of implementing this tool across different settings. In theory the tool can work in any setting, including non ward areas, such as teams who virtually manage patients through a pathway across different teams (e.g. discharge coordination, fractured NoF pathways).
We have spent time understanding the key principles of the tool, such as measurement at team level, and hope that this project will allow us to test which of these principles can be flexed, or adapted; and which need to be standardised to achieve the same impact. This will allow us to spread at a great pace in the future.
Comments are now closed for this post.