Improving across health and care systems: a framework
On this page
Introduction
To achieve sustainable improvements across multiple organisations and hierarchies, leaders from across systems need to come together to plan and deliver work holistically. This complex work is hard to navigate, with activities needed from across multiple organisations and hierarchies to deliver large-scale change effectively.
We developed this learning framework in collaboration with leaders from across the health and care sector. The framework, and its accompanying tools, can be used by those developing strategies to improve health and care across systems. It supports leaders to recognise, navigate what’s available and holistically plan the ways improvement, and related fields, can work together to deliver large-scale change. It has also been designed to help work through what NHS IMPACT means in practice for systems.
We will be using, and continuing to develop it, through our peer-learning programme which is being delivered in a partnership between the Health Foundation, the Q community and NHS Confederation.
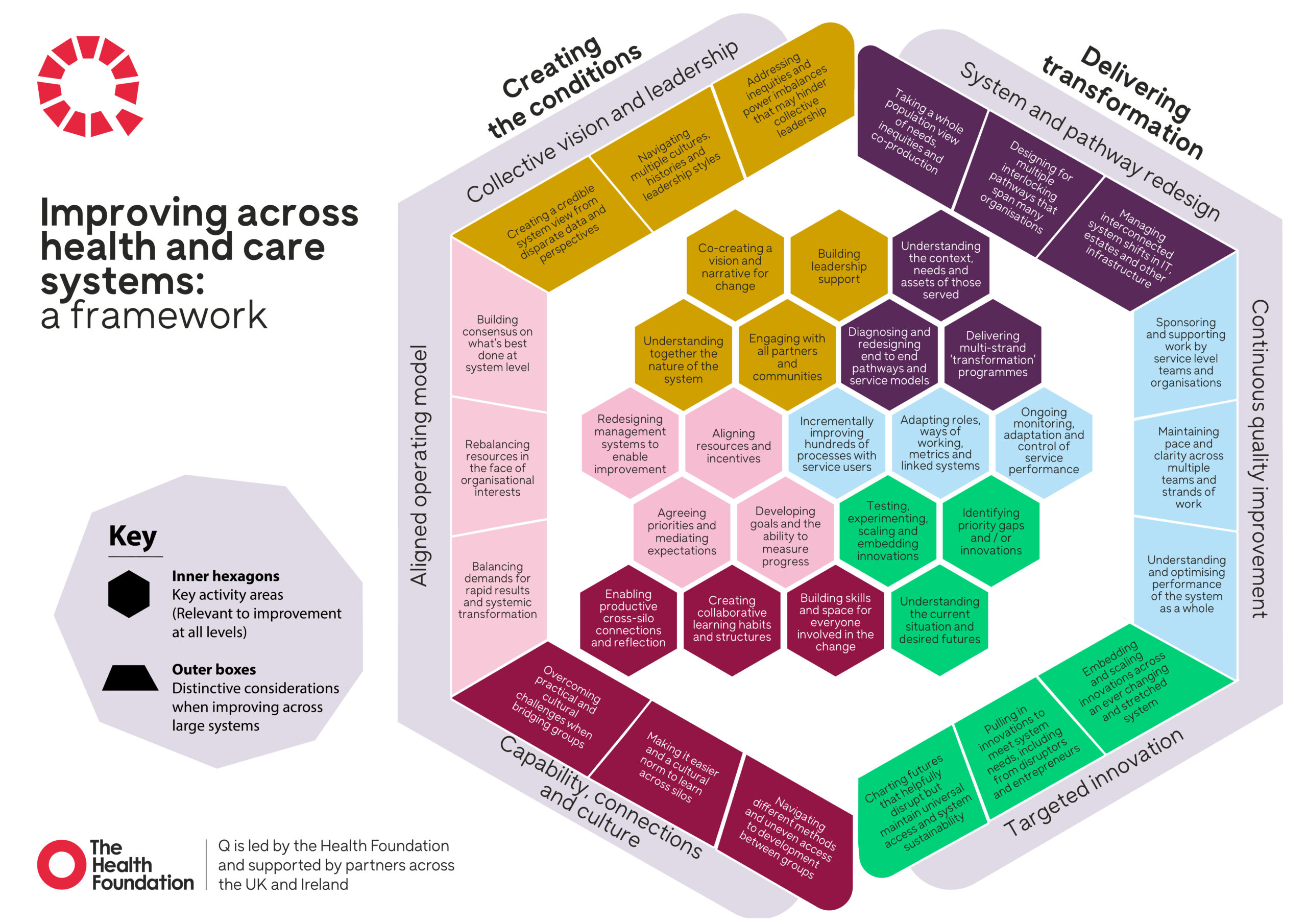
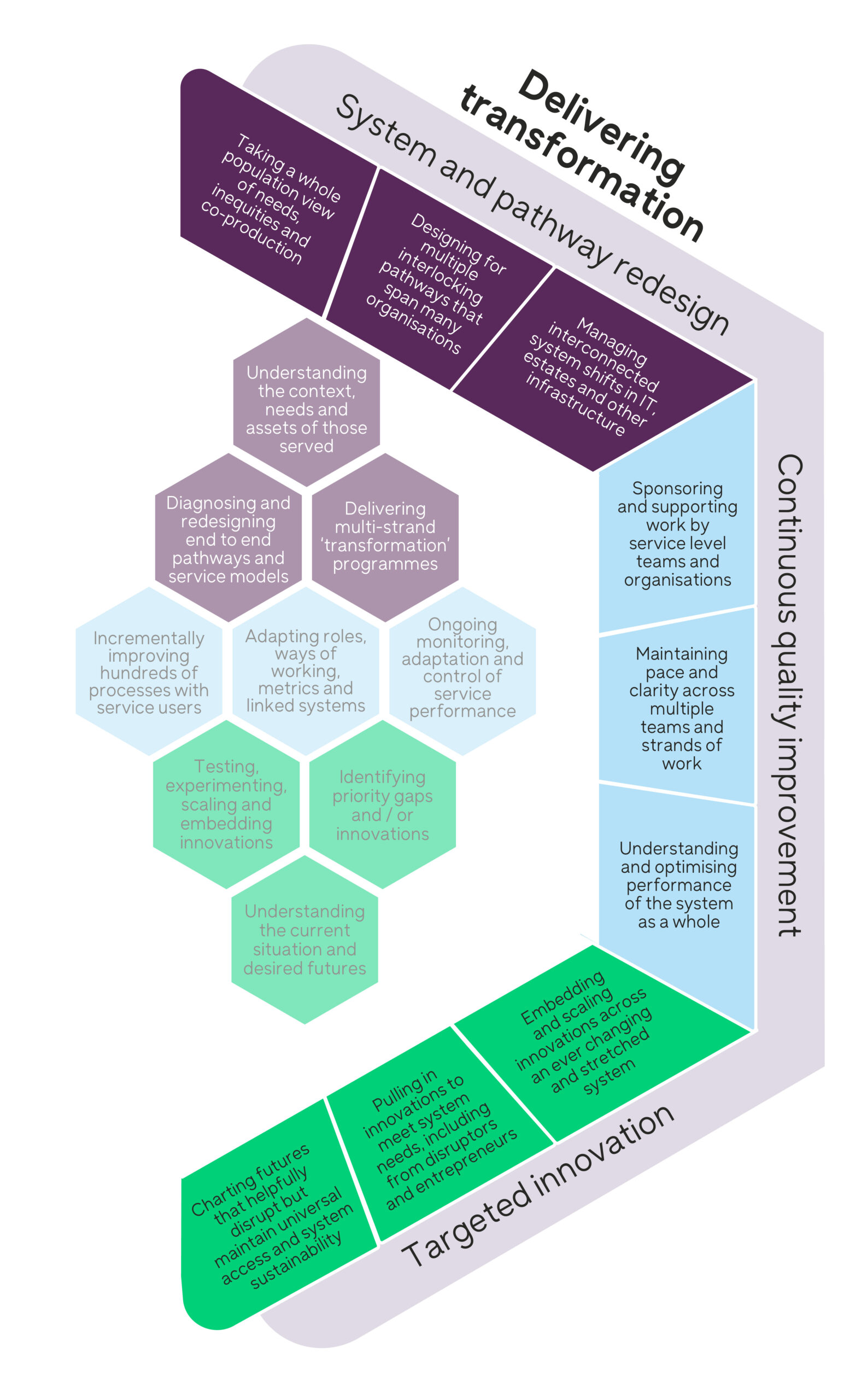
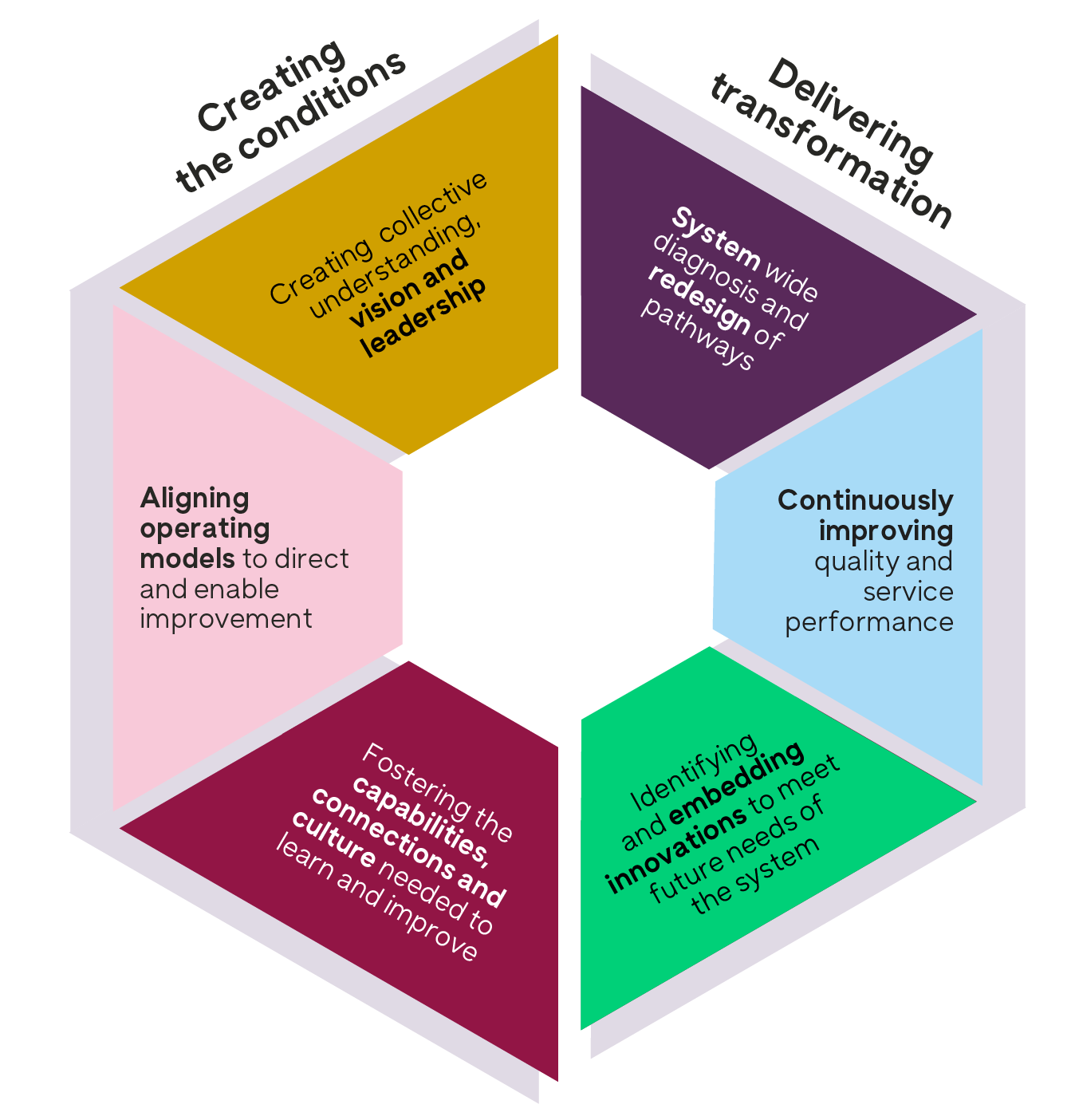
Based on the evidence and the experience of those leading large-scale change, the framework distills six modes of activity, in line with NHS IMPACT. There are three modes of action that help create the conditions for sustainable improvement and three modes that enable transformation of services and outcomes. The framework invites and supports users to consider how these modes of activity can best come together in their context for the greatest, sustainable, positive impact.
The outer segments of the framework show 18 key considerations that we know often accompany cross-system change work. This recognises that improvement work that spans places and systems is different and will often be led by multiple organisations. The framework provides a structure to work through the complexities associated with working together across boundaries to achieve the full potential of system working.
Testing the framework
To make sure the framework continues to best support those who use it, and accurately reflect the activities and considerations needed to deliver large scale system change, we will continue to improve and refine it. Based on feedback so far, we are also developing tools to help review and plan for the work required to deliver change at scale: either overall, in specific service areas, or for system goals.
We are looking for people leading improvement work at a system level to continue co-developing the framework with us. We want to test some workshop tools that introduce and apply the framework within an individual system. Through the workshops we will share materials that can be tailored to your needs, audiences and can support facilitation.
The framework also provides a structure for peer learning between systems. As part of our partnership between NHS Confederation, the Health Foundation and Q, we are inviting all systems in the UK to participate in a peer-learning programme, where we will be using the framework.
We are collating supporting examples to highlight best practice and will iterate and evaluate the framework as it is used in in practice.
Please contact us if you’re interested in exploring this framework within your system.
Navigating the framework
This section introduces the different activities that make up the framework.
6 modes of activity make up the overall hexagon:
- three modes of activity that help create the conditions for effective, sustainable improvement.
- three modes of activity that need to come together when delivering transformation.
Within each mode of activity there are:
- three to five hexagons summarising key activity areas within this mode. These activity areas apply at team, organisation and system level.
- three distinctive considerations often associated with doing these activities at a scale that spans multiple organisations in a system.
Creating the conditions
Overview
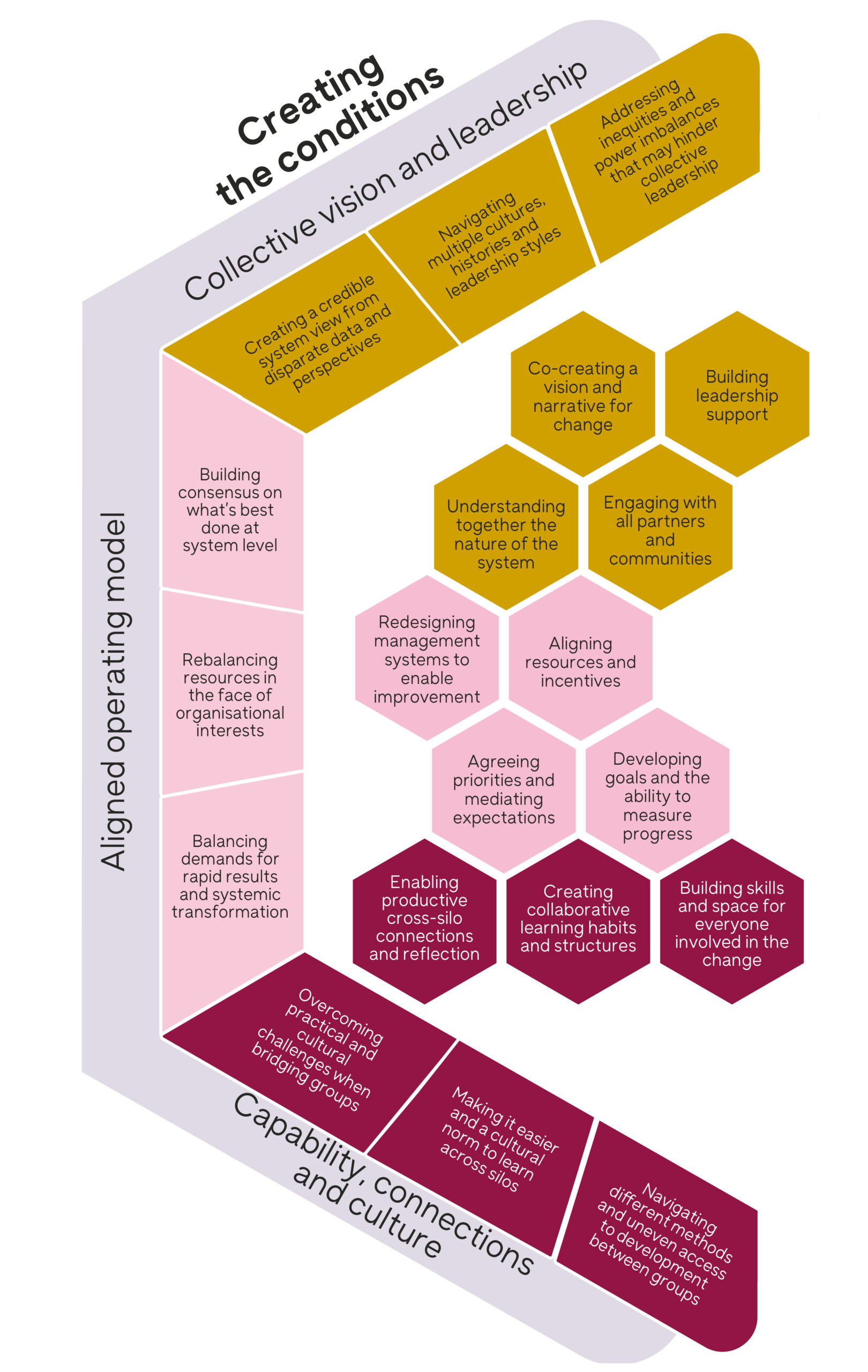
These three modes of activity describe what’s needed to create the conditions for effective change. In England, NHS IMPACT is explicitly focusing on work in this area, so you’ll see the five elements of the IMPACT approach reflected in this section. This draws on testing with leaders involved in designing NHS IMPACT.
The nature of improvement work focuses on building skills, vision and culture as you implement changes. We understand that focusing on the three overarching activities in this area are important to create the conditions for success.
Key activity areas
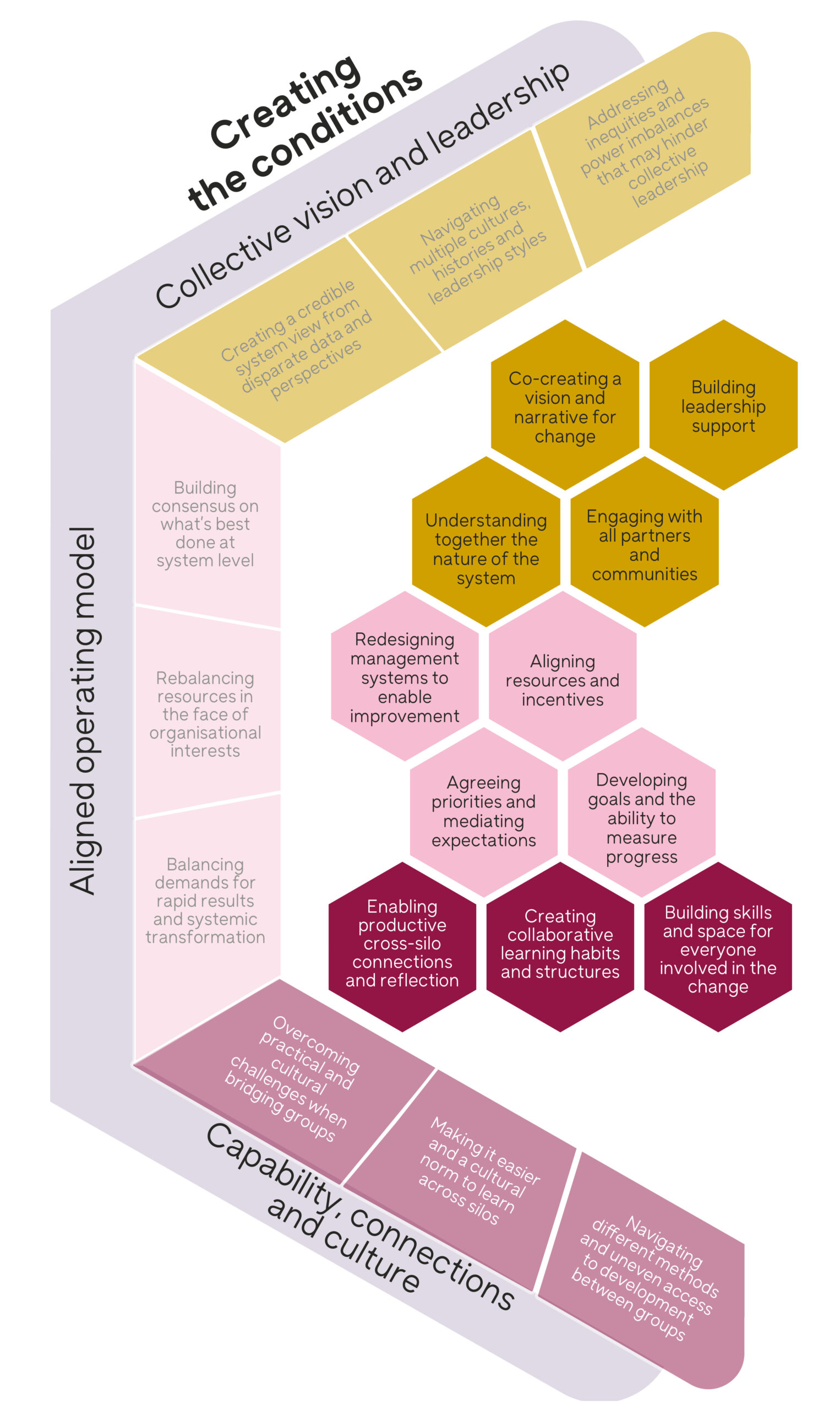
The inner hexagons summarise the main activities needed to create the conditions for sustainable improvement.
When we create a collective vision for a system or organisation, it relies on:
- engaging with partners and communities
- building a shared understanding of the system
- a narrative for change
- the leadership support needed to succeed.
We need to prioritise the effort required to change the intention to transform care, into delivery. It needs incentives and systems to integrate improvement as the mainstream operating model for organisations.
For us to sustain change, it relies on culture and on those working across the health and care sector having the capabilities, supporting space and processes to make progress.
Considerations when working across systems
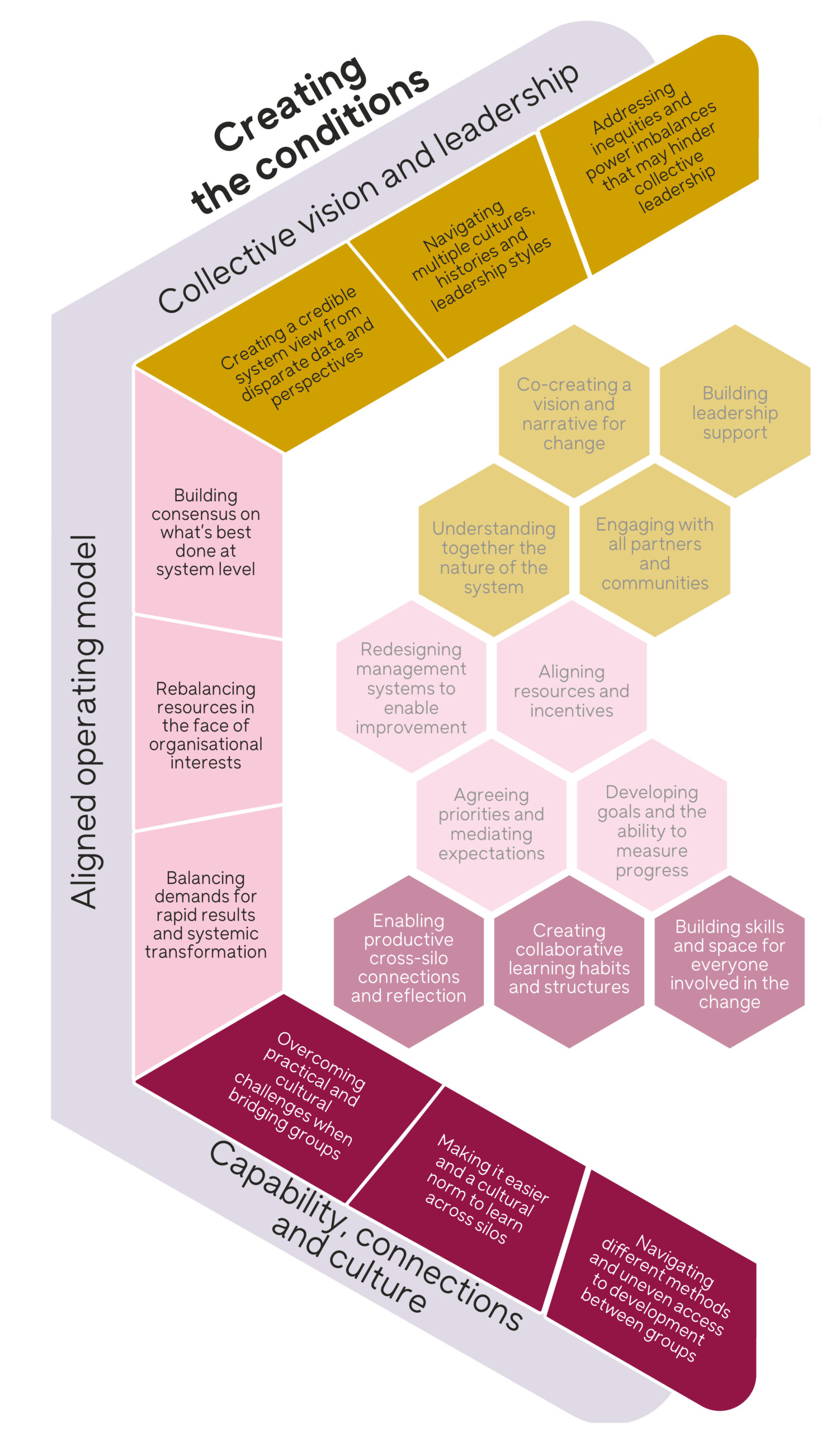
The outer boxes explore the distinct considerations we need to make when doing the activity described in the inner hexagons, at a system level. Being explicit about these considerations helps us to understand and define the leadership strategies needed to succeed. It also provides the opportunity for us to draw on tried and tested improvement approaches.
Seeing how the system is working as a whole can be hard. This is both because data is patchy, and because there are some complex power dynamics at play when we bring together organisations. This can create strategic tensions between organisations. Building and maintaining sufficient consensus and support for change at a system level requires us to employ different strategies, leadership behaviours, and practices. We need people with advanced collaboration skills to support planning and delivering change across organisational and professional boundaries.
Most health sector infrastructure is geared towards operationalising work through organisations. So this work can take longer because of the number of teams involved, each with their own processes and cultures. Making sure we prioritise the needs of the population and the overall system is hard when changes can compete with, or threaten, the interests of individual organisations.
Working in this way can also take longer to deliver benefits. The nature of the work may mean that other parts of the system benefit, rather than the parts involved in making changes. This is especially challenging in a sector where we can be short-term focused and where we rarely have the financial flexibility to support new services to be tested, alongside existing service delivery.
Working together across a system offers us opportunities for a wider range of expertise and experience to come together to address challenges. But competing terminology, and uneven access to learning about improvement can highlight existing divisions and tensions between organisations and professions. For us to realise this potential of cross-system working requires the time, skills, infrastructure, and culture to be able to collaborate well with each other.
Delivering Improvements
Overview
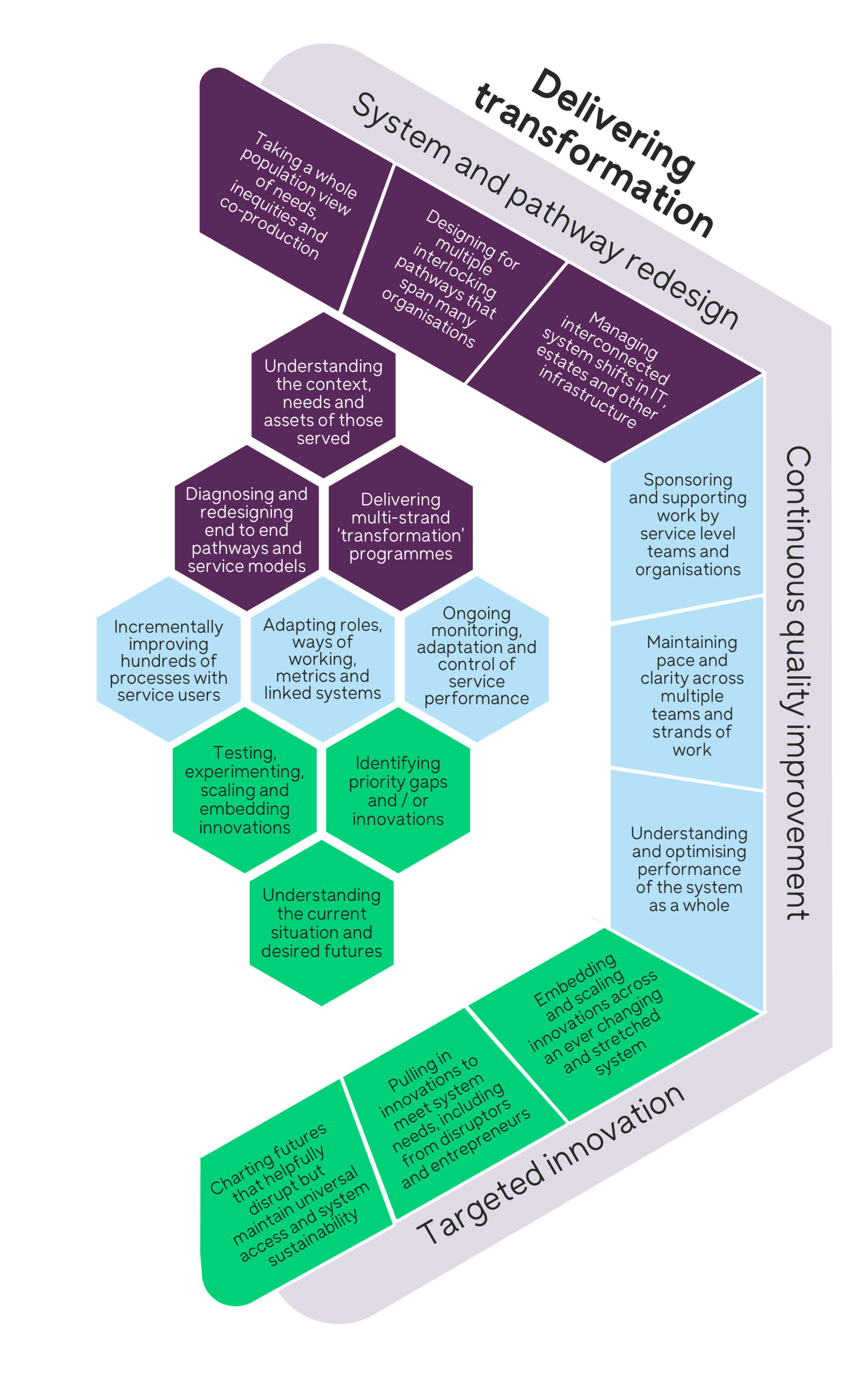
The right-hand side of the framework combines three modes of activity we need to deliver changes across the system, to improve outcomes and transform care.
We need macro-level‘ system redesign’ or ‘transformation’ work to shift overall pathways or models of care. This should work alongside continuous process improvement to address specific service-level quality challenges. Our framework highlights the importance of understanding the multiple methods needed to deliver transformation across these two levels.
A wide variety of innovations emerge through testing and scaling in a system. We could achieve more with these innovations if we take a purposeful approach to stimulate them.
Key activity areas
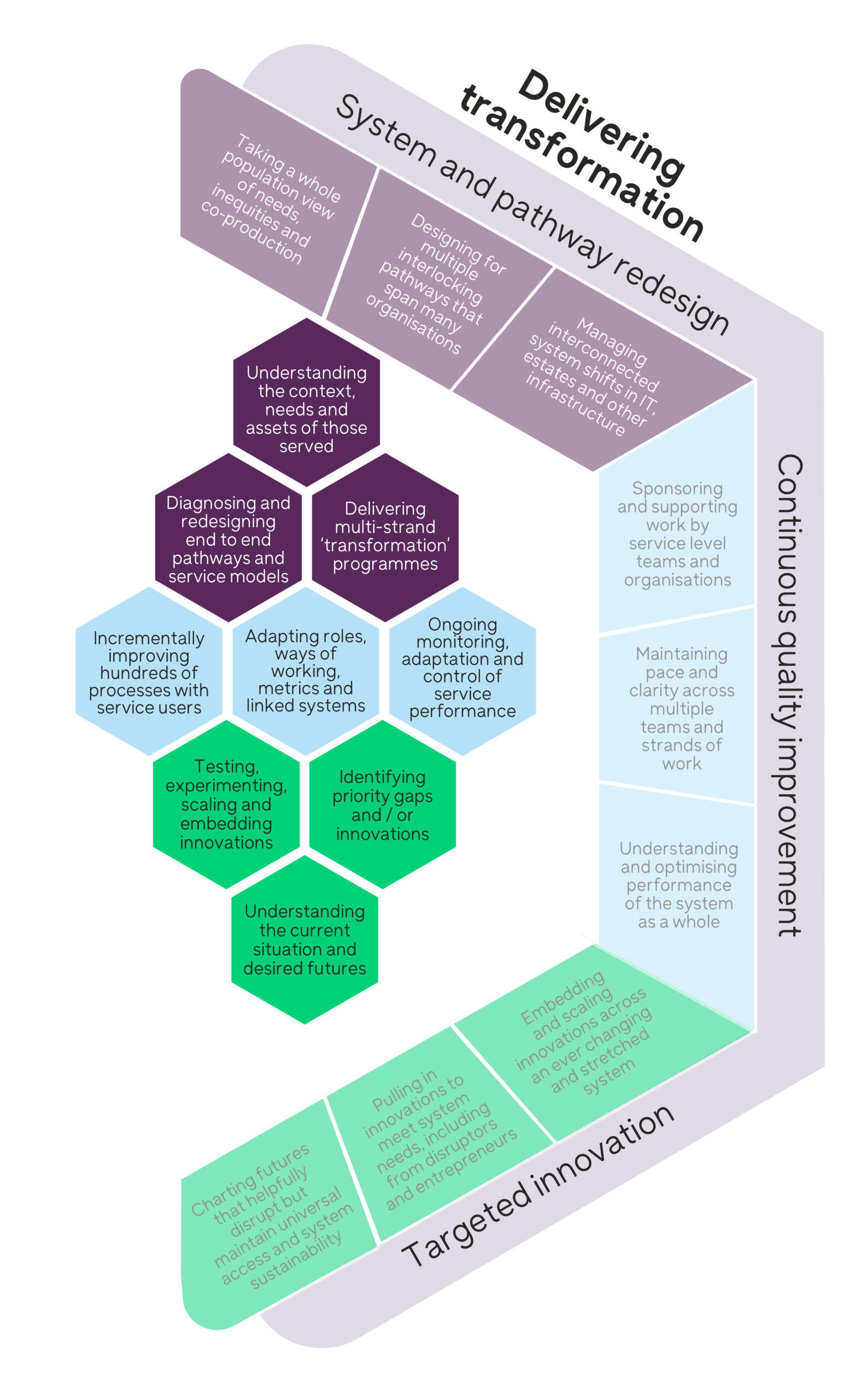
For us to successfully redesign pathways and systems, we need a deep understanding of the local context, population needs and the assets available to drive and embed change. This allows us to diagnose key challenges and provides the platform for carefully designed, co-produced change with those who use and deliver future services. We need to align this with other relevant transformation efforts.
Continuous improvement is built on many small-scale iterative tests of change with the right people. It’s supplemented with reliable, real-time data and measurement. We need to implement ongoing monitoring to refine and sustain service changes – making sure we’re adapting roles, ways of working, and systems to support interventions.
For targeted innovation, a significant role involves identifying promising innovations or delivery gaps and recognising these may come from a range of sources. When we build a long-term view of what needs to change, we need to balance this with experimentation and adapting and embedding improvement at scale.
Considerations when working across systems
The outer boxes acknowledge the considerations associated with delivering change across large systems. When we acknowledge the distinct approach to improvement needed across large-scale systems, and the number of elements that need to come together, we can plan and align our efforts to maximise the long-term positive impact.
Transforming end-to-end models of care is only possible through redesign at the level of health and care systems. We need to look beyond the service models and strategic priorities of individual organisations to deeply understand population needs and the inequities in the current model of provision. For us to implement long-term positive change, it’s likely to need multi-year programmes of activity that combine cross-pathway diagnosis and redesign, with changes to the funding, IT, and estate. It can be hard to maintain progress across these different areas of work that may have limited control at the system level.
Individual organisations should be iteratively diagnosing and improving their processes and systems. However, there will be processes spanning systems that may need sponsorship or support at system level.
We know that there are likely to be many individual innovations at various stages of development within a system. It can be hard to identify the innovations that will support a different paradigm or model of care, rather than optimising the current care model. Sometimes these innovations come from unfamiliar sources outside of the current system. We need to provide structured support to nurture innovation at system level and help people scale and embed ideas into new care models.
Improving care for communities across large-scale systems is complex and dynamic. We hope that building on what we know about how to enable and deliver improvement will help system leaders navigate and develop successful strategies for change.
To explore using the framework with your system, please contact us.
Simplified framework
A simplified version of this framework was published in the report by NHS Confederation Improving health and care at scale: learning from the experience of systems. You can download a version of the simplified framework below.
Acknowledgements
This framework has been developed through workshops and interviews with national, regional, and local leaders. It represents a collaboration between the five countries that partner to deliver Q. We would like to thank the following people for their input:
- John Ashcroft, Director for Pathways, NHS England
- Helen Bevan, Strategic Advisor, NHS Horizons
- Victoria Binks, Assistant Director – North West and Yorkshire, NHS Confederation
- John Boulton, National Director of NHS Quality Improvement and Patient Safety, Public Health Wales
- Ilse Bosch, Deputy Director of Policy, NHS Confederation
- Ailsa Brotherton, Director of Continuous Improvement and Transformation, Lancashire Teaching Hospitals NHS Foundation Trust
- Anna Burhouse, Director of Quality Improvement, Northumbria Healthcare NHS Foundation Trust
- John Drew, Director of Staff Experience and Engagement, NHS England
- Maria Lordan Dunphy, Assistant National Director Quality Improvement, Health Service Executive Ireland
- John Fitzsimmons, Clinical Director for QI, Health Service Executive
- Maureen Flynn, Director of Nursing, Health Service Executive
- Marie Gabriel, Chair, North East London Integrated Care System
- Ruth Glassborow, Director of Place and Wellbeing, Public Health Scotland
- Felicity Hamer, Strategy Lead, Improvement Cymru
- Diana Hekerem, Associate Director Transformational Redesign Support, Healthcare Improvement Scotland
- Raj Jain, Chair, NHS Cheshire and Merseyside
- Sasha Karakusevic, Associate, NHS Horizons
- Aideen Keaney, Director of Health and Social Care Quality Improvement, Health and Social Care Quality Improvement (HSCQI) Northern Ireland
- Annie Laverty, Chief People Officer, NHS Integrated Care Board for the North East and North Cumbria
- Joanne Matthews, Head of Improvement and Scottish Patient Safety Programme, Healthcare Improvement Scotland
- Matt Nelligan, Director of System Transformation, NHS England
- Belinda Robertson, Associate Director of Improvement, Healthcare Improvement Scotland
- Matthew Taylor, Chief Executive, NHS Confederation