Q Exchange
Outpatient Transformation across Norfolk and Waveney STP
- Proposal
- 2019
Meet the team
Also:
- Linda Hunter (Planned Care board lead)
- Jon Green (Exec SRO - NNUH)
- Jo Segasby (Exec SRO - JPUH)
- Sarah Jones (Exec SRO - QEH)
- + c35 other individuals
What is the challenge your project is going to address and how does it connect to your chosen theme?
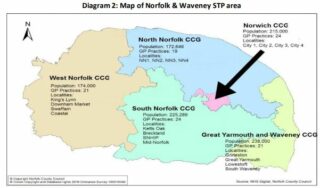
The Norfolk and Norwich University Hospital ( NNUH) is part of the In Good Health – The Norfolk and Waveney Health and Care Partnership . Our partnership is a big and complex system includes local GP practices, 3 Acute hospitals, community care, social services and mental health teams, and together we provide services to more than a million people
We are in the process of agreeing a vision / mission / objectives across the county to make the whole system join up in delivering improvements. Initial discussions between CCG partners and the 3 acute hospitals have identified that all 3 acute trusts have recently kicked off Outpatient transformation programmes with this being an opportunity to link all 3 programmes.
The digital maturity of the three acute trusts is poor (worst, 3rd worst and 5th worst in the country) and with an IT digital strategy linking across. the STP, this is an opportunity to improve together while achieving the NHS Long term plan of 30% virtual appointments by 2024.
What does your project aim to achieve?
All the ideas below have come from staff / patients in Outpatients when asked the question – “What would you change in outpatients” – list by no means exhaustive and will continue to evolve throughout the programme
- Virtual clinics
- Group Clinics
- Virtual group clinics
- Improved triage for referrals
- Better use of digital apps (for patient management of own diagnosis)
- Patient portals (for appointments / letters)
- More cohesive GP Advice and guidance (with pictures / video)
- Co-ordinating evening clinics to be same night
- More one-stop clinics
- Reduction in unnecessary appointments
- Digital dictation / voice recognition
- Electronic prescribing in OP areas
All with a view to
- Reduce inefficiencies (Cost)
- Enhance patient experience
- Patient control of own illness
- Better clinic utilisation
- improved RTT performance
- improved FUN ratio
- Improved DNA rates
How will the project be delivered?
The STP will be aware of the whole programme through the planned care board.
The 3x Acute Trusts each has an appointed Exec SRO and project team who will be be responsible for the individual progress of installing trustwide / STP wide technology tools.
Individual Specialties / Practices will be encouraged to link with other trusts and patients to determine and co-design each of their own 5 year action plans – the center to help provide the tools to deliver.
To mitigate the risk of any change we will identify where trials/pilots (by specialty) for appropriate technology / system wide change will be most effective and where the specialty has a particular interest (i.e. paediatric diabetes and virtual clinics).
During any pilots/trial we will continually monitor progress through the PDSA cycle, assuming a positive effect is being seen in measures (including balancing metrics) – we will then consider rolling out trust wide, then system wide.
What and how is your project going to share learning throughout?
First step is to agree the strategy and general principles across the STP – assuming agreement.
Programme Management
- Monthly updates through scheduled webinar meetings with Executive SRO’s + leads from each organisation
- Fortnightly updates hosted by each organisation to share the learning from above and agree updates to feed up to STP wide board
Specialty Action Planning
- Facilitated face-to-face action planning in a “live” outpatient environment to create the 5 year plan
- Continual support from individual organisations – linking organisations where appropriate
Communication
- Produce a quarterly system wide ‘Sharing the Learning ‘ e -bulletin to provide updates and share progress.
- Implement a local online forum to allow staff to share ideas for transformation, collaborate and communicate regardless of care setting and location.
- Utilise and promote social media to promote cross sector working, collaborative ‘peer support’ and virtual networking
- Use the Q community for commenting on local ideas
How you can contribute
- The promoter: help to get this idea noticed
- Collaborator: When we update the Q community with ideas, if you have a similar idea how can we look to collaborate now or in the future
- Networker: help us to link up with similar ideas
- Critical friend: how can we make this idea better challenge please have we missed anything?
Plan timeline
| 30 Jul 2019 | Agree broad vision / mission / objectives across the STP |
|---|---|
| 30 Sep 2019 | Formally launch the programme |
| 31 Oct 2019 | Consolidate first draft specialty plans |
| 31 Oct 2019 | Implement first changes in pilot areas |
| 31 Mar 2023 | NHS L/T aims achieved - i.e 30% Virtual Clinics |
Comments
Sarah Campbell 16 Jul 2019
Vital that initiatives are joined up! Would be good to explore how you might measure your success criteria/outcomes - is there good data available on these areas?
Comments are now closed for this post.