Q Exchange
Establish collaborative Transfer of Care Hub (TOCH)
- Proposal
- 2024
What is the challenge your project is going to address and how does it connect to the theme of 'How can we improve across system boundaries?
Direct observations, staff engagement, and patient feedback identified opportunities to improve the allocation of community support for patients no longer requiring care in an acute setting.
Contributing to delays leaving hospital, the current process necessitates wasteful activity, including excessive data entry, sub-optimal information sharing, and disparate information management systems.
To ensure optimal outcomes and alignment with best practice, the patient’s needs and support options must be comprehensively considered by those best equipped to do so.
This project will increase engagement with patients and their support networks to improve overall patient experience, understanding and maximise information gathered to inform allocation of support (without repeated requests).
Over 40 patients, carers, and muti-disciplinary/multi-agency stakeholders were empowered to improve this process in a 5-day workshop, using tools from the local management system (SASH+). This project idea was collaboratively generated, to reduce waste, add value, and increase productivity.
What does your project aim to achieve?
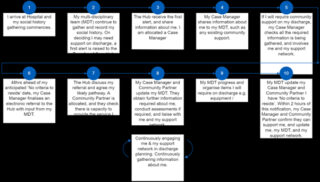
This project aims to operationally support and develop a collaboratively designed process, enabling early discharge planning. This includes earlier patient and support network involvement, social history gathering, community provider input, and allocation of a responsible operator to support each patient’s discharge. Informed by the patient and those who know them best, a holistic description of their needs will be provided to a new joint hub, aligning with statutory guidance. This will allow optimum community support options to be collaboratively identified with community experts and planned before the patient is ready to leave.
The foundational aim is to produce a patient centred process, with involvement throughout and improved outcomes owing to patients receiving the right support, at the right time. Early exploration of tailored and specialist support options will reduce health inequalities. Flow will be optimised across the system, with an improvement culture embedded in the process design and implementation.
(https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1101030/Transfer_of_Care_Hub_-_Hospital_Discharge_Action_Cards_Revised.pdf)
How will the project be delivered?
A system-wide programme of work must now develop, test, and implement the designed future state process. Detailed analysis of the current process has been completed, identifying those impacted. These individuals will continue to be empowered to improve the process, including engaging the patient voice, particularly from less represented communities.
Risks will be managed under a governance framework with a Senior Responsible Officer appointed. Senior representatives from adult social care, the community and other system stakeholders have already been appointed to support delivery.
Implementation will be developed and co-ordinated with project management support. The roll out will include establishment of working groups and improvement events, with accountability, sustainability, and reflection opportunities maintained through regular meetings and reporting to monitor progress against key actions and defined metrics.
Value for money will be delivered by savings associated with improving productivity, system-wide flow, and allocation of resources.
How is your project going to share learning?
Lessons learnt from this project will be captured and shared with Q members and the wider system through regular updates, including mid and final reports. In addition to lessons involving tackling the national challenge of ensuring timely and appropriate discharge and provision of community support, the improvement methodology and tools used to generate, design, and implement this project can also be shared.
The project team will participate in Q exchange activities and arrange a shared learning event for key stakeholders to see the project in action. The local management system (SASH+) utilises a well-established shared learning process, enabling the capture of the successes and improvement opportunities, and already hosts open days and courses accessible to the wider system.
The project focusses on the East Surrey population. However, shared learning has already been undertaken, with out of area system partners engaged in conception and design of this project.
How you can contribute
- As well as sharing lessons learnt from this project the project team are also keen to take learning from others to help inform and support the design of this idea. Particularly around how other systems have:
- • Established successful Transfer of Care Hubs;
- • Created transparency of demand and capacity across the system, how the information is shared in real time and the use of technology to enable this (bespoke or adaptation of an existing platform);
- • Implemented Discharge to Assess successfully into a similar process, how this has been embedded and impact on operations;
- • Utilised capacity to match demand for community services or, when demand outstrips capacity, how operations are managed to avoid sub optimal patient outcomes; and
- • Shared information across organisational boundaries to support with identification and delivery of optimal community support
Plan timeline
| 25 Mar 2024 | Design structure, function, roles, and responsibilities across the system |
|---|---|
| 6 May 2024 | System-wide communications detailing information on formal and informal training sessions |
| 5 Aug 2024 | Live trails alongside PDSA cycles and refinement of process |
| 14 Oct 2024 | Phased go live ahead of winter pressures |