Q Exchange
Talk To Us Together! Enhancing Parent Experience Of Neonatal Encephalopathy
- Winning idea
- 2020

What is the positive change that has emerged through new collaborations or partnerships during Covid-19 that your project is going to embed?
Covid-19 has made healthcare workers completely rethink how to communicate with patients. This is particularly true for families of the one in ten newborn infants who require some form of intensive care. With Covid-19 necessitating the need to isolate symptomatic mothers from their sick baby, the use of secure virtual contact has proved to be an extremely effective tool for communication.
In the East of England around 70 infants each year are born suffering from neonatal encephalopathy caused by lack of oxygen to the brain during birth. These babies are transferred away from their mothers to regional neonatal units for specialised cooling treatment to protect the brain (neuroprotection). Communication with families has always been challenging, particularly if it involved breaking bad news. The virtual communication revolution we have seen during Covid-19 offers a unique opportunity to bring parents to the centre of the decision making and management of their baby.
What does your project aim to achieve?
The aim is to bring parents into the heart of their baby’s management during the critical first few days of life, even if they are in separate hospitals. Parents have expressed the feeling that their baby was ‘taken away from them’, and that they ‘didn’t know what was going on’ (see video). In any event this is traumatic, but in situations where the baby may have lifelong brain injury or worse, poor communication only exacerbates an already horrendous situation. Poor communication is often sited in medico-legal cases (which from maternity cases alone costs the NHS £1 billion/year).
By embedding secure virtual communication tools, we will enable parents to have access to their baby at all times and ensure appropriate and timely communication with the doctors and nurses. Empowering parents in this way will mark a change from a ‘paternalistic’ style of medical management to a more collaborative approach.
How will the project be delivered?
This project brings together healthcare professionals working across 17 network hospitals, the Paediatric and Neonatal Decision and Retrieval service (PaNDR) and families of critically ill newborn infants. We will work closely both with family advocate groups as well as parents who have experienced birth of a critically ill baby requiring transfer for neuroprotection. This will enable us to identify the gaps in communication which this project aims to address.
With a large number of stakeholders across a wide geographical area we will appoint a project administrator to ensure effective operation and communication throughout the project.
We will develop a structured operating procedure and to mitigate risk ensure information governance sign-off from all relevant parties before commencement.
We will enrol clinical champions in each Trust to support the project, working closely with the parent partners. Rolling feedback will be instrumental in measuring and defining impact and developing resources further.
How is your project going to share learning?
UK neonatal services benefit from a regional network-based system of care. The East of England has already developed an award-winning neonatal neuroprotection service set up with funding from the Health Foundation, which will allow this project to be embedded in all 17 neonatal units. The project is scalable across networks throughout the UK through national organisations such as British Association of Perinatal Medicine (BAPM) and BLISS charity. Learning from this project can be shared with both service providers and family groups, through the QI story board, IHI websites, social media platforms, presentations and publications.
Significantly the learning from this project can be translated to other critical care situations involving the transfer of critically ill patients (e.g. trauma networks) where communication with relatives is essential if the patient is incapacitated. The landscape of virtual communication tools is complex and ever-changing and our learning will therefore be valuable to any healthcare provider.
How you can contribute
- Experience - Many Q members have experience of Virtual Communication Environments: developing secure communication tools in the NHS environment is a non-trivial endeavour to ensure appropriate security and governance. Therefore, learning from others experience and sharing our knowledge is fundamental to the success of this project e.g. initial feedback from Q has signposted us towards Mircosoft Teams.
- Sharing - We passionately believe that improving communication with families and relatives is fundamental in improving trust in professionals and developing a collaborative approach to healthcare, so will be excited to help share and support other teams wanting to use this virtual approach.
- Learning - Critical and constructive feedback from Q members will help us develop and think outside the box.
- Support - with QI methodology and implementation science will be vital and will ensure timely rollout.
- Dissemination - The Q community will enable our learning to be spread to other areas of healthcare outside our own specialty.
Plan timeline
| 1 Apr 2021 | Develop feedback form with input from parents, BLISS and charities |
|---|---|
| 1 May 2021 | Engage local units, operational delivery network and parents |
| 1 Jul 2021 | Finalise the digital platform to be used |
| 1 Jul 2021 | Information governance support will be sought from the EoE ODN/PaNDR |
| 1 Jul 2021 | SOP: communication |
| 1 Aug 2021 | Pilot phase |
| 1 Nov 2021 | 3- month interim results |
| 1 Feb 2022 | 6-month results and feedback for analysis |
| 1 Mar 2022 | Dissemination |
Project updates
4 Nov 2021
#Talk To Us Together: Enhancing Parent Experience of Neonatal Encephalopathy
Health Foundation Q Award – Mid-term reportBackground
The aim of this project was to bring parents into the heart of their baby’s management during the critical first few days of life, even if they were in separate hospitals. From the experience gained through the Covid-19 pandemic, we aimed to embed secure virtual communication tools which would enable parents to have access to their baby at all times and ensure appropriate and timely communication with the doctors and nurses. Ultimately by empowering parents in this way we hope to mark a change from the paternalistic style of medical management to a more collaborative approach.The project aimed to focus on families whose babies have suffered from hypoxic-ischaemic encephalopathy – HIE (acute brain injury resulting from a lack of blood flow and oxygen to the baby around the time of delivery). These babies are transferred to one of the three regional neonatal intensive care units (NICU) soon after birth for ongoing intensive care, including therapeutic hypothermia (cooling treatment). There is often a delay in the mother being transferred to the regional NICU and we identified at the outset that there were gaps in communication during this time.
Progress to date
We envisaged this project to be in two key phases: firstly, to look at the patient pathway, identify unmet needs and scope potential solutions. The second phase will be to pilot chosen technologies in a real-world setting.The first phase consisted of 4 key components:
· Identifying stakeholders
· Mapping out the patient pathway
· Parent engagement
· Identifying suitable platformsIdentifying Stakeholders
The applicants for the award are all Neonatal Consultants working across the East of England. At the outset we were keen to broaden the core team to include family representatives as well as stakeholders from nursing teams and the neonatal transport service (PaNDR). We were also keen to involve neonatal Speciality Registrars (StRs) from each of the 4 ‘core’ hospitals and the PaNDR service. We were fortunate to have the support from the charity PEEPS which advocates for families with a baby with HIE. Including StRs the core team expanded to 14 individuals.
Communication with such a large group can be challenging, especially when they work across the whole of the East of England. Instead of trying find a suitable time for a quorate to meet, it was agreed to have a fixed regular weekly meeting on Zoom, which individuals could join as and when available and keep everyone abreast through regular emails. The project could benefit from a Project Manager providing more structure both to the weekly meetings, but also on progress reported against predefined goals and timelines. Unfortunately creating and recruiting to a new post can be time consuming (experience from Cambridge University Hospitals NHS Trust is that it can take 6 months to get an individual into a new funded post).Mapping out the patient pathway
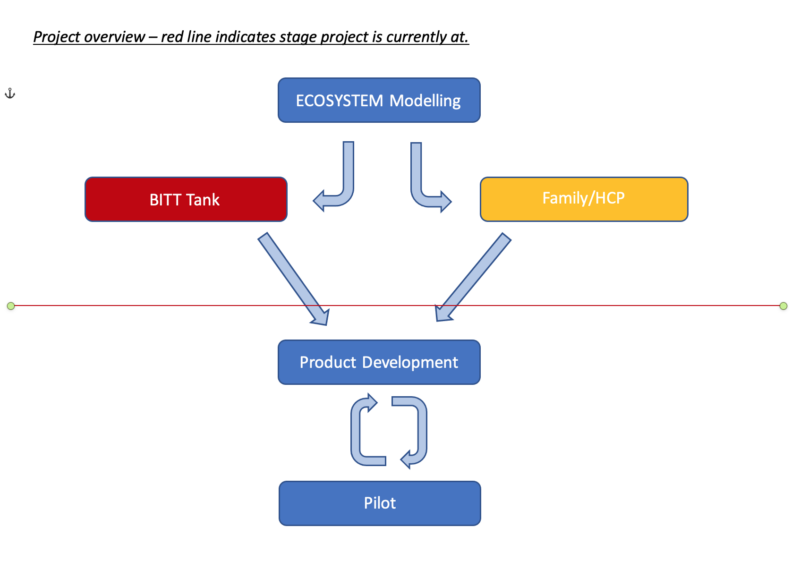
In order to help map out the patient pathway we collaborated with the NIHR Brain Injury Med-Tech Cooperative (www.brainmic.nihr.ac.uk) and the University of Cambridge Institute for Manufacturing (www.ifm.eng.cam.ac.uk). The NIHR Brain Injury MIC is designed to address unmet need in the area of brain injury where there may be technological solutions. They (and project co-application Topun Austin) have previously worked closely with the IfM in ecosystem modelling and roadmapping exercises with respect to research priorities for newborn brain injury and addressing the Department of Health’s ambition to reduce stillbirths and perinatal brain injury (www.brainmic.nihr.ac.uk/paediatrics-and-neuro-development).On 27th May we held a virtual Ecosystem Modelling workshop which was attended by 12 members of the core team (see attached report). The purpose of the workshop was to describe the ecosystem for which families with a baby with HIE finds themselves in. Ecosystem modelling uses a standard process for development and prioritization within the ecosystem and identification of candidate pathway interventions. The importance of the pathway interventions is then displayed against the ease of implementation. Of the candidate patient pathway interventions identified, the most important yet most challenging to implement was developing a transferrable IT system which gives consistent availability and functionality across areas/Trusts.
Parent engagement workstream
Having reached out to the Q community for advice on methodology, we were signposted to the Experienced based Co-Design toolkit which we used as our framework for the parent engagement workstream. We also sought advice and guidance from the NIHR Cambridge Biomedical Research Centre (NIHR C-BRC) Patient Participant Involvement & Engagement (PPIE) lead, Amanda Stranks. We reached out to parents using social medial links to our NICU’s and neonatal charities and carried out two virtual engagement events. The interview structure was based on the templates available on the EBCD framework and adapted to our patient journey. With consent the meetings were recorded, and transcripts forwarded to the rest of the team and emerging themes identified. We have also asked staff from all specialities identified as a stakeholder to complete a survey and meet for a formal interview or informal chat.Some of the themes that emerged from the parent engagement events confirmed our perception of the service in relation to delay in initial consultations with the parents and difficulties of not being able to meet the specialist teams and see their baby.
We identified other themes that are beyond the remit of communication exchange but relate to other information transfers, information availability particularly on repatriation to the local unit and upon discharge. A more detailed report on this workstream is attached.
Identifying suitable platforms
A myriad of potential IT solutions exists but we were keen to identify one which was able to address the needs of families. A key requisite was that the technology solutions needed to be NHS compliant. Through the NIHR Brain Injury MIC we held a ‘Brain Injury Technology Transfer think tank (BITT Tank)’ where representatives from SME’s and regulators met virtually to look at unmet needs and potential technological solutions within the NHS regulartory framework. Two potential IT solutions were identified: Dignio and Piota. Dignio is a leader in virtual health and is well established in community medicine and care homes (www.dignio.com); the platform is particularly designed around monitoring and assessing patients at home remotely. Piota is a communications platform used both in healthcare and education (www.piota.co.uk); with a relatively simple interface it is customisable to provide generic information as well as specific communication tools. For the size and scale of this project, Piota offered a more competitive short term cost-effective solution compared to Dignio. It also had the advantage that it could link into the existing regional neuroprotection website, www.bebop.nhs.net and could be easily modified and adapted without additional cost.Learning
Our application was written by neonatal consultants who perceived there to be a problem around communicating with families whose babies were being transferred to specialist neonatal intensive care units. Although this perception was not wrong, it was only through engagement with families, both on the core team and through the parent engagement days that we were able to truly identify needs and a focus became less on the immediate early days of their baby’s life, but more support for going home and once discharged, where many parents felt alone and overwhelmed.Our knowledge and understanding of the NHS IT regulatory framework have increased considerably and helped inform selection of potential IT solutions. However, implementation of the IT solutions across multiple hospitals in the region remains to be carried out and may be less straightforward than anticipated, as although all Trust IT systems are maintained to the same minimum regulatory standards, each Trust will have their own view as to the use of outside software and their own regulatory and approval processes.
While the project has proceeded well, largely through the efforts of the core team members, in particular Naaz Merchant, Claudia Chetcuti Gando and Florence Walston, the lack of dedicated project management time has perhaps made progress less efficient, and this will be a concern moving forward into the pilot and implementation phase. One particular challenge of an award of this nature and duration is the bureaucratic inertia to get things set up at speed, and this is particular true of recruitment to posts, which is why we decided against this. There were already lengthy delays in getting the contracts approved and signed off by one of the host institutions and this can slow the whole project down. We were fortunate that both the Ecosystem modelling project and BITT Tank was paid up front by the NIHR Brain Injury MIC and the parent engagement workstream was cost-neutral.
The final challenge to date has been getting engagement from other healthcare professionals. This is made harder by the project covering 17 hospitals over a large geographical area. A major challenge in neonatal intensive care units across the unit is one of staffing pressures resulting from a combination of Brexit and the pandemic and those that remain are physically and mentally exhausted. That means, however interested they may be in the project in theory getting their engagement can be challenging.
Next Steps
The next steps will be to purchase the Piota App and develop content for the App and the complimentary BeBoP website, much of which should be reflected by the information obtained through the Parent Engagement exercises. This will be generic information related to perinatal brain injury and links to support sites as well as unit specific information. We aim to link the App to a video-calling platform such as Zoom or Microsoft Teams. There may also be the facility of providing messaging information via the App.We will need to identify the best way of generating content for the App and website. It may be preferable to sub-contract this work, rather than rely on ‘good will’ of team members, given their time pressures.
Once this is done the challenge will be to pilot the platform across 2 or more hospitals. Given that HIE is a relatively uncommon event (~1/1000 births) pilot data may be limited. An alternative strategy will be to pilot across several sites, but there may be challenges of varying IT regulations across different Trusts.
Sustainability: while we have the funds to continue the Piota App in the short-medium term (2-5 years), our previous experience with the BeBoP website was without a champion driving the site it quickly falls into disrepair. The pilot phase may demonstrate proof of principle that the technology works and can be adapted based on feedback but embedding the platform into part of the care package of these infants across the region will be a huge challenge.
Involvement of the Q community
We would welcome any feedback and advice from the community on any aspects of the project outlined in this report.Specifically, we would welcome:
· Advice around navigating IT regulations across different Trusts.
· Engaging healthcare workers in the project.
· Project management tools for non-project managers
Comments
Claudia Chetcuti Ganado 6 May 2021
Dear Team, As one of the team members in this project I would like to invite ideas/help around creating a parent engagement interview or focus group to explore parental expectations in their journey and how our current system failed to meet their expectations. Additionally we hope to learn from positive practice gathered from the differing experience so we can embed positive practice in our processes of care through this project.
Andrea McGuinness 12 Oct 2020
HI, this feels like a very relevant project and is already suggesting lots of transferable learning opportunities both into and out of your project. If you need any help with using QI to define and test your ideas I am happy to help.
Nazakat Merchant 19 Oct 2020
definitely would be interested to touch base re testing our ideas using QI methodology
Jo Scott 7 Oct 2020
Hi Nazakat - you may find it helpful to reach out to members of the SiG about video consultations, as they may have expertise to share about the different platforms available, and pros and cons. Many of the people in that group would have been involved in implementing video consultations rapidly in response to COVID-19 so may also have useful learning about security and governance, and the specific QI approaches that were useful for them https://q.health.org.uk/community/groups/video-consultations-how-to-set-them-up-well-fast/
Nazakat Merchant 19 Oct 2020
Thank you
I have become a member of the group and hoping to get some good ideas to use in our PDSA cycles
Peter Dudgeon 30 Sep 2020
Hi Nazakat,
Myself and my colleague Emma Adams (Health Transformation Partnership) are supporting the Health Foundation this year by fostering conversations between Q members and encouraging collaboration. We were Exchange applicants last year, so we’re hoping that our experience will help us to help others, as their ideas take shape.
Having read through your idea (which I found very compelling, by the way. The litigation costs quoted alone are eye-watering!), I was struck that there are a number of project ideas seeking to deliver a high quality digital services, post-COVID. They address different services, but have some similar challenges e.g. the choice of the best virtual platform. I have picked out a few projects which I think it would be beneficial to link with (perhaps comment on their idea pages?): "Embedding video consultation services inclusive of non-English-speaking communities", "Using Telehealth to support patients on chemotherapy at home" and "Supporting frail patients with diabetes in a virtual clinic age". If I can help you make further connections I will and in the meantime I wish the best of luck with your idea.
Pete
Nazakat Merchant 19 Oct 2020
Hi Pete
Sorry for the late reply (busy clinically- its the season!)
Yes please any help would be great.
Thanks
naaz
Comments are now closed for this post.