A huge thank you to the 427 members who completed the first Q Insight Survey: Improving Outpatient Care. The results provide rich perspectives on this crucial topic, well demonstrating the potential of the community’s collective insight. Some of the findings have already been put to Simon Stevens and my colleague, Sarah Reed, has drawn out the key learning for policymakers and system leaders so that Q members’ knowledge and experience can inform developments across the NHS.
This blog draws out some of the most useful results for Q Exchange projects as they enter their refinement stage.
Great importance, little progress
The vast majority (89%) of respondents saw improving outpatient care as either extremely or very important even in comparison to all other challenges currently facing the NHS. Yet, 51% felt there had been little or no progress within their area over the last decade. Taken together these results support a renewed focus on improving outpatient care but suggest we need new ways working, such as Q Exchange, to drive forward the desired progress.
Multiple solutions may be required
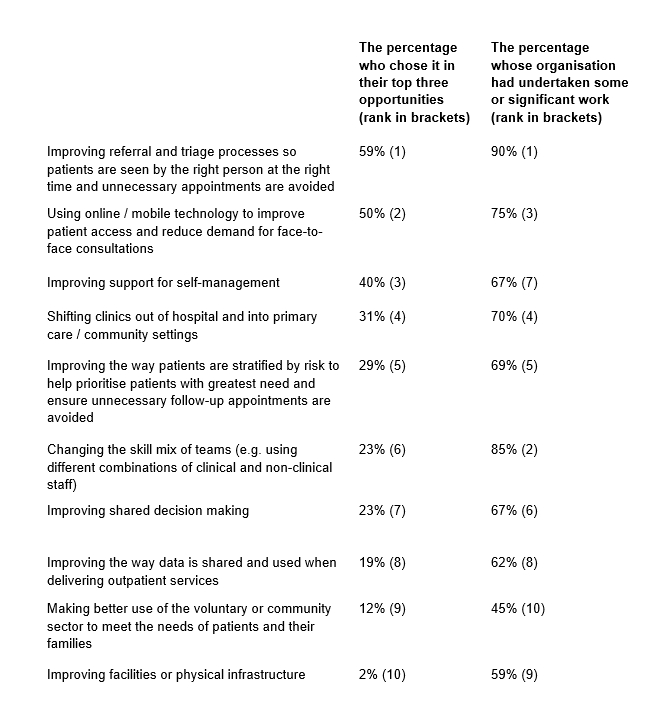
Respondents identified a wide range of opportunities for improvement and it is likely that multiple approaches will be needed to ensure progress – good news for potential Q Exchange projects! However, as seen in the table below, some opportunities were much more highly rated than others. With the option to select up to three, the top-rated opportunities were around improving referral and triage processes (59%), using online or mobile technology (50%) and improving support for self-management (40%). Perhaps surprisingly, a relatively low percentage of respondents chose making better use of the voluntary or community sector (12%) or improving facilities or physical infrastructure (2%).
Lots of experience to learn from
Over half (52%) of respondents had direct experience of improving outpatient care and, as seen in the table below, work has been undertaken across a wide range of areas – crucial for those wanting to learn from what has already been done. Overall, there was fairly close alignment between the areas where respondents saw the greatest opportunities and areas where organisations had undertaken work with improving referral and triage processes (90%) also coming out top. The two most notable differences were in improving support for self-management being more highly ranked as an opportunity relative to the work undertaken and the opposite being true for changing the skill mix of teams.
Work improving outpatient care compared to the percentage who chose it as a top three opportunity for improvement
How to support successful improvement
Our analysis, especially of the free text questions, suggests that respondents see a range of success factors in improving outpatient care, which we hope will be useful for Q Exchange projects. Perhaps unsurprisingly, they act as a strong call to arms for quality improvement methods.
Ensuring patient involvement – ranging from user research to understand experience to much more substantial co-design and iterative collaboration.
Ensuring staff buy-in – including clear communication and vision across the whole team and mobilising staff champions. This was especially highlighted around increasing virtual consultations.
Taking a system-wide perspective – clearly not all projects will do this, but many respondents emphasised the importance of considering how work will impact on the wider pathway – for example, looking beyond outpatient services to include primary care and community care, taking multidisciplinary approaches, or considering how data is shared.
Get the basics right – sixty-four percent thought that a barrier to significantly increasing virtual consultations was access to and reliability of new technologies. It may well be outside the scope of Q Exchange projects to invest in more reliable tech but such fundamental barriers clearly need to be considered in project design.
Learning from others – many respondents emphasised the need for sharing with and learning from others and Q Exchange projects should stand on the shoulders of the work already undertaken as much as possible. Useful examples of successful projects can also be seen in the Health Foundation briefing paper on outpatient redesign.
Testing and learning – finally, respondents stressed the importance of time for designing, testing and iterating new ideas and ways of working and capturing the learning in order to ensure successful and sustainable improvements. The NHS doesn’t always create the space and support for this sort of iterative approach – but hopefully Q Exchange can help.
Next steps for Q’s outpatients work
In recognising that sustainable improvement will require multiple sources of expertise to come together, Q is adopting a co-ordinated focus on outpatient care during 2019/20. Building on the insight survey and the Q Exchange funding, we hope to bring together learning and expertise through the UK-wide Q community event, Q visits and through our work with country partners across the UK. We will share the full results from the survey in due course but please contact Matthew Hill for more information in the meantime.