The general hospital where I supported a debrief has six wards with a mixture of speciality doctor, foundation trainee doctors and nurse practitioners/advance nurse practitioners who provide medical cover on a 24/7 basis.
On one afternoon, two of the speciality doctors were on Supported Programmed Activity (SPA) time, often used for professional development activity.
A patient arrived on a ward where one of the SPA doctors was usually based. There were delays to clerking in the patient and differing views on who was responsible for providing clinical care in the absence of the doctors on SPA.
A number of nurse managers, support colleagues and medical consultants were involved in trying to resolve the situation. The request bounced back and forth between medical and nursing staff and clinical managers.
This situation initially came to light to the management team following email communication between medical and nursing leaders.
Following this event, there was confusion over whether or not there could have been a patient safety issue. In addition, I saw potential for conflict in the team but also a great opportunity for learning.
What action was taken?
A decision was made to undertake a form of structured debrief to achieve shared understanding and ensure learning.
However, what I feel is worthy of note, and what triggered me to write this blog, was my decision to apply some of the learning I acquired over my time in the GenerationQ fellowship sponsored by the Health Foundation between 2018-2021. It was through this fellowship that I came to better understand, experiment with and build even further into my practice what I now know as relational leadership.
So, what was the extra element that I layered onto this structured debrief process?
It was, to quote a Fun Boy 3 featuring Bananarama classic, ‘it ain’t what you do, it’s the way that you do it.’
Applying relational leadership to a learning setting
The relational leadership principles from GenerationQ are:
- careful consideration of the layout and environment for the debrief (creating the conditions for dialogue)
- the nature of the invitation (start in a learning, “one team” mindset, naming the discomfort likely to be experienced whilst describing the space where learning occurs)
- the style of facilitation – curious, non-judgemental, holding the space for discomfort, keeping it simple – use of session outline (so participants know what to expect)
I used a meeting room which was cleared of the usual rectangle table and set up instead with a chair for each participant arranged in a circle (no barriers, no hierarchy).
I provided tea, coffee and cake (nourished – observing Maslow’s hierarchy of needs)
I prepared an outline of the session structure in advance and made sure that it was visible to everyone in large font on a dry wipe board in the debrief room.
Facilitating a learning-based dialogue with colleagues at all levels
My email invitation was carefully structured as an invitation to a meeting aimed at ensuring learning:
Subject: Hot debrief, with cake!
Dear all,
Following some feedback from a couple of you I would like to convene a ‘hot’ debrief tomorrow for an hour regarding the staffing deployment issues on site from yesterday; at 1415 in the meeting room.
This is an excellent opportunity to continue to build strong, trusting relationships between us that enables the challenging stuff to be discussed and progressed collaboratively.
There is a standard outline for such sessions that I intend to use; what happened, why and how it felt for each colleague. I will facilitate this in a ‘removed from the operational detail’ role. There will be tea and coffee, and a fine piece*!
We are a fantastic committed team; and strong teams grow even more with the courage to lean into learning from difficult moments.
I look forward to doing this, together, tomorrow.
Regards
*local vernacular for cake
I invited all those colleagues directly affected – a nurse manager, service manager, deputy service manager, and medical lead.
I also invited one medical consultant colleague who was not involved. I invited this individual in order to balance a potential power dynamic differential between medical and “management team”; and also because I believed that the experience and demeanour of this person would be beneficial to the debrief dynamic.
I ensured all present had a drink and were comfortably seated before signalling the session commencing by outlining the steps I intended to use.
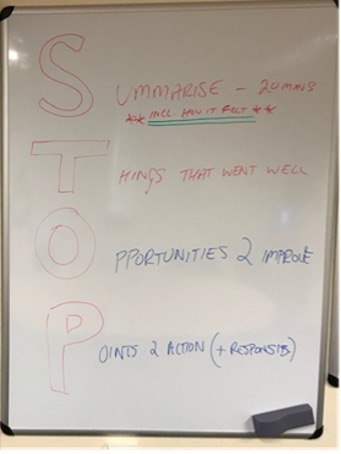
I used a format I was trained in many years ago known as STOP:
I invited each participant (other than the independent consultant) to describe the timeline of events as they experienced it with a factual account whilst also focussing on how it felt. I asked that each participant have the chance to tell their experience of the events uninterrupted.
Following all members having the time to speak, I asked for any observations or thoughts.
The medical lead highlighted that they now had a much more rounded picture of what had happened but also, crucially in my view, how it felt to some of the colleagues.
This led to the voicing of an apology from a colleague who said:
‘I am sorry I made you feel the way you have described; I now have a much rounder understanding of what happened than I did on the day.’
The medical lead also offered their personal learning that it may be helpful to seek other views or perspectives in future challenging situations.
Having shared each individual’s understanding of what occurred and how it made all colleagues feel, we moved to asking for views from those present on the other prompts; things that went well, opportunities to improve and, finally, points for action.
I intentionally adopted a curious perspective, choosing open questions to allow those present to share their views on the contributory factors to the course of events and how colleagues felt.
Learning opportunities
This discussion generated a list of learning opportunities, which we translated into action learning points:
- Unclear or uncomplied with standards for maximum numbers on planned SPA
- Unclear expectations from staff on SPA time as to clinical responsibilities (“rules”)
- Clarify expectations for Direct Clinical Care sessions
- Unclear minimum specification for staffing per clinical area
- Inadequate cluster workforce planning leadership (using clear minimum specifics)
- Lack of triumvirate gathering to ensure a consistent leadership team approach (nursing, medical, general management)
- Lack of respect from Specialist Doctor team to Medical Lead, Deputy Service Manager, Nurse Practitioner colleagues
- Output from SPA protected time
We finished by agreeing who would lead on the actions we identified. We agreed to meet a couple of weeks later to review progress against agreed actions and to get any feedback on the process.
At our follow-up meeting, a number of the actions had already been completed – which could be evidence of the level of buy-in resulting from the process and the manner of delivery.
In addition, three of those present commented on the helpfulness of the format used. When I voiced my interest in writing this up as a blog, colleagues were supportive with one responding, ‘sounds like a good plan to share the learning from this useful exercise.’
On a personal level, this felt like good, useful, courageous work with learning for those present not just related to the event itself but in relation to ‘how we do things round here’ – in other words the culture of the team.
Leaning in to discomfort as part of learning
My main learning from this approach and style of implementing is that although a structure or methodology is important a number of other factors are equally, if not more important.
A relational leadership approach includes intentionally considering the way the space is set up, the nature of the invitation and the style of host leadership. Each of these factors should contribute to facilitating an openness to learn alongside a desire and willingness to lean into discomfort.
These were all key ingredients in this process for delivering the learning derived but also in being a part of the story of the leadership team.
So, next time you are engaging with a group or colleagues in a difficult discussion, it is hugely worthwhile to consider what the song says: ‘it ain’t what you do, it’s the way that you do it!’
Jason Nicol has recently moved from a senior operational management role into a Strategic Change Lead role within NHS Grampian/Aberdeen City Health and Social Care Partnership.