Q Exchange
Improving pathways across an Acute Provider Collaborative
- Proposal
- 2024

Meet the team
Also:
- Ben Irvine, Programme Director Acute Hospital Alliance
- Christine Nagel, Programme Manager, Acute Hospital Alliance
- Rhiannon Hills, Director of Transformation Royal Untied Hospitals NHS Foundation Trust
- Alex Talbott, Associate Director of Improvement, Salisbury NHS Foundation Trust
What is the challenge your project is going to address and how does it connect to the theme of 'How can we improve across system boundaries?
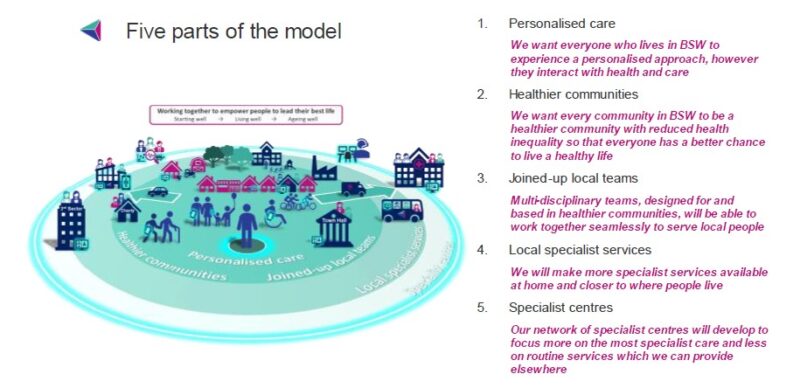
Our Acute hospital provider collaborative works across the 3 acute hospitals. These hospitals are vertically integrated an also provide community services. We are working together to increase the sustainability of a number of clinical pathways across our Footprint as part of our AHA clinical strategy within the context of our ICB model of care. We are working across organisations and with wider partners to: improve care, focus on what matters to patients and deliver care closer to home where possible.
The pathways that are the focus of the work include Orthopaedics, Gastroenterology, Urology and Dermatology. These specialties all have challenges with sustainability either because of increasing demand or capacity constraints. Therefore transformation is needed to think differently and create sustainable solutions that met current and future patient needs.
What does your project aim to achieve?
The project puts the clinical teams at the heart of delivering improvements and sustainability. We are aiming to deliver
- Working together to provide excellent care with equity of access and services across the 3 acute providers within our provider collaborative
- Services with increased sustainability with a workforce that can be developed and maintained to meet the future needs of our population
- Putting patient needs at the heart of our pathways with a focus on reducing health inequalities through the use of population health intelligence. Building co-production into our improvement so that the voice of patients and frontline staff is strong.
- Implementing a “left-shift” in care towards primary and secondary prevention and increasing collaboration between secondary, community and primary care to deliver more joined
We will use the Q exchange funds to increase clinical leadership and improvement practitioner time to increase the pace of the improvement work.
How will the project be delivered?
The three organisations have a common approach to Improvement called Improving Together which is a lean based operational management system. Improving Together resources are being used to support the priority pathways, however, resources are limited, currently there is some clinical leadership, Organisational Development, improvement expertise and analytical support to the priority pathways but we are looking to bolster these using Q exchange funds to pump prime progress.
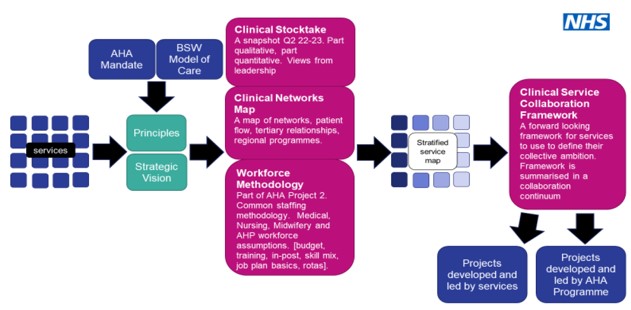
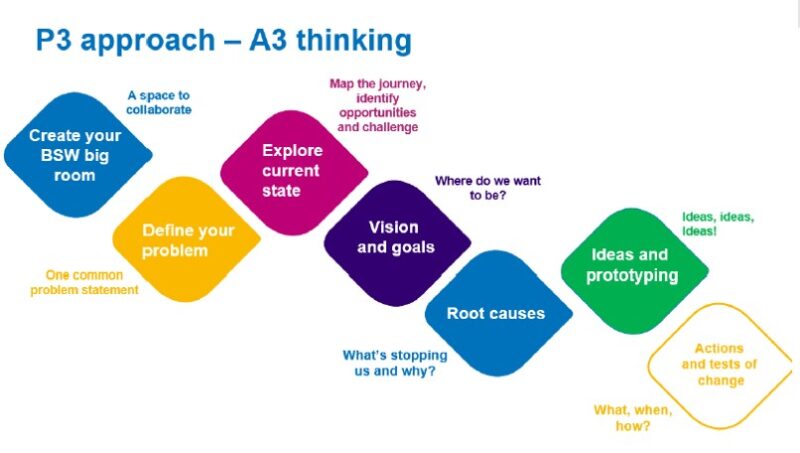
We are using a Clinical Service Collaboration Framework to support improvement in the priority pathways. The framework has three parts: current state, future state self-assessment, roadmap for delivery and implementation. We use an A3 thinking approach which involves “big room” rapid improvement events to involve stakeholders including patients, carers and members of the public. We are keen to increase the focus on co-production and health inequalities within this way of working. Each clinical pathway has a milestone plan (example below)
How is your project going to share learning?
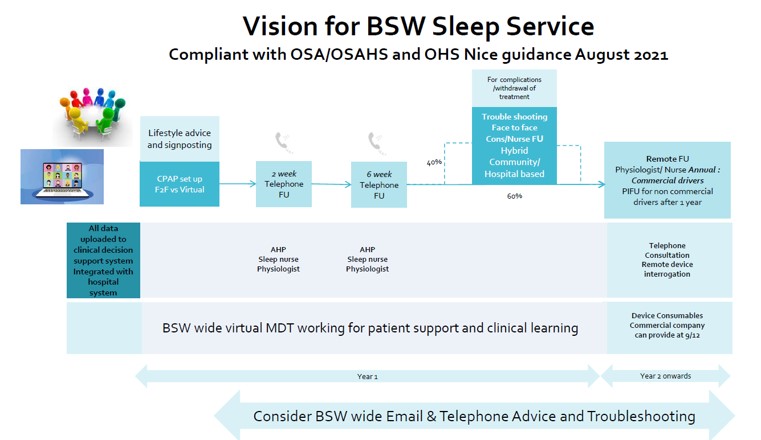
We have regular clinical summits which support clinical teams to share learning. This has been successfully used in a number of specialties including sleep services, oral surgery and pharmacy. Learning from previous clinical pathways has helped inform the current project plan. We also use our Improving Together networks to share learning.
Additional support would allow us to share learning beyond our provider collaborative, we envisage that shared learning would be valuable around February 2025. The pictures below are from previous learning events and we would be keen to use external networks such as the Improvement Directors Network/National Improvers Learning Network to share learning further.
How you can contribute
- Do you have experience of left shift of care in the specialties we will be focusing on: Dermatology, Orthopaedics, Urology and Gastroenterology?
- Do you have experience to share of workforce redesign in the specialties we will be focusing on?
- Can you share learning from consolidating waiting lists across a provider collaborative (orthopaedics)?
- What has worked well in terms of co-production approaches within pathway improvement?
Plan timeline
| 30 Apr 2024 | Recruit additional support |
|---|---|
| 31 Jul 2024 | Orthopaedics implementation |
| 30 Sep 2024 | Gastroenterology implementation |
| 30 Sep 2024 | Urology implementation |
| 14 Jan 2025 | Dermatology implementation |
| 28 Feb 2025 | Agree next steps |
| 28 Feb 2025 | Summary of learning at clinical summit |