Q Exchange
Safe sitting with pressure ulcers, from acute to community setting
- Proposal
- 2024
Meet the team
Also:
- Dr Mark Bowtell (Principal Clinical Scientist)
- Kelly Jones (Rehab Engineer)
- Susan Flavin (Nurse Specialist)
- Dr Lorna Tasker (Head of Rehabilitation Engineering)
- Eleri D’Arcy (Quality priority lead)
- Ward staff
- Rachel Govier-Williams (Lead TVN)
- Susan Learmonth (Locality Lead OT)
What is the challenge your project is going to address and how does it connect to the theme of 'How can we improve across system boundaries?
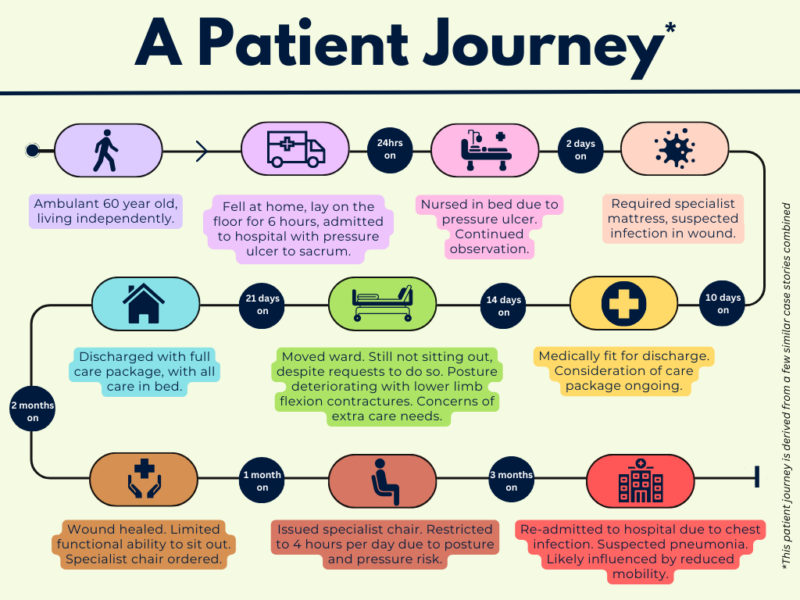
Inpatients with pressure damage can remain restricted to bed for longer than necessary due to lack of expertise, confidence and suitable equipment. Implications in deterioration of posture and function are often irreversible, leading to avoidable health complications. Without specialist input, patients experience poor health outcomes, further deconditioning and multiple readmissions.
The socioeconomic impact of pressure ulcers is extensive, spanning health and care settings. SBUHB has seen an increase in pressure ulcers (~97 per month). NHS Wales’ 6 goals for urgent and emergency care prioritises ‘optimal hospital care’ recognising timely discharge as pivotal to a patient’s recovery.
Many inpatient stories evidence a lack of progressive care, resulting in higher demand within social care and prolonged health involvement. Demand for spread of our specialist posture and seating service is evidenced through referrals received to-date. Here presents an opportunity to improve health outcomes as well as relieving system pressures across sectors.
What does your project aim to achieve?
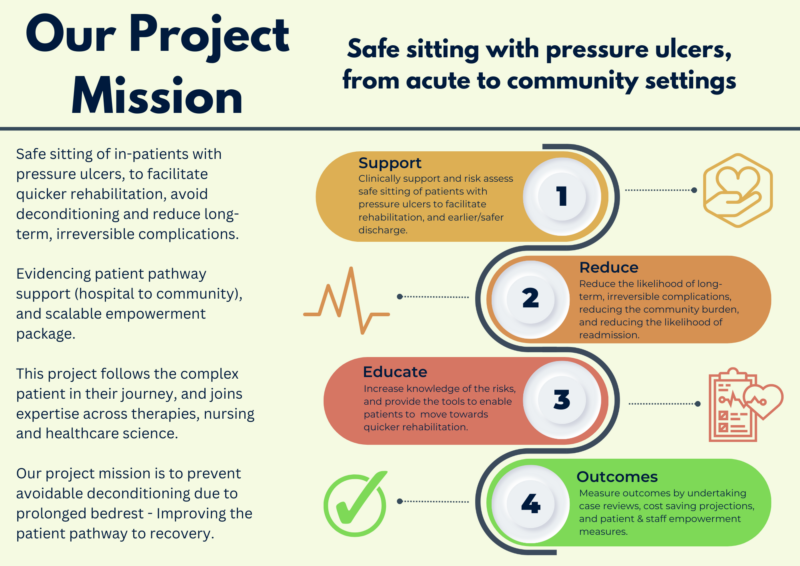
The Pressure Ulcer Prevention Intervention Service (PUPIS) currently supports patients in the community with pressure ulcers that aren’t healing due to difficulty offloading the underlying pressure. This involves supporting those patients with a safe sitting regime and equipment check following surgery. We want to spread this expertise to patients rehabilitating from acute immobility, throughout our hospitals.
This project follows the complex patient in their journey, and joins expertise across therapies, nursing and healthcare science.
Mission to prevent avoidable deconditioning due to prolonged bedrest. Primarily, we aim to translate our existing service to inpatient care with clinical support in safe sitting of patients with pressure ulcers to facilitate rehabilitation, and earlier/safer discharge. This will reduce the likelihood of long-term, irreversible complications (patient harm), reducing burden on community and reducing likelihood of readmission.
A wider aim is to educate the risks and provide tools to enable patients towards quicker rehabilitation.
How will the project be delivered?
- Launch a campaign to communicate the risks of prolonged bedrest.
- Analyse data to demonstrate the challenge and the value of intervention.
- Empower ward teams with equipment choice and risk assessment tools.
- Reduce waits to leave hospital by promoting more functional, healthy, community-ready patients.
We will fund excess hours to enable the team to project manage, seek patient goals, educate, measure and report.
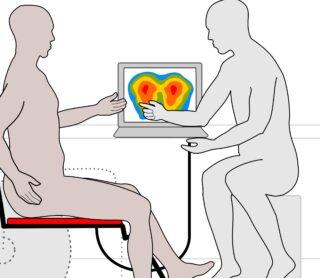
Clinically, we will utilise our specialist knowledge with pressure ulcers and seating, expertise to risk assess with interface pressure technology, provide special seating solutions and manage sitting regimes.
This project will allow us to better link community and acute settings (equipment, discharge planning, follow up). We believe that those with pressure damage and related complexity need to be supported through their health and social care journey, and we are ideally positioned to evidence this model.
Measuring impact will include case reviews, cost saving projections and patient / staff empowerment.
How is your project going to share learning?
· Share experiences of working across boundaries of profession, service and healthcare setting.
This project builds on expertise from various professionals and services, from the strategic lead of therapies supporting equipment provision, to the staff nurse reviewing wound improvement. We have wide support in our health board for this initiative from leads in Tissue Viability, Occupational Therapy, Nurse Directors and Director of Therapies and Healthcare Science.
· Demonstrate and evidence a model with potential to impact patient flow in all hospitals across the UK.
The pandemic affected our field particularly with increase in pressure ulcers, increased postural complexities, and reduced rehabilitation potential for our complex user groups. It also affected cross-working between services, with many restricting referral criteria and being less willing to fill the blurry gaps.
How you can contribute
- Support shaping the final proposal to best fit challenge, honing in on most appropriate measures and scale opportunity. Q-community role could specifically be:
- · The critical friend – help challenging method to ensure best approach
- · The Promoter – support to promote the progress and share learning
- · The fixer – assistance to look at funding restrictions long term to address scaling required
- · The collaborator – understand what other services available
Plan timeline
| 3 May 2024 | Baseline data collection, develop engagement package |
|---|---|
| 7 May 2024 | Scoping, stakeholder engagement, Q-community expertise |
| 1 Jul 2024 | Clinical support initiation, disseminate engagement package locally |
| 11 Nov 2024 | Mid-point review and report |
| 3 Feb 2025 | Finalise data |
| 3 Mar 2025 | Final report |
| 7 Apr 2025 | Disseminate engagement package nationally |
| 1 Sep 2025 | Gather learning from national engagement |
| 6 Oct 2025 | Share learning with Q-community |
Comments
Eleri D'Arcy 13 Mar 2024
This looks like a really good project. Benefits will be felt to individuals, health and social care and really encompasses a patient centred full system approach to those patients most at risk of deterioration.
Mark Bowtell 13 Mar 2024
This looks remarkably valuable, and fitting for this call of the Q-exchange
Mandy Westcott 29 Feb 2024
Extensive thought is evident in the idea.
Comments are now closed for this post.