In 2019, the University of Cambridge set up a partnership project to look more deeply at system-level improvement issues. Emma Adams and I were part of the project team, and our focus was on tailoring the improvement approach to health care.
Along with the University of Cambridge, the partners included The Royal Academy of Engineering, The Academy of Medical Sciences and The Royal College of Physicians.
We have now launched a free online improvement toolkit that draws on engineering theory and expertise. It has been designed for use on its own or alongside an organisation’s existing tools and resources.
Building on the success of Engineering Better Care (2017), a landmark report into applying a systems approach to continuous improvement, we sought to co-design an improvement methodology for health and social care that was human-centred, systems- focused, and holistic.
The task we set ourselves was to develop a set of practical tools for organisations that would respond, continuously, to the care needs of a changing patient population. Beyond the creation of a set of tools, we also wanted to establish a self-sustaining forum for active discussion and learning where success is measured by interaction with the improvement tools and stories of their use.
The UK’s health and social care system is one of the largest and most complex of our national assets. As the Engineering Better Care report put it:
“Successful transformation must take into account the needs of all patients, carers, healthcare professionals and other staff. It requires consistent consideration of every element of the system, the way each element interacts, and the implications of these interactions for the system as a whole – that is, it requires a ‘systems’ approach.”
Engineering Better Care, p7, 2017
We looked across improvement work to identify some of the biggest challenges and pitfalls. One of these was the tendency for a team to leap to solution mode, and not give sufficient attention to the subtleties and complexities involved.
With complex systems, there is sometimes more to be gained from slowing down and looking into a problem more deeply and iteratively than from reacting to what is happening on the surface.
We learned a lot about how to improve health care from the patients we encountered as part of this work. One example is Mrs G, a frail 80-year old woman who lives alone and has a fall. Mrs G showed us a lot about how we could change the way we worked.
In one scenario, which will be familiar to many who work in healthcare, after her fall Mrs G rings an ambulance and is admitted to hospital for treatment where she ends up in a bed for several days. This outcome is often the result of difficulty establishing the precise cause of the fall, lack of access to the patient’s GP record of treatment, and lack of extra support or assessment to enable the patient to go home. After spending several days in hospital, the patient then loses the confidence to move unaided.
After working through her case, we came up with a model of care that identified frailty as a priority issue for Mrs G’s area. With this approach in place, after her fall, Mrs G calls a number given to her by her community support group. A community nurse treats Mrs G in her home, working with the community-based team and updating Mrs G’s family. The nurse arranges a visit from a speciality frailty nurse the following day. This nurse sets up both short term extra support and longer term care options for Mrs G, keeping her family and her multi-professional team informed. Mrs G is happy with the outcome and her family are reassured that plans are in place to deal with any future problems.
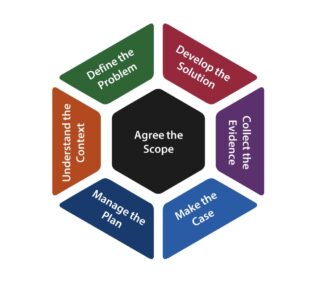
Using a set of visual aids incorporating an improvement model (see image) and a question map, we worked through examples such as these to carefully consider the complexities of these cases, looking at people, processes, technologies, and systems that, in turn, are part of other systems.
We wanted to push ourselves to think around problems, and tap into our curiosity. Curiosity is one of an improver’s most powerful tools.
One of our biggest risks was that our model would clash with other improvement approaches that organisations were already using. To work around this, we considered which elements of improvement are generic to all improvement models and established a thinking framework grounded in these.
Our framework emphasises four core elements: people, systems, design, and risk. The challenge is to ensure that all four elements are working in an integrated and well-ordered way.
As our programme had been designed before COVID 19, mid-way through this work we had to move all of our activities online, which had some unexpected challenges and benefits. While it was clunky at first, as we adjusted to using a virtual platform, we did find that it was logistically easier to arrange events online.
One of the most important outcomes of this work has been that the improvers themselves have co-produced their own storytelling culture.
The Improving Improvement Toolkit is able to be used by any organisation wanting to start improvement work in health and social care.
Equally, organisations already using an improvement approach can adapt the toolkit to enhance or sense-check their own approach.
We hope these tools will be of use to all improvers and we warmly welcome you to become part of our improvement journey.