Q Exchange
In-house Development of Mental Health Apps
- Proposal
- 2024
Meet the team
Also:
- Dr Dave Rogers, Consultant Clinical Psychologist, Psychological Therapies Service.
- Jane Reynolds, Mental Health Manager, Causeway GP Federation
What is the challenge your project is going to address and how does it connect to the theme of 'How can we improve across system boundaries?
The NI Mental Health Strategy stipulates that local Trusts should develop and implement a comprehensive digital mental health model to deliver services at all steps of care. To achieve this, and reduce waiting lists, we plan to work collaboratively with Primary and Secondary care teams to develop in-house Mental Health Apps (Apps). These can reach large Community based audiences, offering evidence-based alternatives to 1-1 therapy, support to those on waiting lists, and adjuncts to existing therapy. Existing Apps are of mixed quality and need frequent updating to keep up with the evidence-base.
Building expertise in “No-code” platforms and other in-house solutions would allow clinicians to control release dates and flexibly update App content without expensive 3rd party suppliers, or coding skills needed to develop, deploy and update Apps.
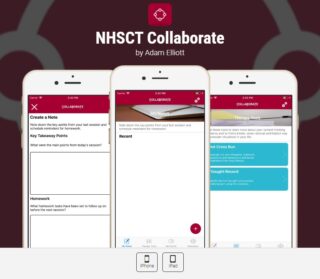
We have had positive feedback from service users on existing digital mental health projects (e.g. NSFU website; Collaborate App).
What does your project aim to achieve?
- Training and upskilling of our workforce to enable clinicians to independently create, deploy and maintain Apps using “No-Code” platforms over a 10-year period.
- Deployment of our existing, adjunctive App (Collaborate) to iOs and Android platforms.
- Joint training of clinical staff to implement this and support service users who opt for Digital interventions.
- Diversification of effective, accessible and acceptable interventions leading to enhanced capacity and flow.
- Additional support for those waiting on or engaging in therapy to boost readiness for therapy.
By diversifying our suite of interventions, free, remote and highly accessible standalone digital options can be delivered to a proportion of the population. which may suit those living in rural areas, or groups that avoid services due to practical obstacles such as childcare or perceived stigma around Mental Health.
These interventions should reduce treatment duration enabling clinicians to move quickly and effectively through our waiting lists.
How will the project be delivered?
Our team includes representatives with Level 2 & 3 QI, project and technical skills from the Psychological Therapies Service and Causeway GP Federation. This will be co-produced and co-designed with service user / staff focus groups to inform the project.
Using QI methodology, we aim to achieve the ability to independently create digital interventions for use across sectors. Waiting list numbers and waiting times, experience of time on waiting list, number of App downloads, and outcome evaluations will assess improvement, whilst service-related research conducted will assess effectiveness, accessibility and acceptability.
A typical 12-18 sessions of 1-1 therapy incurs costs of £3000-£4500. If only 6 service-users (a very conservative estimate as annual referrals >2000 individuals) opted to use the App for therapy instead, 6*£3000-£4500 (close to or exceeding our projected costs of £18,400) could be reinvested back into the service.
To manage risk, Apps will include support services. Service users may be given an option of further support from an Assistant Psychologist.
How is your project going to share learning?
We would intend to make this App usable free of charge across all Health Care Trusts, and share our experience of independently designing and developing software solutions.
Research (RCT) and project evaluation (QI) would be undertaken to enable service users’ anonymised experiences to be assessed. Results would be published in peer-reviewed journals and shared via the Q Community
Learning from the project process, not just outcome, will also be shared across the national and regional QI forums, such as the Q Community and HSCQI, offering site visits and feedback sessions as opportunity arises. QI methodology will feature heavily, with poster presentations including run charts, process maps and driver diagrams to be shared at appropriate fora.
How you can contribute
- Previous experience of MH App design
- Experience of “no code” platforms
Plan timeline
| 13 Apr 2024 | Use funding to launch existing version of App |
|---|---|
| 1 May 2024 | Set up project team |
| 1 Jun 2024 | Identify preferred 3rd Party/No Code platform |
| 1 Jul 2024 | Create wireframe of App; feedback from staff and service users |
| 1 Jan 2025 | PDSA 1: launch app with PTS clinical population and gather feedback |
| 1 Jul 2025 | PDSA 2: launch app NHSCT-wide and with Primary Care (gather feedback) |
Comments
Jacqueline Morton 15 Mar 2024
Adam how will you capture service user engagement and impact of this approach whilst maintaining anonymity?
Comments are now closed for this post.