Q Exchange
Parents in the Driving Seat: What Matters in Neonatal Follow-Up?
- Shortlisted idea
- 2024

Meet the team
Also:
- Hilary Wong (Consultant Neonatologist and Research Workstream Co-Lead, British Association for Neonatal Neurodevelopmental Follow-up)
- Claire Marcroft (Academic Neonatal Physiotherapist, expertise in qualitative research)
- Emily Gorrod-Smith (Expert Parent)
- Jessie Cunnett (Point of Care Foundation; Expertise in Experience-based Co-Design, Patient & Staff Experience and Implementation Support)
- Rachel Stamp (Lead Neonatal Physiotherapist, EoE ODN)
What is the challenge your project is going to address and how does it connect to the theme of 'How can we improve across system boundaries?
Follow-up of infants born preterm after neonatal intensive care discharge is essential to optimise long-term health and educational outcomes. Matching clinical resources with patient needs, while maintaining equitable access and maximising patient experience is the challenge we seek to address.
Current follow-up care provision straddles across multiple system boundaries (home, primary and secondary care, and education) and are problematic:
- Age-specific health and developmental assessments are manually coordinated, leading to delayed or missed assessments.
- No reliable system to triage and coordinate appointments according to needs.
- Poor clinic attendance rates due to parental disengagement and access issues.
- Variable information sharing across systems.
Digital technologies offer potential solutions:
- Automate the process of assessment administration.
- Capture of parental concerns empowers shared decision-making and facilitates care triage.
- Synchronisation with electronic health records.
Familiarity with telehealth accelerated during COVID-19 but the integration of digital technologies in neonatal follow-up has not yet been systematically adopted or evaluated.
What does your project aim to achieve?
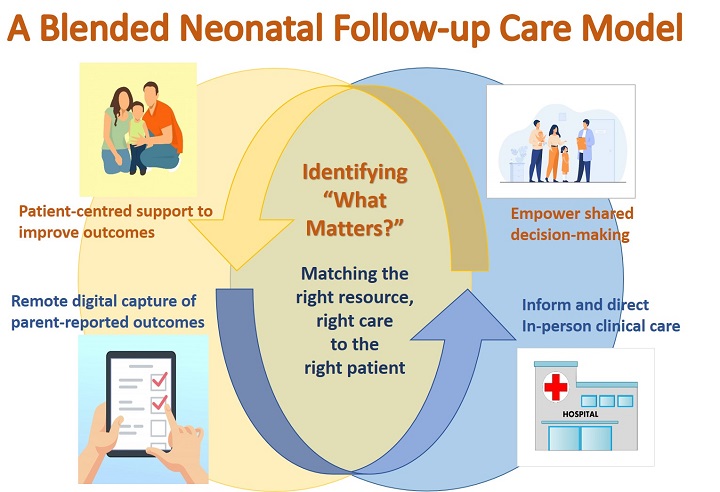
Our project aims to develop a ‘blended follow-up care model’ that allows remote digital capture of parent-reported outcomes (‘what matters the most?’), which are fed back to clinical care teams to enhance in-person follow-up.
This digital-facilitated model will:
1) Increase productivity and reduce waste
- Automate the delivery of parent-completed health and developmental questionnaires.
- Seeking parental perspective on ‘what matters most’ improves engagement, shared decision making and reduce missed appointments.
2) Reduce waits sustainably and equitably
- Improve access to parental questionnaire-based health and developmental assessments that act as an initial screen, enabling a triage process and target clinical resources to those in need.
3) Embed improvement into management systems and processes
- Parent-reported measures will be shared with all professionals involved in the child’s care as a function of the platform.
- Synchronisation of the outcome measures with the child’s neonatal electronic health records enable systematic collection of valid outcome data in cross-system levels improvement work.
How will the project be delivered?
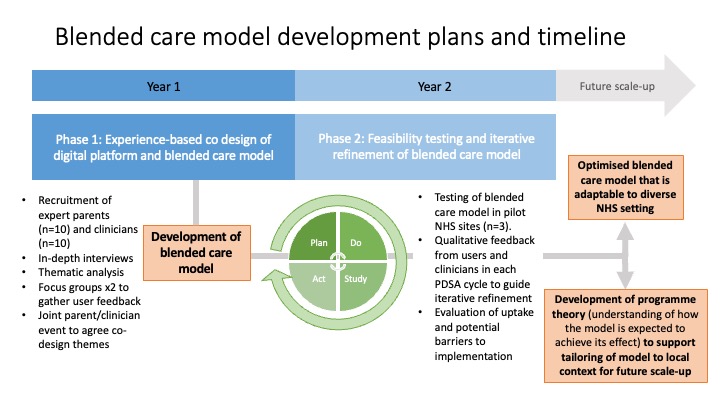
Phase 1 (Months 1-12): Experience-based co-design (EBCD) of the digital platform and blended care model
Supported by EBCD experts from Point of Care Foundation, we will hold focus and co-design working groups with expert parents and clinicians to inform the design of this new care model, prioritising stakeholder experience. We will adapt an existing electronic data capture platform (with proven functionality in administering questionnaires directly to families and results feedback to clinicians) and develop an optimal model of integration with clinical care.
Phase 2 (Months 13-24): Feasibility testing and iterative refinement
We will test the feasibility of the new blended care model with cohorts of parents and clinicians. Through repeated PDSA cycles, we will evaluate the implementation, uptake and user experience, and iteratively improve and increase the adaptability of the model to different settings within the NHS. This knowledge will form the initial programme theory to support future scale-up efforts.
How is your project going to share learning?
UK neonatal services benefit from a regional network-based system of care. The East of England has already developed an award-winning neonatal neuroprotection service set up with funding from the Health Foundation, which will allow this project to be embedded in all 17 neonatal units.
The project is scalable across networks throughout the UK through national organisations such as British Association for Neonatal Neurodevelopmental Follow Up (BANNFU) which is an affiliate of BAPM (British Association of Perinatal Medicine) and BLISS charity. Learning from this project can be shared with both service providers and family groups, through the QI story board, IHI websites, social media platforms, presentations and publications.
Significantly the learning from this project can be translated to other critical care situations such as cardiac or paediatric intensive care follow up.
The landscape of virtual communication tools is complex and ever-changing and our learning will therefore be valuable to any healthcare provider.
How you can contribute
- Experience - Many Q members have experience of digital tools and embedding them in NHS practice. Developing secure digital tools in the NHS environment is important to ensure appropriate security and governance. Therefore, learning from others experience and sharing our knowledge is fundamental to the success of this project.
- Sharing - We passionately believe that improving communication with families and relatives is fundamental in improving trust in professionals and developing a collaborative approach to healthcare, so will be excited to help share and support other teams wanting to use this approach.
- Learning - Critical and constructive feedback from Q members will help us develop and think outside the box.
- Support - with QI methodology and implementation science will be vital and will ensure timely rollout.
- Dissemination - The Q community will enable our learning to be spread to other areas of healthcare outside our own specialty.
Plan timeline
| 15 Aug 2024 | Project commencement: Project team planning meeting |
|---|---|
| 15 Sep 2024 | Initiation of Phase 1: Recruitment of co-design members |
| 30 Nov 2024 | Conclude in-depth interviews of expert parents and clinicians (co-design members) |
| 5 Jan 2025 | Thematic analyses of interviews |
| 28 Feb 2025 | Clinician feedback to check themes from interviews |
| 20 Mar 2025 | Expert parent focus groups |
| 15 May 2025 | Joint clinician and parent feedback event to agree co-design themes |
| 31 Jul 2025 | Check-in with co-design members to ensure care model meets brief |
| 31 Aug 2025 | Initiation of Phase 2: Recruitment of parents to test care model |
| 30 Nov 2025 | Project team meeting to evaluate feasibility testing and refinement |
| 20 Feb 2026 | Stakeholder meeting to evaluate care model |
| 30 Apr 2026 | Further project team meeting for ongoing evaluation |
| 15 Jun 2026 | Project team meeting to agree components of programme theory |
| 30 Jun 2026 | Develop digital platform and formalise blended care model |
| 31 Jul 2026 | Formalise blended care model, celebratory event and conclusion of project |
Comments
Nazakat Merchant 6 Jun 2024
Dear Anthony,
Thank you for your very insightful thoughts and feedback.
- We have an existing PPIE group of expert parents with lived experience who have been actively involved in the development of this project, from the conception of idea through to shaping the methods and Q exchange application.
- We have planned for focus groups for clinicians and parents to be held separately initially to tease out specific themes for each group, and then jointly to establish the vision and resolve concerns. We have within our team, experienced qualitative researchers with expertise in staff and patient experience to lead the Experienced-Based Co-Design.
- Equality within the group dynamics is something we will be very mindful of when inviting focus group members and facilitating the group – thank you for highlighting this.
- Similarly, we may have to adapt strategies to gain insights from seldom-heard communities, perhaps through direct 1:1 communication outside the focus groups.
- Digital exclusion is a very real concern for us. From our early PPIE work, we have recognised that any digital tools introduced into routine practice should be offered as a patient choice, rather than being mandatory. We will be seeking to keep non-digital means to avoid discriminating against those who cannot (or choose not to) use digital health care services.
Anthony Fryer 29 May 2024
I'm interested in the public involvement elements of this project. Sounds interesting, but I have a few things for you to consider. How were parents involved in its development? How will you ensure there is equal power in the focus groups? Will they be involved in the development of the specification for the digital platform. How will seldom-heard communities be involved. What about the risk of digital exclusion.
Comments are now closed for this post.