Q Exchange
Digital integration at primary-secondary care interface to streamline blood tests
- Winning idea
- 2020
Meet the team
Also:
- Paul Altman, consultant nephrologist, OUH
- Megan Morys-carter, Programme Director, TheHILL
- Marc Huglin, Operations manager, TheHILL
- Matthew Bottomley, renal registrar , OUH
- 2 Patients
- Jayne Haynes, GP representative
- second GP to be commissioned
What is the positive change that has emerged through new collaborations or partnerships during Covid-19 that your project is going to embed?
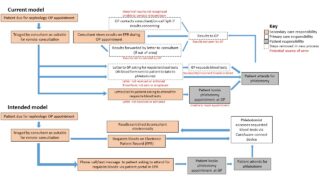
Patients with chronic health conditions including those with kidney disease are followed-up every 3-4 months. Pre-COVID, renal clinic appointments were face-to-face consultations and blood tests were performed then.
During the pandemic, we rolled out telephone/video consultations to minimise contact. Patients had blood tests either at Oxford University Hospitals (OUH) or at their GP practice.
Patient survey showed that 92% found telephone consultations effective but would prefer blood-tests at their GP practice. This requires the blood request forms to be posted to patients, creating an additional administrative workload and carbon footprint.
The results are returned to GPs for review rather than to secondary care . This results in duplication of work in primary care and delays in patient management.
Many patients with long term illness have multiple co-morbidities and require blood tests from different specialities. The current pathway requires patients to have multiple appointments to undertake these tests due to lack of IT integration.
What does your project aim to achieve?
The project aims to streamline the patient pathway for undertaking blood tests in the community to facilitate remote consultations. We introduce a new digital solution (CareAware Connect) that will link GP practices and Cerner Millennium- Electronic Patient Record (EPR) in secondary care. The blood test requests made in secondary care can be directly printed off at GP practices eliminating the need for paper request forms. This will ensure that correct tests are undertaken and results are sent electronically to secondary care reducing GP workload and delays in accessing the results. It also provides opportunity to co-ordinate blood tests requested by different specialities to be performed in a single visit and improve patient experience. We anticipate significant reduction in carbon foot print.
The project will assess the experience of using the device and the process change from a GP perspective as well as from secondary care, identifying any barriers to implementation.
How will the project be delivered?
We will pilot this within renal services and 15 GP practices within Oxfordshire. Clinicians will offer telephone/video consultations to suitable patients and request blood tests on EPR. Patients will be informed of the need for blood test by phone/text message via patient portal function within EPR. GP practice phlebotomist will use the CareAware connect device to scan the unique barcoded identifier card (each patient will be provided with one) to print EPR requests labels. Blood samples tagged with EPR labels will be sent to OUH for processing. The results are returned to the requesting clinician and to patients via patient portal.
We will evaluate its effectiveness through various outcome and process measurements including patient and health care professional satisfaction. Implementation will be through PDSA cycles to assess any barriers, mitigate risks and refine the new patient pathway. Carbon foot print evaluation will be undertaken by the UK Green Nephrology team.
How is your project going to share learning?
The project aims to test proof of concept using a simple digital solution. If successful, this project can be rolled out to other GP practices and OUH specialities. There is potential for other NHS trusts using Cerner Millennium to adopt a similar approach. We have consulted and received positive feedback from patients and GPs locally on this proposal.
GPs, patients and TheHill – Oxfordshire health and care digital transformation catalyst- will be active members of the project team. Results will be shared through OUH and Oxfordshire CCG blogs, patient forums, presentation at national meetings and peer-reviewed publication.
Communication via patient portal will empower patients to monitor their own results and co-ordinate blood tests required by several specialists during a single visit to the GP practice.
In collaboration with TheHill, there is scope for further innovation to replace the barcoded identifier card with smart phone apps to enable positive identification of patients.
How you can contribute
- Have other Q members faced similar problems organising blood tests in primary care and any feedback on our approach to solving this.
- Has any other member developed another digital or process change solution to this problem, or are you aware of one that exists?
- We would really appreciate your comments on patient portal. Does any other speciality routinely use such a system to communicate with patients directly?
- What QI measurements do members think would be important for this project?
- Is any member aware of a smart phone app that has the potential to interface with Cerner millennium?
- What are the perspectives / stakeholders we need to consider in this project (e.g. GPs, patients, commissioners, OUH staff)?
Plan timeline
| 11 Mar 2021 | Approve project plan, agree roles and responsibilities |
|---|---|
| 18 Mar 2021 | GP practices recruitment completed |
| 25 Mar 2021 | Phase 1 (Planning) -Process mapping workshop with all stakeholders |
| 8 Apr 2021 | Develop driver diagram |
| 22 Apr 2021 | Finalise QI measurements and methods of data collection |
| 7 May 2021 | Phase 2 (Set up) – Distribution of CareAware connect device printers completed |
| 14 May 2021 | Workflow development and online training tools for CareAware connect |
| 21 May 2021 | Recruitment of patients for project completed |
| 28 May 2021 | Provision of barcoded identifier card and patient portal registration completed |
| 4 Jun 2021 | Roll out training for CareAware Connect in GP practices |
| 18 Jun 2021 | Phase 3 (Implementation)– Pilot in 5 GP practices through PDSA cycles |
| 16 Jul 2021 | Interim project review and roll out to further GP practices |
| 15 Oct 2021 | End of implementation phase |
| 17 Dec 2021 | Phase 4 – Complete Data analysis |
| 18 Feb 2022 | Complete project write up for peer-reviewed publication and shared learning |
Project updates
29 Sep 2021
Unfortunately our project timeline has been delayed by 6 months
Challenges: The integration of the new technology ( CareAware) and associated software with our electronic patient record required trust management approval. Due to Trust competing priorities and COVID pressures, this has been delayed and we had just managed to get this approval last week. Contract agreements will now need to be signed off between the trust and the company and we hope to have this completed in the next 3 months. Our trust has also decided to use this technology within our hospitals for inpatient management for phlebotomy and medicines administration. This expanded application has broadened the scope of the project and will address patient safety issues.
Learning:
Don’t underestimate time required for trust senior management approval
Progress so far:
We have recruited 2 GPs and patients and a community phlebotomist as part of our project team. We have developed patient information leaflets, driver diagrams and have been working with out IT teams to develop data extraction routines for our QI measures. We have finalised data items for carbon foot print estimation in discussion with the Green nephrology team. We are currently developing staff and patient satisfaction questionnaires. We are working on developing patient ID barcoded laminated cards to be distributed to patients
Future Plans and timescales
Arrange stakeholder meeting and demonstration of technology once contract agreements in place ( Jan-Feb 22)
Project implementation from March-April 22
3 Mar 2021
We are making progress with getting the new technology approved by our NHS trust management and finance department. This is expected to be completed by end of April 21.
We are developing our process map , driver diagram and QI measurements whilst waiting for the trust sign off.
Comments
Shaine Mehta 14 Oct 2020
This is a such a useful idea - watching with interest as this is something we would look to do in our own area. GPs have been getting so many requests to for blood tests as a result of remote outpatient care. It's challenging as currently the bloods all come back to the requesting GP and this would help resolve this issue.
Be keen to hear how the integrating software works and any learning from use in due course.
Udaya Udayaraj 16 Oct 2020
Dear Shaine
Thank you for your positive feedback. As you mention, remote consultations in the COVID era has significantly increased primary care workload and it is important GP practices are adequately supported. We have been in touch with some our local GPs who share similar concerns and there is a great enthusiasm amongst GPs locally to implement this idea.
best wishes
uday
Deon Louw 2 Oct 2020
Excellent project proposal. Getting patient feedback would be crucial. I imagine it will be positive! You mentioned something about carbon footprint in your description. Have you considered promoting this as a Green Nephrology impact? See https://www.kidney.org.uk/green-nephrology. There's mention of promoting self-management by allowing patients to access their bloods. It should be simple to measure carbon savings for your project and gives it further benefits.
Udaya Udayaraj 6 Oct 2020
Dear Deon
Many thanks for your time reading through our proposal and for your excellent suggestion. We had previously evaluated reduction in carbon foot print with telephone consultations for kidney transplant recipients. Please click this link to see the paper that was published in BMJ. https://bmjopenquality.bmj.com/content/8/2/e000427.
As you say, it would be great if we could show wider benefits in the form of further carbon foot print reduction and patient empowerment. I have contacted the UK green nephrology team to seek guidance on incorporating carbon foot print analysis within this project. We certainly will be considering patient reported experience measures (PREM) and patient reported outcome measures (PROM) for the project and are recruiting patients to our project team.
best wishes
uday
Bethan Page 29 Sep 2020
This project sounds like it can simplify processes, save time for patients and GPs and give patients access to their own data/ blood results. Lots of positives. How are you going to evaluate? Can you quantify time saved for patients and GPs? Reduction in number of blood tests carried out?
Udaya Udayaraj 29 Sep 2020
Dear Bethan
Thank you for your comments. We would certainly be considering various outcome, process and balancing measurements in our initial project team meeting. One of the outcome measurements could be the proportion of blood tests performed correctly as per secondary care request. We know from current experience that certain blood tests are missed or cannot be processed because they are sent in the wrong tubes. We also intend to undertake a patient, GP and secondary care satisfaction survey to capture some of the metrics that you have alluded to.
best wishes
uday
Peter Dudgeon 17 Sep 2020
Hi Udaya and Sahana,
Myself and my colleague Emma Adams (Health Transformation Partnership) are supporting the Health Foundation this year by fostering conversations between Q members and encouraging collaboration. We were Exchange applicants last year, so we’re hoping that our experience will help us to help others, as their ideas take shape.
Having read your project idea, I applaud you for the way you've responded to patient need during this difficult time. I am not currently aware of others undertaking a similar challenge but will keep my eye out to help you make connections where I can.
I did have one reflection though, from recent work, engaging stakeholders to understand their needs. We have been recently been asking stakeholders to describe their needs thus .... As a ...... I need ..... so that ...... Asking questions in this way really helps to get under the skin of what people need and can hint towards the measures required to ensure that those needs are being met. Here's a link which describes more: http://www.iitoolkit.com/resources/stakeholders.html
If you'd like to know more about accessing this toolkit as a resource, I'd be happy to help. Best of luck.
Udaya Udayaraj 29 Sep 2020
Dear Peter
Thank you for feedback and sharing the toolkit with us. I have gone through this over the last few days and looks very impressive. I like your suggestion of ' As a ... I need... so that...' This is something I will look forward to using in our stakeholder meetings. We are in the process of recruiting some GPs and patients and clinical colleagues for the project and will certainly find your resources useful. Once again many thanks for sharing this with us. best wishes. uday
Comments are now closed for this post.