Q Exchange
Triage MDT ‘Paeds Together’ (CYP hubs) – working smarter, not harder
- Shortlisted idea
- 2023
Meet the team
Also:
- Dr Attah Ocholi (Clinical Director Paediatric department of St. Georges Hospital in equal partnership with Dr Tom Coffey, GP lead of paediatric integrated care Wandsworth
What is the challenge your project is going to address and how does it connect to the theme of 'How can improvement be used to reduce delays accessing health and care services'?
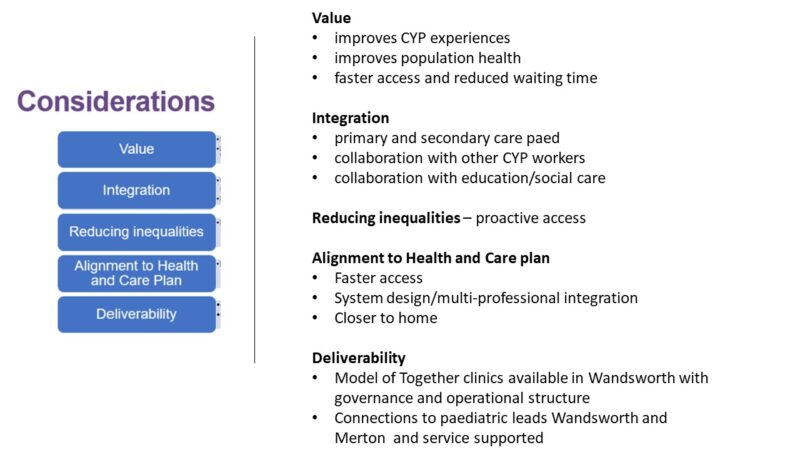 Instead of referring CYP (Children, Young People) to hospital clinics, these joint Triage meetings facilitate the review of referrals and allow direct advice for paediatric management input. This leads to faster clinical input getting patients to the right place, right time and right team, ensuring pathways are built around patients and not around organisations, reducing waiting for time/referrals to hospitals and enabling clinical assessment without delay.
Instead of referring CYP (Children, Young People) to hospital clinics, these joint Triage meetings facilitate the review of referrals and allow direct advice for paediatric management input. This leads to faster clinical input getting patients to the right place, right time and right team, ensuring pathways are built around patients and not around organisations, reducing waiting for time/referrals to hospitals and enabling clinical assessment without delay.
The service is agile, brave, transparent, using Quality improvement tools/data to address issues continuously in partnership with primary care.
It utilises existing ‘Together clinics’ relationship and operational processes by inviting additional professionals, e.g. nurses, pharmacists, health visitors etc.), connecting primary care with secondary care paeds and through secondary paediatrics, building links to tertiary specialists. As a result, the multi-professional teams can ensure faster and safer access to services.
In addition, it provides interprofessional learning leading to high standards in clinical management.
What does your project aim to achieve?
The project aims Triage MDTs in PCN Together clinic hubs:
- provide faster paediatric input improving access
- fewer referrals to paediatrics as input and advice is given before referral
- increased quality of management of paediatric issues thr
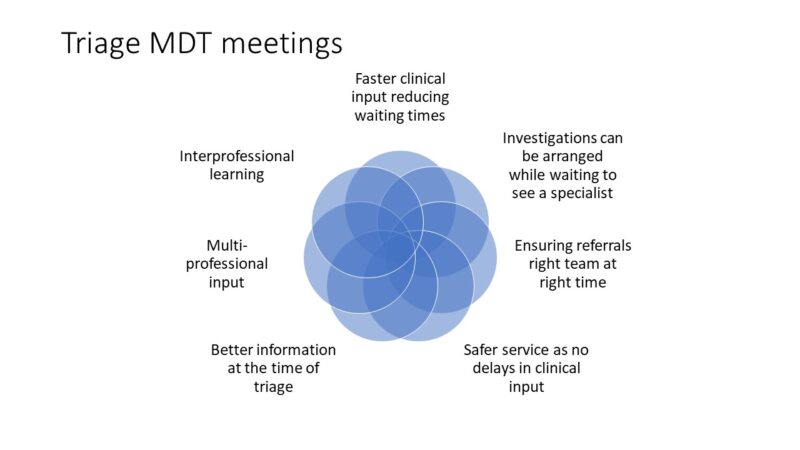 ough immediate clinical advise
ough immediate clinical advise - reduction in admin-related tasks for GP and Paediatrician (more time for clinical input)
- safer referrals as triaged together with GP/consultants (better information)
- Secondary gain to increase interprofessional learning and connection
- improving pathways of referrals if identified as suboptimal
- possibly to reduce health inequalities through focused paediatric input
- Evaluation of the impact of outcomes reduced waiting time, decreased referrals to hospital, improved CYP experience and staff experience and possible positive impact on A&E attendance within a PCN hub
- ultimately spread to all Together clinic hubs Wandsworth and Merton (at present, 12 PCN hubs)
- ‘CHILD’s’ framework used a similar model, which showed improvements
How will the project be delivered?
The project is delivered as a pilot, establishing a 1-hour weekly virtual MDT via teams in 3 PCN ‘Together clinic’ hubs in partnership with GPs.
28 1-hour MDTs are added to the existing 24 MDTs in a year. Together clinic hubs (funded already) provide weekly MDT Triage meetings. In additi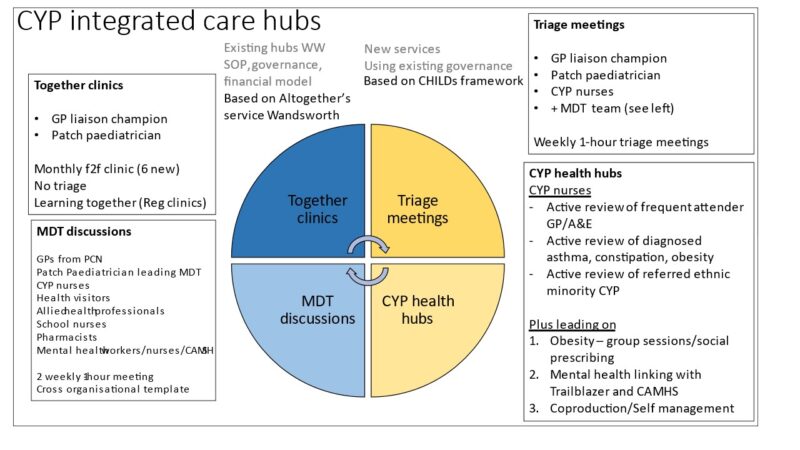 on, GP practices within a PCN will put details of patients into a PCN-shared referral template giving access to EMIS GP consultations. One GP chairs the meeting, with PCN-related GP practices joining the meeting.
on, GP practices within a PCN will put details of patients into a PCN-shared referral template giving access to EMIS GP consultations. One GP chairs the meeting, with PCN-related GP practices joining the meeting.
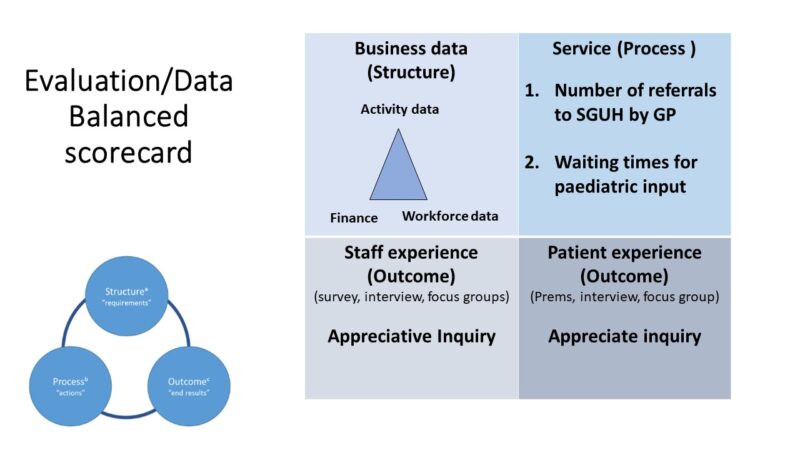
Concise data (triangulated activity data, workforce and staff) and coproduction with staff and patients ensure detailed evaluation allowing a review of impact and making service ‘business as usual’ after the pilot.
Building on existing well-trialled operational processes, standard operation procedures SOP and governance agreements in joint clinics between GPs/consultants (2monthly MDT and 1x monthly clinic Together clinic hubs) visit: https://swlondonccg.nhs.uk/news/together-clinics/
How is your project going to share learning?
 Developing a sustainable service for ‘business as usual’ service transformation. In addition developing a package of pathways, operational processes, governance assessment business plan) which can be used to establish Triage meetings in the other Together clinic hubs
Developing a sustainable service for ‘business as usual’ service transformation. In addition developing a package of pathways, operational processes, governance assessment business plan) which can be used to establish Triage meetings in the other Together clinic hubs
Through detailed evaluation and outcomes to transform acute general paediatric care expanding integrated care. Connecting further to education, health and social services, building teams around the CYP and families ending silo working within organisations.
Emphasis on coproduction with staff and patients CYPF Children, young people and families.
Detailed financial breakdown and impact – e.g. sharing co-produced surveys, Patient related outcome measures, including business model/Employment
Further plan connecting with ambulatory, NHS 111, primary/secondary/tertiary care impacting population health and shifting to prevention
How you can contribute
- Please share Ideas or existing surveys on how to coproduce - I have developed already a survey; however, open to new inputs
- Already established Standard operating procedures, pathways, risk assessments we can copy
- Digital solutions on EMIS and sharing info between hospital iclip and EMIS system
- More input regarding evaluation
Plan timeline
| 12 Mar 2023 | Finalising Analysis and evaluation report |
|---|---|
| 12 Mar 2023 | Making a case for business as usual and spread |
| 15 May 2023 | Network meeting with all 3 PCN reviewing project plan and evaluation |
| 22 May 2023 | Finalising rota with GP/consultants/admin |
| 29 May 2023 | Start of first pilot weekly TRIAGE MDTs Together Hub |
| 1 Jun 2023 | start of weekly coproduction , developing surveys including staff debriefs |
| 12 Jun 2023 | Start of second pilot weekly TRIAGE MDT Together hub |
| 26 Jun 2023 | Start of third pilot weekly triage MDT Together hub |
| 2 Oct 2023 | Focus group reviewing progress, data, enablers and barriers |
| 11 Mar 2024 | Network focus group reviewing progress, data, enablers &barriers |