Q Exchange
Paediatric Continence – a wee wee problem??
- Proposal
- 2023
Meet the team
Also:
- Sunni Liston, Assistant Paediatric Nurse Manager, NHS Highland, Paediatric nurse and Health Visitor (Project Lead)
What is the challenge your project is going to address and how does it connect to the theme of 'How can improvement be used to reduce delays accessing health and care services'?
Approximately 900,000 children in the UK experience continence difficulties. These difficulties are caused by a spectrum of overlapping bowel and bladder symptoms referred to as bowel and bladder dysfunction (BBD).
The negative impact on the health and wellbeing of children living with BBD is well documented. Early identification/management is essential to prevent chronic changes in the bladder and bowel which persist into adulthood.
There are causal links between these conditions and therefore they require an integrated approach for effective treatment. In Highland, children with BBD do not have access to an integrated children’s community continence service that provides individualised evidence-based care in line with national guidance. There are separate clinics for different aspects of continence care resulting in costly, inefficient use of clinical services, multiple long wait times and a lack of joined up approach to treatment. This project would involve setting up a one-stop nurse led clinic for paediatric BBD.
What does your project aim to achieve?
Currently there are separate clinics for constipation/soiling, nocturnal enuresis and daytime incontinence, plus there are a variety of healthcare professionals supporting children with delayed toilet training. Some are in primary care, some are in secondary care, and each have their own waiting lists, referral criteria, paperwork etc. A one stop clinic would aim to improve outcomes for children with BBD by…
· Ensuring all aspects of BBD are identified, assessed and treated in one clinic
· Ensuring evidence-based practice in line with national guidance
· Creating clear and effective pathways from universal services to secondary care
· Reducing multiple waiting times for access to Gp, school nurse and paediatrician clinics
· Ensuring comprehensive assessment by healthcare professionals with the necessary skills and expertise
· Creating necessary documentation to ensure the smooth running of the service e.g. referral criteria and assessment documentation.
Overarching aim is to prevent BBD continuing into adulthood through quicker identification, assessment and management.
How will the project be delivered?
The idea is to run a pilot clinic, situated in Raigmore hospital, for children with BBD. This would be run by a band 7 nurse with band 4 and admin support.
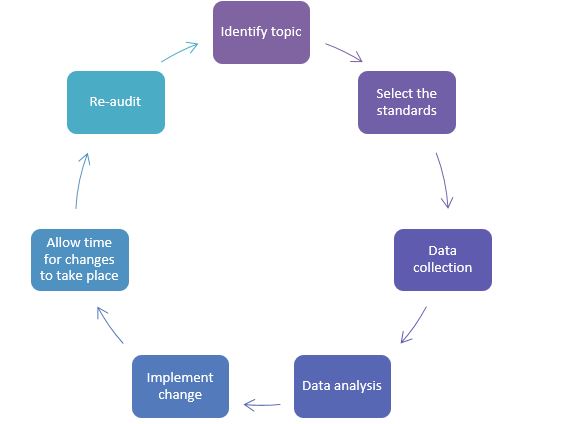
The plan would be to use the audit cycle below
1. Identify topic – improving outcomes for children with BBD
2. Select standards – Paediatric Continence Forum: Children’s continence commissioning guide, 2019
3. Data collection – current patient journey vs new patient journey. Would include numbers of children seen in the different clinics/ waiting lists and times/ number of appointments. Engagement with stakeholders – HVs, Gps, school nurses, paediatricians
4. Data analysis – method of assessing outcomes, patient feedback
5. Implement change – establishment of referral criteria and pathways, assessment documentation, management of red flags, location and admin support
6. Allow time for changes to take place
7. Re-audit – repeat data collection to see whether there is improvement in identified criteria i.e. reduced waiting times, shorter clearer journey, patient satisfaction
How is your project going to share learning?
This project will build on information and learning obtained from carrying out a scoping exercise of Children’s Continence Services in Highland, which identified the following shortfalls:
- No designated children’s continence service
- No paediatric continence nurse specialist
- Lack of clinical supervision and unchecked advice being given to children/families
The recommendations from the exercise focus on creating an integrated service. This project would trial putting that advice into practice. Only 1 in 14 Health Boards in Scotland have an integrated Paediatric Continence service which includes all 5 areas (toilet training, enuresis, daytime wetting, constipation/soiling and product provision). Therefore, this project has the potential to demonstrate good practice which could be employed in other areas to improve outcomes for children with BBD. The findings will be disseminated through the Q network and also through Paediatric Continence Scotland. Hopefully this project would also provide further evidence of the need for an integrated service in Highland.
How you can contribute
- To enable progression with the project it would be extremely useful to have help from the wider Q community in the following areas…
- QI resources to measure impact – how to compare the before and after. eg. audit cycles, data collection
- Develop my personal knowledge of how to lead on a project
- Specific questions from members around how my project will work to help me refine my idea and navigate challenges and pitfalls
- Benefit from the wealth and knowledge of others who have been through this process before
- To connect with others who are passionate about improving services within the realms of real life – budget restraints, time challenges and competing interests.
Plan timeline
| 31 May 2023 | Data collection |
|---|---|
| 31 Aug 2023 | Data analysis |
| 30 Nov 2023 | Implement change |
| 31 Dec 2023 | Evaluation |
Comments
Karen Wardrop 27 Mar 2023
This sounds a great project and an essential one. It is not acceptable that children living in some areas of Scotland are disadvantaged with poor access to healthcare. Bladder and bowel concerns impact on a child's development and wellbeing and can also affect their family and carers'. If we can assess and treat the issues promptly, the negative impacts are reduced significantly.
Look forward to hearing more, good luck.
Sarah Watt 24 Mar 2023
This project sounds fantastic. Fife has a similar clinic which has been running for several years. It has worked very well and the service continues to grow. When it started it really highlighted the number of children and young people with Bowel and Bladder Dysfunction within our area. These children had previously been seen by a number of different practitioners community paediatricians, acute paediatrics, school nurses, health visitors but now streamlined care can be provided. It has also meant in many cases reduced waiting times.
Best wishes going forward with this brilliant project.
kim mollison 23 Mar 2023
Working as a children's continence project nurse i fully agree with your aim for improving bladder & bowel services for children in your area, as this is what i am doing for my local area.
One of my aims is to develop an integrated service in Tayside to deliver clinics where assessments and treatment plans are provided for all children in a timely mannner provided by specialists with the knowledge and expertise required.
I notice in your plan it would be a band 7 nurse providing the service - could i ask if this person is a non-medical prescriber ? If not are your local GP's happy to do the prescribing for your nurse led clinic - is this from a recommendation in a letter to the GP ?
My current team does not have non-medical prescribers but i would like the nurses do complete the course in the near future.
Good luck with the project
Josephine Elliott 16 Mar 2023
Sounds fantastic - can't wait to hear more
Comments are now closed for this post.