Q Exchange
Novel ADHD Pathway for Adults
- Proposal
- 2023
Meet the team
Also:
- Dr Rachel Hennessey, Acting Chief Medical OfficerRaja Mukherjee Consultant Psychiatrist, Clinical Lead Adult NDD & FASD, CCIO PLD- Chief Medical Officer Project Lead
- Philippa Alisiroglu, Director of Services for People with Learning Disabilities
- Robert MacDonald, Transformation Manager
- Muqbool Khan, Senior Digital Project Manager
What is the challenge your project is going to address and how does it connect to the theme of 'How can improvement be used to reduce delays accessing health and care services'?
Context:
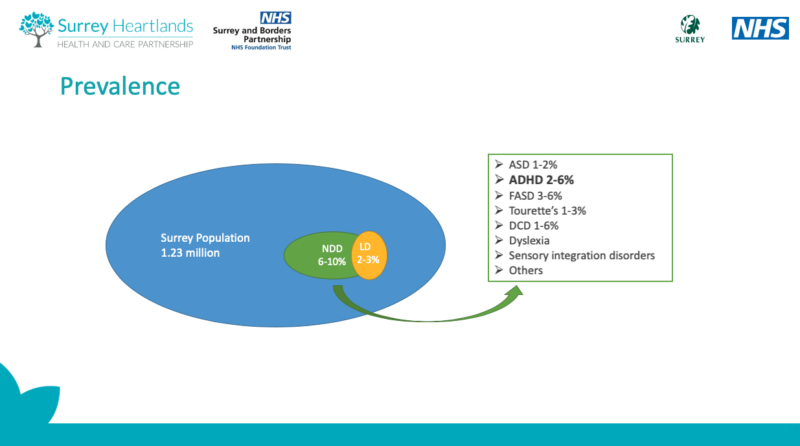
Surrey mental health services are currently experiencing high volumes of referrals with limited resources. ADHD is a mental health condition that people experience throughout their lives. ADHD undiagnosed can directly affect ability to work and lead enabled lives.
Surrey and National NHS ADHD waiting lists are very long or closing. There could be years waiting to be seen by an ADHD expert. GP’s will not assess, diagnose or treat. NHS Business Services Authority confirm demand for ADHD is soaring.
Need being assessed:
Would citizens benefit from an on-line first ADHD service?
That empowers people to:
– self-assess ADHD and better manage own care
– receive a first line of treatment that is safe, quick and effective
– including self-directed CBT and first-line prescribing of non-controlled medication
-better quality of life
– early identification of cases requiring a ‘complex case’ treatment pathway if required
-Surrey the area of focus with national scale and spread.
What does your project aim to achieve?
Aims for patients:
Empowerment for patients to self-assess ADHD (neurodevelopmental condition)
Significantly shorter waiting times
Welcome offer of intervention and support for those on waiting list
Earlier identification of ‘complex cases’ that require more intense resource
Offer of medication while waiting
Possibility of coming off waiting list if no service required
Less stigma surrounding ADHD
Systemic Outputs:
Managing demand through the system
Numbers treated
Impact on standard waiting list
Citizen’s empowerment
Better use of resources and filing workforce shortage gap
Clear data on assessment and treatment of ADHD used to further improve and align services to need
User champions of the system
Improved access to healthcare reducing current inequity
Clear numbers of people requiring to continue as per referral to ADHD wait list
Explore cost-benefits of non-controlled medication which, on first exploration, is significantly less expensive – short-term and long-term prescribing
Potential to apply this online pathway to other conditions
How will the project be delivered?
– Explore and review what other relevant online treatment pathways exist and learn from these;
e.g., smoking cessation pathway with medic review and online prescribing
– Further build on technology assessments already started
– Bring together partners within the SABP organisation and expertise across our ICS and identify early pain points, barriers and potential solutions with an ADHD CO-Design Hackathon e.g. patient groups, Pharmacies/GP’s/Nursing Teams
– Involve digital services and potential for utilising the shared record system across the ICS
– Development of pathway
– Scoping Online questionnaires/clinical assessment tools
– Clinical review and buy-in across partners of questionnaires
– Scope shared decision-making tools for ADHD
– Scoping of an online ADHD Therapy/Coaching programme
– Clinical and pharmacology partners review of prescribing
– Scope safety mechanisms required
– Development of a clinical risk assessment of this pathway
– Risk assessment of Information Governance issues
– Development of outcomes and impact dashboard
How is your project going to share learning?
We will use our Surrey Health Tech Accelerator (Partnership across the ICS with AHSN and Surrey University) as to create a working group across NHS Trusts experiencing similar problems.
An evaluation of the project for publication which will allow other trusts and organisations to build on our learning and scale up.
Thought leadership and webinars will be used as a way of sharing learning as well as developing a space on the NHS Futures platform.
Updates will be published through our online corporate channels at intervals.
– Reports and outputs will be shared on Q Exchange for the benefit of other members
Significant findings will be shared by hosting a webinar that will be recorded for YouTube/Socail Media for the general public
How you can contribute
- There are ethical questions around self-assessment and treatment being offered that is not first line NICE Guidance- we would like members views on this question given the situation.
- We welcome input from members who may share an interest or from patient groups.
- We would also like members to recommend novel approaches or care-pathways that they may have come across that support our approach.
- We also welcome support from the Q Community about sharing learning more broadly and also support in developing a community of practice.
Plan timeline
| 15 Jun 2023 | Discovery-scoping and bringing stakeholders together |
|---|---|
| 21 Jul 2023 | 2 Plan and Build stage |
| 18 Aug 2023 | 3 Test, feedback and refine stage |

Comments
Laura King 28 Mar 2023
This looks fantastic and so very needed. I wonder if you have engaged with the paediatric service / community paeds to find out how many of the target patient population are undergoing assessment for their child? Having read around this recently, it appears that some of the increased demand for adult ADD assessment [anecdotally, in adult females] is triggered by parents accessing services for their children and realising in the process that they perhaps are not neurotypical?
I wonder if there's some work there in strategies for parents and children to work on together? A very naive thought, perhaps, but timely?
Muqbool Khan 28 Mar 2023
Hi Laura, yes indeed this is something we found with Barnardos and our CAMHS Service, although resource and consent would have needed to be looked at first.
Helen Crimlisk 23 Mar 2023
An ambitious project for a colossal problem. It is certainly an area where we need to think differently as current waiting lists are untenable.
I like the idea of a digital first option and signposting/ supporting early
I have some misgivings about treatment whilst waiting - do you mean medication or something else
The focus in recent years has been on medication with much less emphaisis on self help, CBT and other coping strategies. It would be helpful to have these available much earlier in the pathway.
How will you evaluate impact on waiting lists?
How will you engage with patients and primary care (will you need shared care arrangements?
Best of luck!
(the RCPscyh has a good leaflet on this which we coproduced with a patient group)
Parya Rostami 10 Mar 2023
I really like this idea. I know how much of a difference it can make to have a diagnosis, to help you to understand your condition and make appropriate adjustments to the way you do things. There is a guy with ADHD, who shares his ADHD story through social media and how he got diagnosed later in life. He touches on some of the difficulties you mention above. He has podcasts on Spotify - https://open.spotify.com/episode/6cNdpXSuPkjb00yWTUMjbZ?si=i5R4CRb0RDC4TZsUpzbfvA
might be a good person to link in with?
Emilios Lemoniatis 20 Mar 2023
Thank you Paraya- I can listen to this on my way home tonight. Its always good to hear another person's perspective. Our aim is to help give people information so that they can move forwards in their own way- diagnosis or treatment up to them. :)
Clare Fountain 7 Mar 2023
An ambitious and worthwhile project!
Some thoughts:
- How will you make sure that the latest evidence-base interventions / self-care is incorporated?
- How will you engage patients in this project?
- Will the resources be available to patients that do not meet the diagnostic threshold for diagnosis, but still suffer symptoms? (as per NICE guideline 87)
- Ethics around self-diagnoses could be an issue - but perhaps how the support if framed so as not self-diagnosing but sharing information that "people who experience difficulty with .... may find useful"? Since this changes provision I'd suggest a review from a regional ethics committee to be sure.
Given the potential and scale of this project it might be worth putting in a bid to:
22/160 NIHR NICE rolling call (EME Programme) | NIHR
Let me know if we can help, as we work with the Royal College of Psychiatrists quite a bit. clare.fountain@hqip.org.uk
Emilios Lemoniatis 20 Mar 2023
Hey Clare
thanks so much for this/ especially the ethical question.
The answer to most of the questions are likely to be 'yes!' though the project really si to sift through these issues and come up with something novel enough to make a difference in the context.
Be great if we could arrange a chat about teh ethics- are you free for a moment on Monday 27th? Before 11?
Comments are now closed for this post.