Q Exchange
Promoting safer prescribing: sustaining, scaling and spreading SMAC2
- Idea
- 2018
Meet the team: The SMAC2 cooperative (#smac24saferprescribing)
Also:
- Tim Dornan, Professor of Medical Education, Queen's University Belfast
- Ms Angela Carragher, Associate Postgraduate Dean, Northern Ireland Medical and Dental Training Agency
- Deborah Millar, Clerical Officer, Centre for Medical Education, Queen's University Belfast
The General Medical Council commissioned EQUIP Study (Dornan et al, 2009) which examined the prevalence and causes of junior doctor prescribing errors, identified that 70% prescribing is made by junior doctors and 30% of prescribing contains errors. However a lack of prescribing knowledge is rarely the reason why prescribing errors occur. This has also recently been echoed by the Royal College of Physician’s guide ‘Supporting junior doctors in safe prescribing’, which cites a lack of knowledge / experience as 1 of 22 reasons why prescribing errors occur. Other reasons are due to the systems, the environment, the task, the team and the individual themselves e.g. their resilience.
Our aim builds on an earlier idea, which we have successfully developed, implemented, and disseminated in the context of
Northern Irish insulin prescribing. It is attracting national attention. But it has much untapped potential. Our present idea is to achieve even greater health benefit by sustain, scaling and spreading SMAC2:
-
More widely in the diabetes community
-
To other high-risk medications.
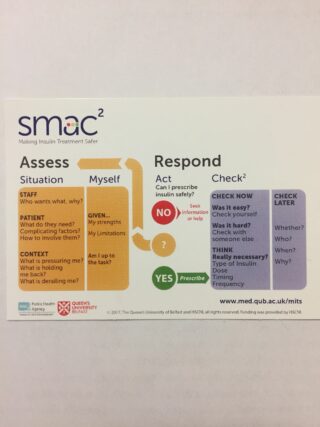
The acronym SMAC2 (pronounced ‘smack squared’) guides professionals through five stages of situation and self awareness:
-
(What is there about this) Situation (that could lead to harm)?
-
(What is there about) Myself (that could make me behave unsafely)?
-
(How should I) Act (to ensure a safe outcome)?
-
(Have I) Checked (the safety of my action)?
-
(Who needs to) Check later (to ensure the action is working as intended).
Foundation doctors (FDs) carry a SMAC2 lanyard card, which spells out those messages in a little more detail and the reverse side provides ‘hot tips’ to prescribing insulin (or, potentially, carrying out any other safety-critical task) more safely. We have trained pharmacists, nurses, doctors and patients with type 1 diabetes in empowerment and facilitation techniques, to carry out 15-30 minute case based discussion debriefs that help FDs reflect on specific prescribing experiences and make SMART commitments to safer future behaviour. This is centred on the SMAC2 tool and gives them non-technical skills to behave safely in situations that provoke uncertainty. The debriefers also don’t need to be specialists in diabetes management, they just need to be able to conduct reflective learning and support the doctor identify their training needs using the SMAC2 tool.
Most important of all, SMAC2 addresses patients’ involvement in their own care head-on. It does this in two ways. One
is that SMAC2 teaches FDs to involve patients in decisions about their own. The second is that patients with type I diabetes use their expertise in insulin safety to conduct SMAC2 debriefs, which contribute to FDs’ progress assessments. Service users are actively involved in improving patient safety.
This simple initiative make a sea-change to patient safety education. It shifts the focus from isolated, individual prescribers, to
prescribers collaborating in interdisciplinary practice, in which patients themselves are active members. It personalises workplace learning to the individual professionals, and their relationships with individual patients. Rather
than ‘teaching the right answer’ which often does not exist, it encourages prescribers to identify whatever uncertainty exists in a given situation and respond to it by drawing on all available resources. We have evidence, for example, that junior doctors are reluctant to call senior help but SMAC2 helps them do this.
The beauty of the original idea is that SMAC2 is applicable to any high-risk medication. Indeed, any medication. Indeed any complex act undertaken by a health professional. Because it is flexible and widely transferable, its benefits will amplify as it scales and spreads. At present, however, the idea is in between the proof-of-concept stage, for which we obtained external funding, and it becoming sustainable within user communities. There is every reason why it could and should become embedded. Because SMAC2 is a reflective tool, supported by simple operating procedures, it can be implemented within existing systems and structures at minimal additional cost.
We have such strong ‘proof of concept’ that we have been award a Royal College of Physicians Education and Training Award and we are shortlisted for a HSJ patient safety award. Given that, for example, the excess cost of treating diabetic (compared with nondiabetic) patients in UK hospitals approaches £1 billion, even small impacts on insulin safety could pay huge dividends. These will result from reducing the cost of error and litigation and making better use of existing system education. This will also reduce the anxiety caused to patients and professionals by error.
The beauty of the original idea is that SMAC2 is
applicable to any high-risk medication. Indeed, any medication. Indeed any complex
act undertaken by a health professional. Because it is flexible and widely transferable,
its benefits will amplify as it scales and spreads. At present, however, the
idea is in between the proof-of-concept stage, for which we obtained external
funding, and it becoming sustainable within user communities. There is every
reason why it could and should become embedded. Because SMAC2 is a
reflective tool, supported by simple operating procedures, it can be
implemented within existing systems and structures at minimal additional cost.
We have such strong ‘proof of concept’ that we have
been short-listed for two national patient safety awards. Given that, for
example, the excess cost of treating diabetic (compared with nondiabetic)
patients in UK hospitals approaches £1 billion, even small impacts on insulin
safety could pay huge dividends. These will result from reducing the cost of
error and litigation and making better use of existing system education. This
will also reduce the anxiety caused to patients and professionals by error.
How you can contribute
- • From within the diabetes community, to embed SMAC2 into interprofessional diabetes practice
- • From patient safety champions, to advocate for this novel approach to health professions education
- • From interprofessional team members and service users to spread SMAC2 to other safety-critical healthcare tasks
- • Building and sustaining communities requires administrative support. We request funding to establish and support the excellent communication that will achieve the desired results
Further information
MITS SOP (PDF, 5MB)