From advances in remote monitoring in sub-Saharan Africa to the implications of AI on health care systems, this year’s International Society for Quality in Health Care Conference (ISQua) presented a richly varied picture of emerging developments in improvement from a global perspective.
Q member Helen Crisp shares some of the highlights from the floor with Henry Cann.
1. The improvement world in one room
Helen: This was my nineteenth (!) ISQua conference since 2003, so it’s something of a highlight in my working year. This conference is a great way of cramming an annual update on what’s happening globally in quality improvement and patient safety.
It’s an opportunity to reconnect with friends I’ve made over many years in this field. At every conference, I continue to meet new people with new ideas and it’s still one of the friendliest conferences going.
Henry: Whereas this was my first ISQua conference! I was there to talk to delegates about our work on engaging staff, using Thiscovery.
There was something very humbling about seeing a room full of delegates from across the world facing a dramatic range of challenges – all committed to quality and improvement.
As well as feeling like a much bigger world, it simultaneously felt smaller to meet Q members there such as yourself and Jan Mackereth-Hill.
2. Smarter improvement and launch of a new toolkit
Helen: I started the Seoul conference co-presenting a workshop on ‘Smarter Improvement’ encouraging improvers to use a wide range of methods and approaches with fidelity! Our exercise around improving patient transport, car parking and physical access to health care facilities resonated with delegates from around the world and participants were soon stuck into developing driver diagrams.
Henry: I was there too, a great first session! Afterwards I attended a session where Tom Foley launched a new world first toolkit on Learning Health Systems. This has been supported by the Health Foundation, through Tom Hardie. There were so many other highlights throughout; I attended a great ‘world café’ run by John Brennan.
3. Bringing co-production into the consultation room
Henry: At their plenary session on co-production, Helen Leonard and Catherine Calderwood challenged delegates to think about how we planned to bring co-production back into our work. Indeed, co-production and the patient were a huge focus of the conference.
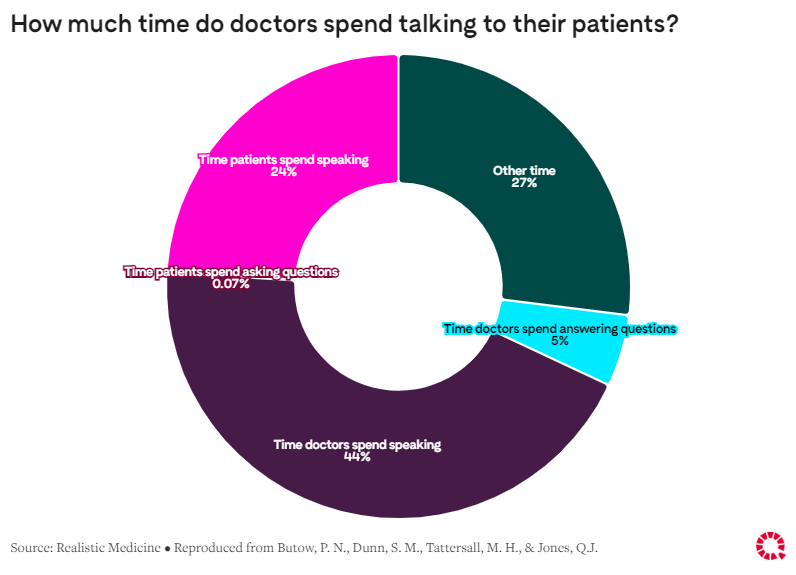
I was struck by some stats about the amount of time, in a typical consultation, that the patient talks compared to the clinician. According to research by Phyllis Butow, patients speak for 24% of the time and ask questions which take up 0.07% of the consultation time. In contrast doctors speak for about 44% of the time and spend just 5% answering patient questions.
Different studies show the average time it takes a clinician to interrupt a patient, most placing this in the range of 11 to 20 seconds after the patient begins talking to describe their issue.
A really stark reminder of the challenge for many patients in getting the most out of services particularly when, as we heard in one session, there is a continuing need to address low rates of public health literacy. One study found that 43% of English working-age adults will struggle to understand instructions to calculate a childhood paracetamol dose.
4. The opportunities (and challenges) of Artificial Intelligence, tech and data
Helen: This year’s conference had a very timely emphasis on use of data and automation; and the implications of Artificial Intelligence (AI) for health care. In a number of sessions, care providers reported on their experience of remote consultations, the speed of implementation and whether or not it has been sustainable.
They also explored the gap between patient and staff experience of implementation, echoing the Q work around engaging staff well in change.
The UK has a lot to learn from the international experience. For example, we heard about providers of community health care in sub-Saharan Africa making great strides with remote monitoring via mobile phone apps. As well, the conference heard about health centres in the United States reaching out to communities with poor access to care via telehealth and how AI is transforming hospital care in Israel.
Henry: As you say there was a focus on the use of data, specifically around patient and public understanding and trust around data collection. This is definitely something I worry about. As an analyst and evaluator, I think we often do a poor job of communicating reasons for our data collection.
In general, I think we often collect far too much data and we need to consider how data collection can be more targeted and purposeful.
Integration and collaboration between agencies not used to working together – such as those in England’s Integrated Care Systems – is another area where trust is going to be key to success.
5. Frailty support and implications for long term care
Helen: On the last day of the conference, I presented results of a frailty support pilot project from Lewisham, South London in a session with presentations from Denmark, Armenia, Taiwan and the United Kingdom. Each project stimulated thinking around long-term care support, meeting individual needs from a unique perspective.
One of the shared challenges that surfaced in this session is how to ensure projects don’t briefly bring some extra resources and then disappear again. In the final plenary, we were challenged to think about what we had learned and, importantly, what we were going to change in practice as a result.
A very unexpected conference finale saw us dancing on the stage. This was a spontaneous expression of the joy and friendship we found in coming together to share ideas to improve quality and safety in health care.
6. Remote care and telemedicine
Henry: Earlier, you mentioned remote consultations which is one of my interests as well as an area of Q’s ongoing work. As you noted, there is evidence of a gap between staff and patient experience of remote consultations. The conference presented some of the challenges to uptake of telemedicine, including quality of care.
A key point raised during this session was the need to have a clear legal framework for telemedicine in place, so that the workforce do not end up becoming antagonistic to this practice.
We know from the evidence that the most successful quality improvement projects are those where staff are empowered with the information and skills they need to make the necessary technical and culture shifts.
Next steps
Henry: It feels a long way away but do you think you’ll be there again next year for your twentieth?
Helen: Planning is already underway for the 2024 conference in Istanbul. Organisers are thinking about how they can respond to Seoul by offering even higher impact plenary sessions and giving as many improvers as possible the chance to present their work in short talks and posters. Will I be going? You couldn’t stop me!
Henry: Love to hear it. I do think, as you said earlier, there is a lot that the UK can learn from work internationally. And although this isn’t why I travelled out there, I couldn’t put a price on the connections made and possibility of future collaborations. I hope someone from the Foundation will be in Turkey next year, even if it’s unlikely to be me!
See ISQua’s plans for the 2024 conference in Turkey
Read more about question asking behaviour during consultations
Find out more about Scotland’s plans to address the hidden problem of poor health literacy
Comments
Sarah Andersen 17 Oct 2023
Thank you for this - sounds like a great conference. I particularly liked the image of a spontaneous dancing finale!
One question I have is : was there a thread of environmental ( as well as financial) sustainability running through it? Will this be a focus at the next International Quality in Health Care conference in Turkey?
Helen Crisp 17 Oct 2023
Hi Sarah, Yes, there was a thread on environmental sustainability at the ISQua conference 2023 and it's likely to be more prominent at the 2024 conference in Istanbul. The call for papers will be looking for abstracts on 'Navigating climate change and sustainability in health care' so that should generate some very relevant content.
Sarah Andersen 9 Nov 2023
Thank you Helen, yes, sounds like you will be addressing it head on by asking for papers on exactly that issue. I look forward to following the outcomes from that.