Q Exchange
Transforming Transition for Young People with Complex Needs and Disabilities
- Proposal
- 2024
Meet the team
Also:
- Dr Hemavathy Palanyiaya, Consultant in Neurodevelopmental Paediatrics, Evelina London Children's Services
- Dr Ella Hubbard, GP trainee
- Dr Emma Parish, General Paediatric and Adolescent Consultant, Evelina Children's Hospital
- Dr May Yip, Consultant Community Paediatrician, Evelina Children's Hospital
What is the challenge your project is going to address and how does it connect to the theme of 'How can we improve across system boundaries?
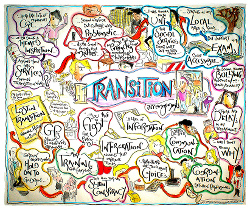
Transition from paediatric to adult services is a very challenging time for young people with learning disabilities (LD) and complex medical needs. For these young people, transition is complex and requires moving across system boundaries in multiple services. This is isolating, confusing and often worsens health inequalities.
In Southwark and Lambeth, our young people and their families are navigating transition from a point of disadvantage, with high levels of deprivation and low levels of health literacy. These young people face additional barriers at each moment of transition, and are particularly vulnerable to falling through the gaps or being left behind, exacerbating existing health inequalities and adverse health outcomes.
The handover of overall oversight of a young person’s care from community paediatrics to general practice (GP) is frequently done informally, incompletely, and fails to equip primary care to fully support young people with LD as they move into adult services.
What does your project aim to achieve?
Our aim is to develop a model of best practice for the transition of care for young people living with LD and medical complexity.
In this project we will:
1. Use patient journey mapping to co-produce a toolkit of resources with young people, families and GPs to evaluate current practice and improve the holistic care provided to those with LD, and to provide a framework for annual LD reviews from age 14 years before transition.
2. Co-design and pilot joint transition clinics with community paediatrics and general practice to support the ‘handover’ of care of young people with LD and medical complexity.
3. Training days with primary care MDT to support their learning on children with complex needs.
We will focus on our local area (Lambeth and Southwark), while developing a model of best practice which can be shared nationally. This will improve integrated care, patient experience and outcomes, whilst reducing health inequalities.
How will the project be delivered?
The team is comprised of 2 Consultant Community Paediatricians, PCN community paediatrics lead, a GP trainee and a researcher in child health.
The clinical lead for the project is a consultant in neurodevelopmental paediatrics who will lead the work to develop a model for joint transition clinics, whereby the annual LD review is undertaken collaboratively by both a GP and a neurodevelopmental paediatrician in the four years preceding a young person transitioning to adult services.
Researcher Bethan Page will support with coproduction and evaluation.
We will use funding to pay for a GP training fellow to support our team member Dr Ella Hubbard (GP) to help plan the two training and engagement days for GPs. Their engagement will be critical for building on our existing relationships with local GP practices.
This project builds on existing work we are doing to improve coproduction and joint working between community paediatrics and primary care.
How is your project going to share learning?
At the completion of the project, we will share the following outputs:
– A toolkit of resources for general practices to evaluate their current LD provision, ensure the identification of those with LD, and improve the quality of LD annual reviews
-Educational resources targeted at the wider multidisciplinary team in primary care to improve the understanding of the ongoing complex health needs in patients with LD
-A model for how joint transition clinics can be conducted across primary care and community paediatrics
We will use the Q community to help us understand the relationship between the local and national picture, and to share learning with other clinical areas working to improve transitions for young people to adult services. We will particularly seek to share learning with clinicians working in areas of high deprivation nationwide.
We will present the work to relevant clinical networks, e.g. British Association of Childhood Disability (BACD).
How you can contribute
- Anyone with experience of transitions for young people with learning disabilities and complex needs who could share learning from your local area.
- Teams with experience of transitions in other clinical areas, e.g. transitions for young people to adult services in mental health
- Engagement from primary care. This project will support primary care to meet the NHS national objectives for 2023/23 includes ensuring that “75% of people aged over 14 on GP learning disability registers receive an annual health check and health action plan by March 2024” (https://www.nhsconfed.org/publications/202324-nhs-priorities-and-operational-planning-guidance).
Plan timeline
| 1 Jul 2024 | Co-production of Transition Pathways and Toolkit with families and clinicians |
|---|---|
| 1 Aug 2024 | GP Education and Event Organisation begins |
| 1 Sep 2024 | Refinement of Transition Pathways and Toolkit |
| 1 Nov 2024 | Joint Outreach MDT Clinics begin alongside evaluation |
| 1 Dec 2024 | GP Education and Support : first event held |
| 1 Feb 2025 | Second Round of MDT joint clinics |
| 1 Mar 2025 | Evaluation analysis of MDT joint clinics and GP training day |
| 1 Apr 2025 | Preparation for National Symposium/conference to share learning |
| 1 May 2025 | Second GP training day |
| 1 Jul 2025 | Share learning at national symposium/conference |
Comments
Katie Lean 20 Mar 2024
Bethan,
You and your team are addressing a really important group of young adults who often are marginalised. It's so important that you are focusing on a co-design approach. A well thought through project.
I wish you all the best in it.
Bethan Page 20 Mar 2024
Thank you Katie- codesign approach is definitely the way forward on this! We did a day recently at a special educational needs schools to work with parents on transitions, with different stalls representing different medical teams, social care, charities etc. So critical to work across these different boundaries!
Mary Salama 19 Mar 2024
Really love this idea Hannah and Beth
The care of children with complexity is difficult in any circumstance but we know families find the transition between different systems particularly difficult. Add to this a variation in boundaries in many services and it can leave even the most experiences parent-carer stranded. Well done on looking at this important issue. Myself and all my colleagues on the colab partnership committee will be watching it with interest. Good luck!
https://www.colabpartnership.org.uk/
Hannah Zhu 20 Mar 2024
Likewise - love your Canal project proposal and so exciting we're both growing and continuing the work of Powering Up! https://q.health.org.uk/idea/2023/powering-up-co-producing-solutions-to-health-inequality-with-young-people/
Have heard the schools presentation was brilliant last week and definitely keen to keep working together and learning from you :)
Bethan Page 20 Mar 2024
Thanks Mary- we are very keen to link up with your Powering Up project and learn from your work on coproduction with families! We will definitely share updates with the colab partnership if we get funded so we can share learning
Bethan Page 19 Mar 2024
This team of clinicians are already doing excellent work to improve transitions for young people in South East London, including running a really helpful transitions event for parents and young people last year in a special educational needs schools. I am really looking forward to working with them to support with evaluation and coproduction with families in my role as a researcher. They are a really dedicated team with good existing links across boundaries with primary care, social care, schools etc. There are so many services involved in the care of children with complex medical needs, we need to work across many boundaries to improve transitions to adult services.
Guddi Singh 18 Mar 2024
This is a fantastic project proposal! An important and hard-to-solve problem for a neglected cohort of patients. I also love that it places young people and service users at the heart of the change idea.
There are huge commonalities of approach and ethos with WHAM's Powering Up project and also another bid in this year’s exchange by Mary Salama and team, who are looking to link across GP and paediatrics better. It might be worth linking up to expand your thinking and reach, not to mention that we, at least, would be delighted to share our findings in case they are useful for you to build on.
Some questions to think about:
Wishing you luck with this and do stay in touch!!
Guddi
Bethan Page 19 Mar 2024
Thank you so much Guddhi. Some responses from our team:
• How will you recruit the young people who are ‘most in need’?
1. A few of the clinicians organising this project currently run regular clinics at a special school in a highly deprived area, which caters for young people (YP) with moderate to profound intellectual disability. We intend to identify the young people ‘most in need’ through these clinics based on their socioeconomic background and specific challenges they may face. We will engage their parents/carers (either through parent carer forums or contact in clinic) in the process from the beginning. This would involve explaining the purpose and benefits of the programme and how their involvement can make a difference. We hope to conduct workshops with parents/carers and young people to facilitate co-production of the programme, to gather their ideas and understand their needs. We also aim to provide the necessary support to these YP and their parents/carers throughout the process through appropriate signposting.
• What is your strategy for making co-production events as inclusive as possible (e.g. for those with disabilities or neurodiversity)
1. We will provide support for YP with communication difficulties through use of visual aids, sign language interpreters or speech to text technology. If required, we will utilise the necessary AAC (augmentative and alternative communication device) to promote inclusivity.
2. We will involve parents/carers in the planning process and ask for their input on how to make the events more inclusive through parent forums.
3. We will ensure the staff and volunteers are trained in disability awareness and can provide proper support and adjustments as needed.
4. We will plan inclusive activities by planning activities that can be enjoyed by all YP regardless of their disabilities.
5. We will ensure that the venue is accessible to all with disabilities.
• Is there a plan for how you might ‘embed’ the changes in the long-term?
1. We recognise that transition is a very stressful period of time for parents/carers and poor transition is associated with poor health outcomes, especially in YP with complex health needs. We hope to embed the initiatives introduced through this project into regular clinical practice to improve transition in the long term, and resultantly future health outcomes. We will conduct regular educational events on transition jointly with the primary care network and adult services, and look to have joint transition clinics going forward. We hope to collaborate with other services locally and nationally, to exchange ideas and provide a platform to generate discussion about findings and outcomes achieved through similar initiatives
• Have you seen the AYPH material on youth co-production and health inequalities?
It's brilliant! Yes indeed, this is very relevant to the population of YP we are serving! It would be great to hear more about your work. I will be at the RCPCH conference next week on the tuesday and will come and find you- i believe you're presented the WHAM work!
Nikki Davey 15 Mar 2024
This is a challenge that paediatricans flag up regularly that they feel needs to be improved. They see the glaring gaps and have to pick up those who fall through them every day! It great to see this initiative focusing on outreach into primary care - where the majority of children receive the majority of their care. I know that Hannah has a great track record of using QI to make change happen AND that she is great at engagin young people in co-deisgn too.
Hannah Zhu 19 Mar 2024
Thanks so much Nikki and also for your ongoing wisdom with my projects. I'd encourage anyone with paediatric trainees in or near London to encourage them to sign up for Nikki's QI course, which supported my first health inequalities QI project: Improve ONE thing:The Full QIPOPEN CourseSpring 2024 - QIClearn
Hannah Zhu 15 Mar 2024
Meaningful coproduction with primary care, young people and families will be key to the success of this project - we are starting to set up links with the PCN networks and learning from other coproduction groups locally. Please let us know if you have any advice or local contacts?
Bethan Page 15 Mar 2024
Thanks very much for your comments Jenny. We just had a project meeting with the team to refine our ideas. We think there will be plenty of learning from the project on transitions for other areas like mental health- as you say, the pathways are unclear and people fall through the gaps. We plan to share the learning with the q exchange, perhaps through a webinar and blogs discussing the issues of transitions. Do reach out if you would like to chat!
Jenny Marshall 5 Mar 2024
Hi Bethan - I'm really interested in this idea and would love to see how this progresses. Transition from child to adult mental health services often has an unclear pathway, and unfortunately there are cases where individuals fall through the gaps. It would be great to see how you get on with this project and whether it can be scaled up to include other mental health transitions. I really like the idea of providing a toolkit for internal evaluation - are you planning to gather this information from the practices and review any changes/progress?
Comments are now closed for this post.