Q Exchange
Improving Clinical Nutrition Services provided to Cancer Outpatients at SHSCT
- Proposal
- 2024
What is the challenge your project is going to address and how does it connect to the theme of 'How can we improve across system boundaries?
Nutrition is highly important for cancer patients across their trajectory of care from the period of diagnosis, treatment and beyond into survivorship and in palliation. Research shows dietetic interventions can be correlated with improved QOL, prognosis, treatment tolerance, reduced toxicities and reduced unplanned admissions.
Currently patients attending the Chemotherapy unit in SHSCT are screened for malnutrition however due to limited capacity and funding patients have been referred out to community services resulting in long waits of up to 274 days for dietetic assessment. A lack of specialist Dietetic input at the point referral puts our patients at a disadvantage when it comes to the prevention of malnutrition, outcomes and experience during their SACT.
Enhancing care and experience for these patients is crucial to prevent complications of malnutrition, optimizing QOL and ensuring we are meeting regional standards that align with best practice that is offered across the boundaries of other trusts.
What does your project aim to achieve?
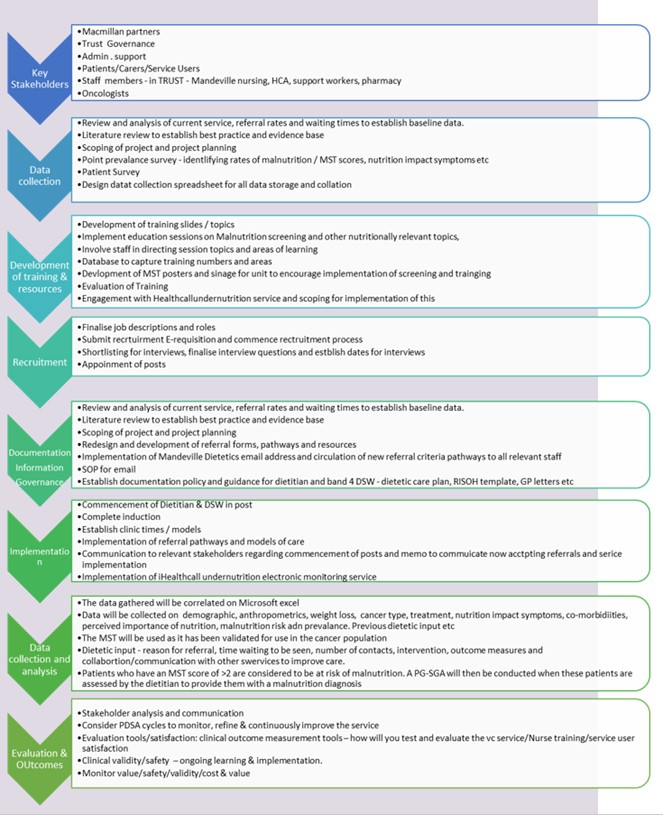
Aim: improve the Clinical Nutrition Services provided to Cancer Outpatients attending the Mandeville Unit within the SHSCT.
We to conduct a needs assessment to identify the most appropriate means of nutrition service delivery to cancer patients of the MDU and assess the benefits of piloting a consistent standard of care by a specialised oncology dietitian and dietetic support worker, in addition to the implementation of the digital monitoring Healthcall Undernutrition service.
Through co-design with stakeholders, our service model will provide specialist dietetic input for cancer patients undergoing treatment at the SHSCT MDU, incorporating an interdisciplinary approach, enhancing productivity, efficiency and quality of practice in the unit, aiming to bolster partnership working between dietetics, members of the oncology MDT and service users and their families. We aim to improve timely access to dietetic assessment and intervention and reduce inequitable delays for our patients requiring nutrition support during their journey.
How will the project be delivered?
Develop a systematic approach to identification of malnutrition and malnutrition risk with the use of the MST.
Pilot increase FTE funding with Specialist Dietitian and DSW. Address model of care; provide all patients referred to the dietitian with specialist dietetic assessment and intervention; include blanket referrals for high risk cancer streams, improve malnutrition screening and codevelop, & deliver education sessions to MDU staff.
Implement health call undernutrition service –monitoring service for patients in their own homes, allowing remote monitoring reaching those in all areas within the trust
Surveys to obtain service user feedback and staff perceptions. Ensure that a well-considered approach, involving relevant stakeholders at critical points, measuring impact, delivering value for money, and managing risk. PDSA cycles will be used to start the roll out of the service and regular feedback will be sought from stakeholders at early stages to allow for changes to be made.
Evaluation once implemented
How is your project going to share learning?
All activity will be shared through the relevant Q Community members and specialist interest groups
We will aim to build connections through social media and the Q Community by regular engagement and learning from feedback.
We will submit our results and outcomes as abstracts and presentation to relevant to conferences locally and nationally– eg BAPEN, to share learning across the region.
We will share progress and learning through formal trust governance channels, steering groups and leadership forums. Outcomes will be presented with relevant partners such Macmillan and NiCAN, to enhance proactive links to local or national priorities and structures.
Any service models and guidance documents developed will be available for sharing and disseminating locally and regionally through Q Community and stakeholders. This project model could be adapted and implemented in other adult dietetic services demonstrating the potential for our insights and interventions to be scalable.
How you can contribute
- QI Learning
- Specialist evaluation skills/advice
- Ideas on how to share learning
- Feedback on similar implementation - learning and ideas for going forward
- Do others have a model of care that works well – benchmarking best practice in other services nationally.
- Advice on improving this idea is very welcome – all feedback is beneficial
Plan timeline
| 4 Dec 2023 | Scoping and project planning. Review and analysis of current service |
|---|---|
| 6 Dec 2023 | Engagement with stakeholders – Mandeville unit, Nursing, Macmillan etc |
| 14 Dec 2023 | Development and delivery of nursing education |
| 21 Dec 2023 | Implementation of Mandeville Dietetics email address |
| 22 Dec 2023 | Circulation of new referral criteria pathways/forms to all relevant staff |
| 31 Jan 2024 | Engagement with Healthcall undernutrition service and scoping for implementation |
| 6 Feb 2024 | Finalise details for implementation of electronic monitoring service |
| 4 Mar 2024 | Development of audit proforma for point prevalence and patient survey |
| 8 Apr 2024 | Conduct point prevalence and patient survey |
| 15 Apr 2024 | Finalise Job description & personnel criteria for posts |
| 29 Apr 2024 | Implementation of electronic monitoring service for current priority referrals |
| 6 May 2024 | Completion of induction manual, best practice guide and induction plan |
| 3 Jun 2024 | Determine/finalise funding for posts |
| 17 Jun 2024 | Commence recruitment process |
| 12 Aug 2024 | Conduct interviews for Band 7 dietitian and Band 4 DSW |
| 1 Oct 2024 | Commencement of staff in post and begin induction |
| 7 Oct 2024 | Communication to relevant stakeholders regarding commencement of posts |
| 4 Nov 2024 | Memo to communicate now accepting referrals and service implementation |
| 11 Nov 2024 | Implementation of referral pathways and models of care. |
| 7 Feb 2025 | Interim Progress evaluation report |
| 3 Mar 2025 | Continue to collect activity of team showing impact new service |
| 10 Apr 2025 | Repeat - Conduct point prevalence and patient survey |
| 21 Apr 2025 | Conduct staff satisfaction survey/ focus group |
| 5 May 2025 | Involve service users and share stories from the service user |
| 2 Jun 2025 | Final evaluation of service and wider regional dissemination |
Comments
Rachel Bamford 20 Mar 2024
This sounds like a really exciting project which could have a significant benefit to the patients outcomes. Good luck!
Arleen Watt 20 Mar 2024
Thank you Rachel, we are very excited at the potential impact it could have on our patients journey and outcomes.
Olive McGleenon 19 Mar 2024
Such an invaluable service for these patients whose outcomes can depend so dramatically on their nutritional status. Knowing that they have support between treatments when things are changing rapidly and anxiety levels are heightened will be a huge comfort for anyone going through treatment. Good luck and look forward to seeing the impact you are sure to make.
Arleen Watt 19 Mar 2024
Thank you Olive.
The implementation of the health call electronic monitoring system will all for closer monitoring between attendances to the unit and a more equitable service including for those in rural areas and with limited access to transport.
We hope to embed this element to help us with sustainable improvement that will complement and enhance the service and systems that already support our patients through their cancer journey.
Irene Thompson 18 Mar 2024
This sounds like an exciting project. We (community nutrition and dietetics) have used healthcall successfully in community, to remotely monitor clients in 2 different settings so it will be interesting to see how it will be used here. I am happy to offer support from our learning.
Arleen Watt 19 Mar 2024
Thank you Irene, it is great to have support from colleagues who have already implemented a version of this tool. I am grateful to have the experience and expertise of fellow Q-community members and colleagues. It is invaluable to have your experience of Healthcall and what you have learned from implementing this in your service.
Edel Carty 15 Mar 2024
I am delighted to hear of the plan for regular dietetic input and monitoring of this patient cohort who are at significant risk of malnutrition due to their condition and their cancer treatments.
Health call has been successful in tracking patient's weights and intakes in other patient populations and I expect some other Trusts have evidence of success of Health call within the cancer population enabling patients to tolerate cancer treatments more successfully as a result of timely dietetic intervention.
I look forward to hearing of the progress of this project
Arleen Watt 19 Mar 2024
Thank you Edel. The goal will be to use this electronic monitoring system to remotely monitor nutritional status and weight in between face to face contacts. Some patients may have a number of weeks in between cycles and attendance at the unit, being able to monitor these patients at home will reduce the burden of traveling at a time when they are often symptomatic in the weeks and days post treatment. It will also allow a more equitable service as we can offer this to those patients who are quite rural and live a significant distance from the unit and those who have limited transport means, who may not be able to travel in for intervention in between cycles.
As a result of picking up their nutritional decline / weight loss via Healthcall we can intervene much earlier rather than waiting weeks until their next attendance at the unit by which time their weight and nutrition may have significantly deteriorated. The alerts provided by Healthcall will allow us to prioritise our resources to those patients most in need and allow efficient service provision.
Jacqueline Morton 1 Mar 2024
Arleen and Hilary can you share a little more information in relation to what the patient will experience differently at the point of care by having direct access to a Specialist Dietitian and Dietetic Support Worker.
How will you know that this change will be an improvement?
Arleen Watt 19 Mar 2024
Thank you for your question Jacqueline.
There is a well-established link between malnutrition and the oncology patient group. The causes of malnutrition are multifactorial and include systemic effects of the cancer itself, treatment and side effects as well as patient demographic and lifestyle factors. As such, the prevalence of malnutrition amongst this population group varies accordingly, ranging from 11-80%
Numerous studies have demonstrated positive correlations between nutrition intervention and dietetic intervention for cancer patients and improvements in quality of life, prognosis, treatment tolerance, reduced toxicities and an overall reduced burden on the health care system.
The goals of nutrition intervention in this patient group are to prevent or reverse nutrient deficiencies, limit treatment-related symptoms, maintain weight/reverse weight loss, preserve lean body mass, protect immune function, aid in recovery and healing, and achieve the best possible quality of life and functional status of the patient.
At present the limited service we provide is reactive and capacity only allows those with significant malnutrition and nutritional issues to be prioritised. Improving referral pathways and screening and having timely access to a specialist oncology dietitian will allow for earlier intervention with the focus being on nutrition halt nutritional decline and to delay or prevent the development of malnutrition. A dedicated support worker will allow closer monitoring and addition support to relevant staff who are also supporting the nutrition of this client group – enabling a holistic and effective service.
Comments are now closed for this post.