I have written previously about the “Family Voices” Big Room where we brought people from primary care, secondary care, the council, integrated care board, academic health science network, third sector, and the local community together to talk about the health journey of new parents.
I learnt so much from using the Flow Coaching Academy’s principles of combining improvement methods and coaching in this context, but the most valuable learning came from the mothers themselves.
“Why would I come to a meeting when I don’t know anybody there?” said one of the Maternity Champions. Her words stuck with me – how true! Local community members would enter our room in little groups – a table of Sudanese women, another of Moroccan friends… we got to know their family backgrounds, hopes and wishes over our cumulative time together.
In person, in partnership, in place
These last Thursday of the month in-person sessions were where “the magic happens” as Maternity Champions Programme Manager Sona put it. Handshakes, hugs and sharing lunch in a place designed for community conversations brought people together in greater numbers than the weekly Zoom meetings in-between.
Partnering with local third sector organisation Maternity Champions meant we were working in a setting where trust was already established. Families felt comfortable at The Venture Community Centre on their estate – it was close to home and they already attended parenting classes, cooking classes and play sessions there. We scheduled the sessions to run immediately after a baby group and to include lunch, so it was natural to invite mothers to stay for lunch and join the discussion.
Handshakes, hugs and sharing lunch in a place designed for community conversations brought people together.
While we discussed rotating the venues, we decided against it, recognising the benefit of investing time to build these local place-based relationships.
The remote sessions were still valuable in between. They were easier for our office-based partners and useful for reviewing data, Plan Do Study Act (PDSA) cycles, and planning how best to use the monthly meetings.
Paying attention to who is and who isn’t in the room
The sessions brought together local mothers, volunteers, health sector professionals from primary and secondary care, council representatives and academics.
Involving local community health workers, who operate on a model of monthly home visits, enabled us to magnify representation from the local community. They get to know their family caseload by understanding their holistic needs and thus are able to represent a large number of diverse families, including those who were not present at the meetings.
Co-production tells a different story
A week after war broke out in Sudan, we went into the session and – as usual – began with an icebreaker. Part of the reasoning for this is that if a voice is heard early on in a meeting, it’s more likely to be heard again later. We asked people, lightly, where in the world they might like to visit. One of the participants answered that they would like to go to Sudan, but sadly that wasn’t possible now. It was a moment of recognition, shared sadness and mutual respect.
We realised that mistrust of hospitals amongst certain minority groups was linked to inter-generational trauma and poor experience dealing with formal institutions.
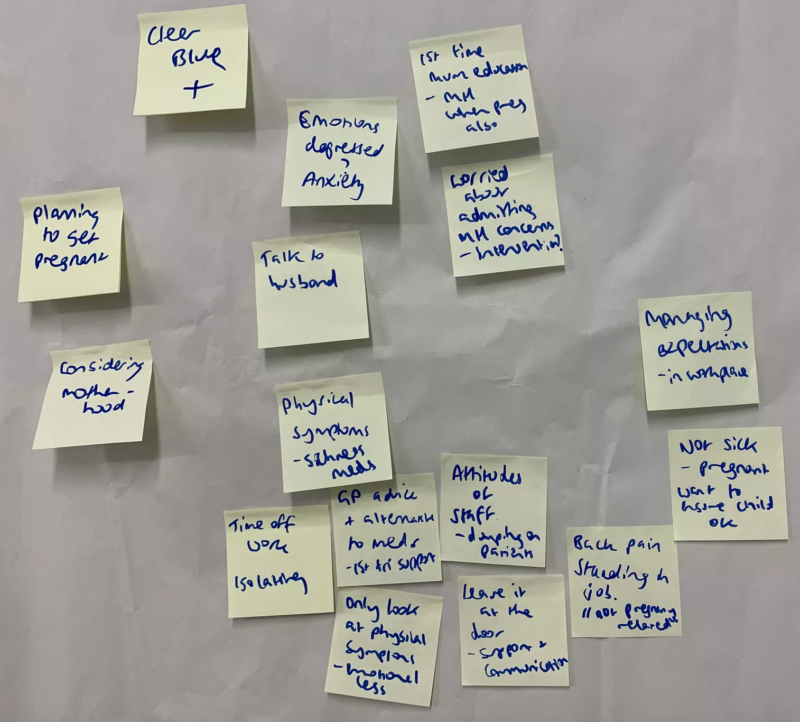
One of the most powerful and memorable Big Rooms we had was early in our journey, where we mapped the pregnancy pathway. We created an emotional map rather than a conventional process map, and identified where the critical points were for the pregnant person and the wider family. We realised that mistrust of hospitals amongst certain minority groups was linked to inter-generational trauma and poor experience dealing with formal institutions such as the police, education, housing, etc.
This emotional map led us down the route of working on the mental health needs of our new parents. We also facilitated a Big Room conversation on the cultural experiences of receiving health care to enable listening, learning, and trust-building.
Networks for collective power and knowledge
Here are some things we accomplished via the power of our collective networks:
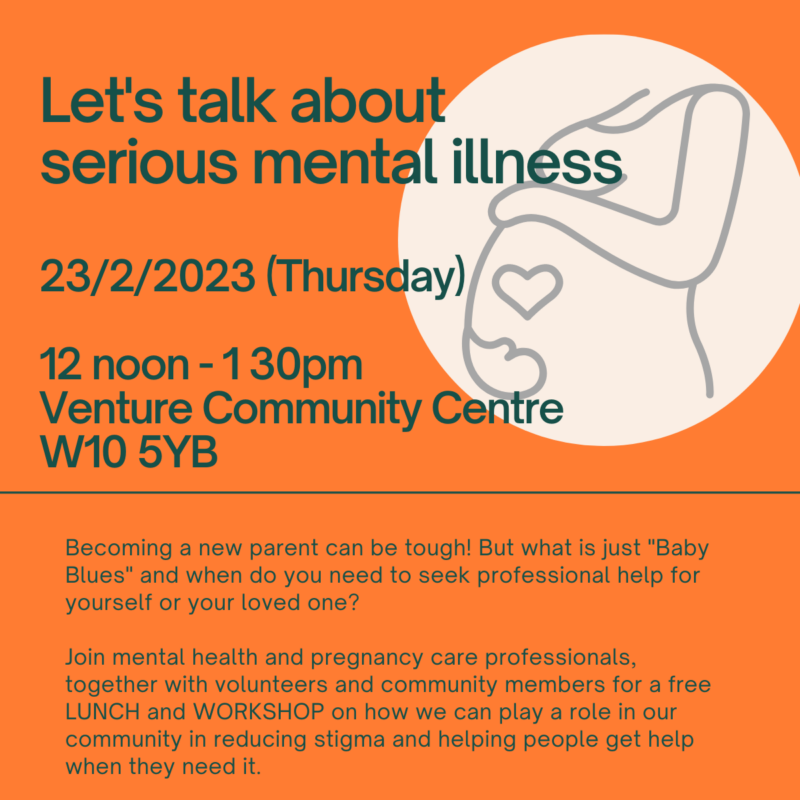
- Consultant Psychiatrist Jamila ran a Serious Mental Health workshop, which brought together 40 attendees learning about how to identify and refer new mums with serious mental illness.
- We compiled a repository of local support – addressing financial, mental and physical health – for new families. We have gotten this information into the northwest London Mum & Baby app owned by the ICB.
- We connected Anya, the award-winning parenting app with the northwest London ICB, following a local trial via our Maternity Champions.
- We increased the number of breast-feeding support volunteers working on postnatal wards through inspiring and encouraging Maternity Champions, and by connecting them with Imperial Health Charity.
- Attendees have reported using facilitation skills, story-telling and inspiration from the Big Room to further their own personal development and careers.
Recipe for health
Improving health in a diverse community is complex. The ingredients are understanding diverse needs, safe spaces and trust. The method is co-production through skilled facilitation, coaching, utilisation of networks, and bringing together existing structures. Working in this way does need dedicated time, coordination and leadership.
Engagement is a journey of constant relationship-building and networking.
We used the tried and tested Impromptu Networking on our last Big Room on 27th April 2023 to ask:
· What are the ingredients for successful community engagement?
· What have we accomplished?
· How do we work together to make our families healthier?
I was sad that many of our Big Room regulars asked me, “Is this really our last session? Or is it just a pause?” The fact was that the pace of a weekly meeting was really effective at maintaining engagement and interest but required constant oversight and steer from the Big Room coaches.
Working in this way does need dedicated time, coordination and leadership.
I plotted the attendance data for our weekly meetings onto an SPC chart:
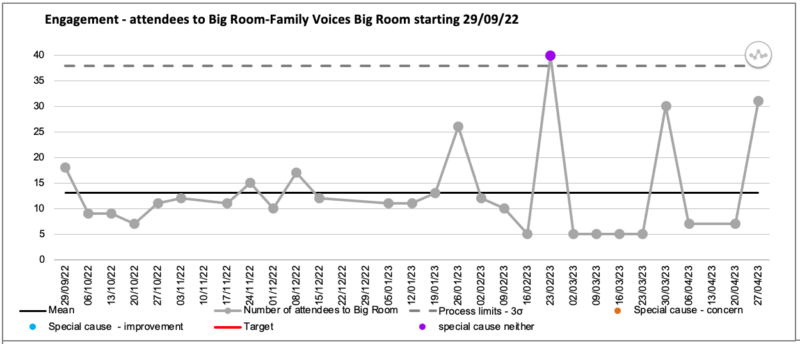
The SPC chart showed that in the month of March, when I was on holiday and my weekly email invite detailing the agenda and actions was not being sent, our Zoom attendee numbers went down. The chart also clearly shows that the in-person sessions at Venture were really popular, with spikes occurring the last Thursday of each month.
With my co-coach Hannah going on maternity leave and me starting a new job at NHS England, the Big Room – though beloved – was going to have to go. But there’s no reason why it couldn’t start up again.
Access co-production tools and tips and join the conversation in our Co-production Special Interest Group.
Resources
National Co-production Week 2023

Comments
Nicola Platts 21 Aug 2023
Sabrina this a fantastic article showing the benefit of coached weekly meetings for patients and staff alike. It also rises the challenge about how to sustain when the coaches have to move on. I do hope it will be a pause and not a stop. Congratulations to the Big Room this is a great case study about what makes good co-production and even has an SPC chart.