When it comes to implementing quality improvement (QI) projects, the NHS in England faces many challenges. Often, the first of these is deciding where to place quality improvement resources for the greatest impact. Applying multi-criteria decision analysis (MCDA) can offer a transparent and structured approach to decision-making.
A recent project I’ve been involved with, funded by the Health Foundation, enabled my colleagues and I to test the use of MCDA to rank and prioritise interventions that could help to optimise medication use in hospitals.
We asked Q community members to participate in our survey, so I’m sharing these findings with thanks to everyone who took part. You can read more on our methodology in the links at the end of this blog.
Patient needs are the main focus of QI
The study looked at preferences and priorities of stakeholders for optimising medication use in NHS hospitals. We surveyed 356 people working on quality improvement, asking them to rank a set of interventions and the criteria influencing these choices.
Addressing patient needs emerged as the most influential of the 10 criteria. This underscored the importance of interventions that directly and positively impact patient wellbeing and health care experiences. The cost associated with the interventions was the second most significant criterion. Adaptability to meet local needs ranked third.
This underscored the importance of interventions that directly and positively impact patient wellbeing and health care experiences.
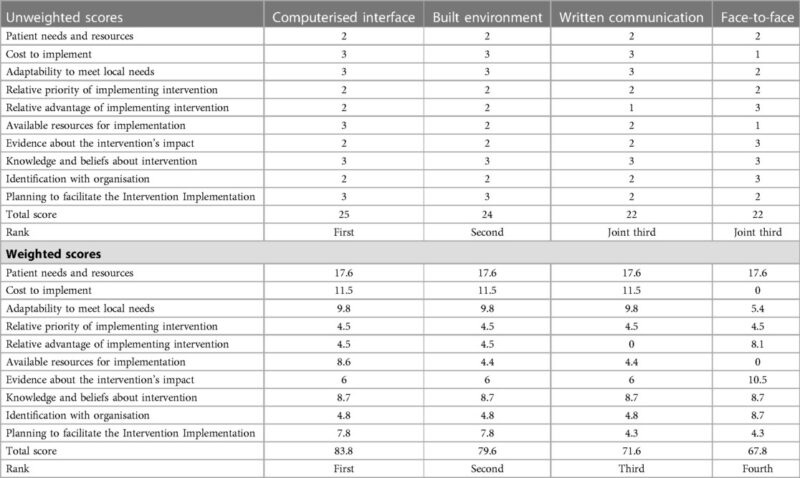
In terms of the four types of interventions tested, participants ranked them in the following order:
- computerised interface
- built environment
- written communication
- face-to-face.
The table below shows the preference ratings given for each intervention type and criteria when those scores are unweighted or weighted according to criteria preferences (see methods for additional details).
In both scenarios, our findings highlight technology-based and environmental interventions as preferable ways to deliver quality improvement interventions for optimising medication use in NHS hospitals.
While written communication and face-to-face interventions achieved third and fourth rankings, respectively, they still play valuable roles in the overall quality improvement landscape.
Using MCDA for QI projects
MCDA should be embraced as a systematic approach to prioritise quality improvement interventions, ultimately enhancing the quality of care and patient experiences in health care organisations.
‘In terms of potential uses for MCDA, there are so many areas that need improvement – medication optimisation is not the end,’ says project co-lead Kelly Schmidtke, Assistant Professor at the University of Health Science and Pharmacy in Saint Louis. ‘MCDA offers a way to engage a broader audience in making these decisions.’
MCDA offers a robust and transparent approach to decision-making in quality improvement interventions within hospitals.
While our study is the first we know of that has been used as part of a quality improvement programme, MCDA has been used in other health care settings. These include to prioritise non-pharmacological treatment options for patients with abdominal cancer suffering from chronic pain and to prioritise different groups of people who would be offered COVID-19 vaccinations when vaccines were in short supply.
Our study found that MCDA offers a robust and transparent approach to decision-making in quality improvement interventions within hospitals.
We recognise that any decision to initiate or implement quality improvement programmes in the NHS would be a multifactorial decision. However, many interventions that have the potential to be effective fail because staff do not support their use.
Understanding the preferences of the people who will be implementing and benefitting from the project can help to allocate resources to remove barriers to change.
Limitations and considerations
Sometimes MCDA gets really lost in that people think it can give them the answers. It doesn’t. It’s basically a decision-making tool that’s complementary to the other work of quality improvement.
The MCDA approach only reveals which intervention options people prefer; it does not tell us which intervention options are most likely to be effective.
The important thing is to identify your stakeholders. The stakeholders could include clinical teams, IT and – crucially – patients.
One of the limitations of this project was that we only surveyed people working in health improvement. The important thing is to identify your stakeholders. The stakeholders could include clinical teams, IT and – crucially – patients.
By incorporating stakeholder preferences, addressing trade-offs, and considering multiple criteria, hospitals can optimise resource allocation, improve patient outcomes, and foster a culture of continuous improvement.
The research team would like to thank the Health Foundation’s Behavioural Insights Research programme for the funding and all the participants from the Q community for responding to the preference survey.
Get in touch with Dr Saval Khanal or Dr Kelly Ann Schmidtke if you would like a further discussion about the project, or leave your comments in the box below.
Further information
For more details on methodology and findings, see the full project report.
Read our previous blog to brainstorm this idea: Quality Improvement Programmes: Plagued by the Paradox of Choice.