Q Exchange
Lost in the system: Integrated care for complex pain
- Proposal
- 2024

Meet the team
Also:
- Dr Katherine Irving, Dr Biba Stanton, Dr Tim Segal, Prof Mark Edwards, Prof Trudie Chalder, Dr Catherine Stack
What is the challenge your project is going to address and how does it connect to the theme of 'How can we improve across system boundaries?
Current provision for patients with chronic pain seriously fails the 20% with the most complex needs, who utilise 80% of the pain-related healthcare resources.
For these patients, pain results from psychophysiological changes that produce multiple physical symptoms and many have high mental health needs. They are sent to multiple different services, producing fragmented, slow and ultimately ineffective care.
Our approach could get patients to the right treatment more quickly and prevent unnecessary appointments. We will offer a Treatment Planning Conference where patients and their families work with a consultant with expertise in pain and mind-body interface to create a personalised treatment plan.
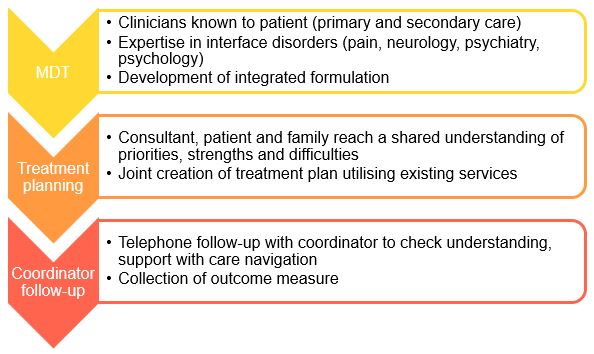
This will be supported by:
· A pre-conference MDT (with clinicians from primary and secondary care, physical and mental health) to integrate previous assessments.
· Post-conference follow-up with a pathway coordinator, to help the patient access the recommendations made.
What does your project aim to achieve?
Objectives:
1. To co-develop a personalized holistic treatment plan with people with complex pain and their families.
2. To provide expertise to support development of the treatment plan from a multi-disciplinary team.
3. To support the implementation of the personalized treatment plan through a pathway coordinator.
Benefits:
1. Quicker access to right service(s)
2. Reduction in unnecessary appointments and investigations.
3. Improved patient understanding of their condition and ability to self manage with reduced functional disability and better quality of life.
4. Build capacity by increasing confidence amongst clinicians in the biopsychosocial approach to complex pain.
5. Gather evidence to determine the clinical and economic outcomes of this model, allowing replication at other centres
Inequality:
Complex pain disproportionately affects people from deprived and minority communities. The project will be based in Lambeth, an inner London borough, ranked amongst the 15% most deprived in the country. We will proactively identify patients who experience barriers to accessing care.
How will the project be delivered?
The pilot project will run for 1 year, working alongside GP practices in Lambeth.
Patients with chronic pain who cannot access existing community interventions due to their high complexity will be offered a Treatment Planning Conference.
MDTs will run online fortnightly for one hour to discuss two patients. Uniquely, the MDT will include clinicians from multiple specialties and disciplines as well as community services.
Treatment Planning Conferences will run face to face fortnightly (2 x 2 hour appointments). The conference will use a collaborative approach with the patient and their family, based on rehabilitation principles, including discussion about illness attributions that might be barriers to increasing activity. The pathway coordinator will support running the MDT, attend conferences and offer telephone follow-up. They will also lead outcome measure collection and evaluation. We anticipate that about 40 patients will come through the pathway over the one year pilot.
How is your project going to share learning?
We will report the following data
· Patients utilising the service from a defined population
· Patient satisfaction with care
· Patient understanding of their condition
· Healthcare costs in 6 months before and after
· Confidence in managing chronic pain in clinicians attending MDTs
We will identify areas of unmet need within treatment services for chronic pain.
This will allow us to model the costs of implementation for a given population compared with the potential cost savings. We will present these data to the Southeast London Integrated Care Board with a view to commissioning a scaled-up version of this service across their six boroughs.
We will invite clinicians from other UK centres to observe our MDTs to share our model and learning.
We will submit data for presentation at conferences (British Pain Society, Faculty of Liaison Psychiatry, Association of British Neurologists and the British Society for Rheumatology) and for publication.
How you can contribute
- We would like advice from the Q community on how best to share learning from this project.
- We’d also appreciate suggestions from anyone with experience in implementing MDT-based or care coordination based interventions for complex disorders.
Plan timeline
| 1 Aug 2024 | Project begins. Pathway coordinator in post. Start identifying cases |
|---|---|
| 9 Sep 2024 | MDTs and treatment planning conferences start |
| 1 Jun 2025 | Continue telephone follow-up and data collection |
| 1 Aug 2025 | Pathway coordinator contract ends |
| 1 Dec 2025 | Project team complete data collection and analysis |
| 1 Apr 2026 | Complete sharing of learning and promotion of wider adoption |
Comments
Owen Hughes 14 Mar 2024
An interesting project. I'd be keen to know more about a few things:
- how does this vary from pain teams who are already offering an MDT assessment?
- how will you identify the 20%?
- what about the impact on social aspects of life (work, family etc)?
- you mention consultant assessment, is this just medical consultants or will it involve psychologists and AHPs?
Simon Anderson 12 Mar 2024
This is a really important initiative. These patients do not have access to the right clinicians and this project is vital in correcting this deficiency. The team is knowledgeable and effective in working in the MDT format and will provide a great service for these struggling patients.
Dr Martin Johnson 10 Mar 2024
I fully support this excellent project. Chronic pain patients are often the victims of 'revolving door' investigations and treatments with no overall plan. This is to the detriment of the patients, their families and the NHS.
Martin Johnson
RCGP Representative for Chronic Pain.
Past Vice President & Hon Secretary of the British Pain Society
Dr Lorraine de Gray 8 Mar 2024
A laudable project in keeping with the FPM Four Nation Pain strategy (https://fpm.ac.uk/four-nation-strategy-pain-management) - promoting patient focused care from point of first contact including, self-help, signposting, personalised care and shared decision making.
I look forward to reading more about this project as it progresses and hope that the evidence collated will help to fund other similar projects across the country.
Well done to all involved!
Geoffrey Warwick 8 Mar 2024
This is a great idea, and badly needed. There is a huge unmet need for patients like this, and they sorely need to have services developed for them. Patients suffering with chronic pain tend to be funnelled into to clinics that aren't set up to meet their needs, which can lead to them being prescribed treatments that don't work. Offering them a dedicated, multi-professional MDT will mean their cases can be looked at in a more holistic way, making it more likely they will be given an appropriate treatment plan, with a better chance of recovery.
Andrew P Baranowski 6 Mar 2024
The needs of those living with pain who also have complex issues radically over whelms the current NHSE specialised service provision. It is clear that there needs to be a ‘hub and spoke’ mechanism in place to support decision making and to enable care at community level for these complex cases. This is something recognised by the NHSE Adult Highly Specialist Pain Management Service Specification, but has been poorly instigated This is partly because of lack of resources; but, also a lack of evidence for the most appropriate model. This project will provide evidence around one very sound approach and as such is worthy of support. The outcomes of this project may potentially improve the lives of many thousands if not 10s of thousands of individuals UK wide.
Andrew P Baranowski
Consultant Pain Medicine UCLH and Honorary Associate Professor UCL
Past President The British Pain Society and Past Chair NHSE CRG for Adult Highly Specialist Pain Management Services
Catherine Stack 6 Mar 2024
This will be a very useful project to help the complex patients in the chronic pain service at Kings.
Sabrina Bajwah 6 Mar 2024
As a palliative care consultant, I often see patients with pain. Their care is so fragmented and communication between all those involved in their care is fragmented. This is a great proposal to address all those issues.
Sophie Harris 6 Mar 2024
Such a fabulous project to support these really complex people and help reduce admissions and unnecessary investigations/medications. care coordinator will help to build the case and communicate across boundaries
Jeremy Johnson 6 Mar 2024
A vital and timely project that would substantially benefit a large number of patients poorly served by current practice and with the potential to substantially reduce healthcare costs.
Rebecca Cathersides 6 Mar 2024
This is an amazing multiprofessional project focusing on improving access for a patient group that already face multiple inequalities, I really hope it is given the opportunity to flourish”.
James Galloway 5 Mar 2024
This project is excellently devised, tackling a crucial aspect of clinical management. There is a dire need for multidisciplinary team (MDT) care for chronic pain.
The burden of chronic pain is a significant and complex challenge within the healthcare system, affecting countless individuals' quality of life. Chronic pain management requires a comprehensive and multidisciplinary approach. However, patients frequently find themselves navigating a fragmented healthcare landscape, where care is delivered in siloes. Such a disjointed approach can lead to patients being shuffled between specialists without a cohesive plan.
Bridging these siloes and fostering a more collaborative, multidisciplinary approach is essential for addressing the intricate needs of individuals suffering from chronic pain, ultimately leading to improved outcomes and patient satisfaction.
It is great to see this project addressing these issues.
Eche Anakor 5 Mar 2024
This sounds like an exciting, meaningful project which seeks to embed a codeveloped personalised, holistic approach to chronic pain which can improve the lived experience of those living with chronic pain in Lambeth and addresses the health inequalities within this space. Learning from this will be valuable to the chronic pain workstream within Lambeth (NWDA) and wider across south east London
Emily Jay 5 Mar 2024
This project is an important project this patient group are often passed from pillar to post by each specialism a team to co-ordinate and make shared decision about how to best manage their complex presentation and ceilings of care/investigations are an important so that patient can access the correct treatment pathway
Rachael Jarvis 5 Mar 2024
A really important project designed to target the needs of patients and their families who are continuing to suffer under the current system. The proposal looks really thought out and by gaining a better understanding of the patient care in a more joined up way, could also lead to improvements in care more broadly across the population.
Cormac Fenton 5 Mar 2024
This is an excellent project. I see patients in acute hospitals who's complex pain has led to a huge impact on their mental health and quality of life. This kind of work is vital for this group of people.
Natasha Curran 5 Mar 2024
Chronic pain is going to be an even bigger public health problem in this country soon: https://www.health.org.uk/publications/health-in-2040. And people with the most complex pain (and other issues) that are not well addressed will use a huge amount of our valuable resources. So this is a brilliant project to ascertain what might help them and conserve healthcare!
I would love to see this project move forward with support from Q as more data is needed in different systems, in order to demonstrate the relative costs and benefits for patient, staff and health system. This can then be evidence to develop and adapt services across the country.
Natasha Curran, Consultant in Pain Medicine, University College London Hospitals, Medical Director, Health Innovation Network
Implementation & Involvement Team Lead, Applied Research Collaboration South London
Joseph Casey 5 Mar 2024
Important project addressing the unmet needs and fragmented service experience of many people experiencing complex pain. From experience supporting family members, I understand the complexity of navigating health services and the importance of the proposed project to meeting this need
Sarah Dheansa 29 Feb 2024
Very much needed to improve the pathways for this short of patients .
David Okai 29 Feb 2024
This is an integrated approach to pain. The greater the complexity of the patient, the more the need for a full MDT approach. This bid is supportive tot he evidence base in this regard. The evidence suggests a significant improvement in function following such interventions (interestingly, this is in the context that patients often rate the severity of pain the same. In other words, the pain may not be perceived to improve, but the patient is able to perform better in social and occupational activities.
Comments are now closed for this post.