I worked with the Q Improvement Lab (Q Lab) over the last 6 months on its first initiative to support the use of peer support services.
There is no formal definition of peer support, but through working on the topic, the Lab defined peer support as people with shared experiences, characteristics or circumstances supporting each other to improve health and well-being. Peers can be people with similar health conditions, or from similar communities or backgrounds.
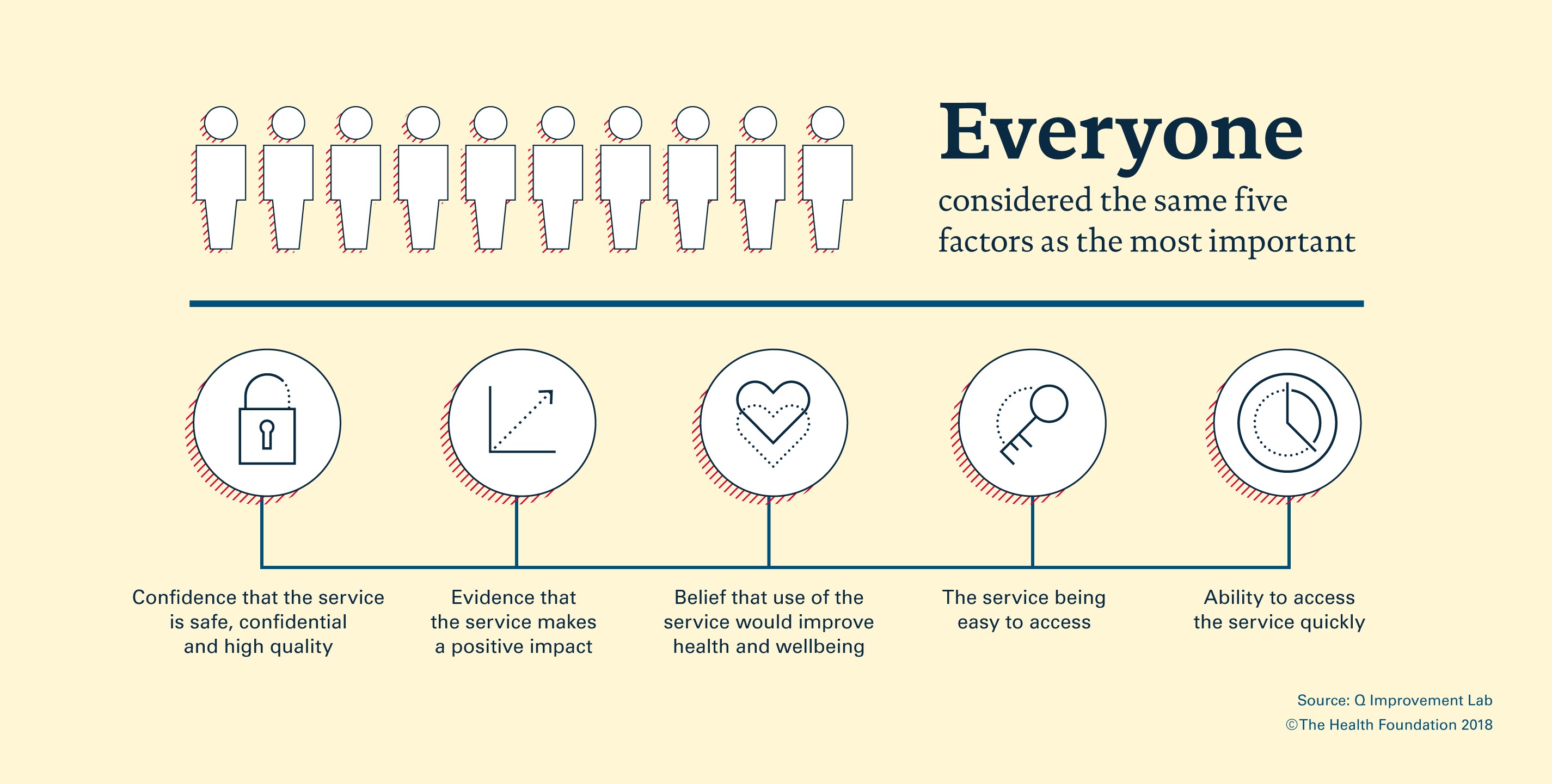
In particular, I analysed data from the largest peer support survey to date of over 2500 people about what is most important to them in choosing to either use, recommend or refer to peer support.
The full results are available in our online essay, but two aspects in particular caught my interest.
The role of personality
Members of the public said that confidence in the quality of the service, and belief that peer support would improve health and wellbeing, were the two most important factors in deciding to access support, regardless of whether they had actually accessed peer support.
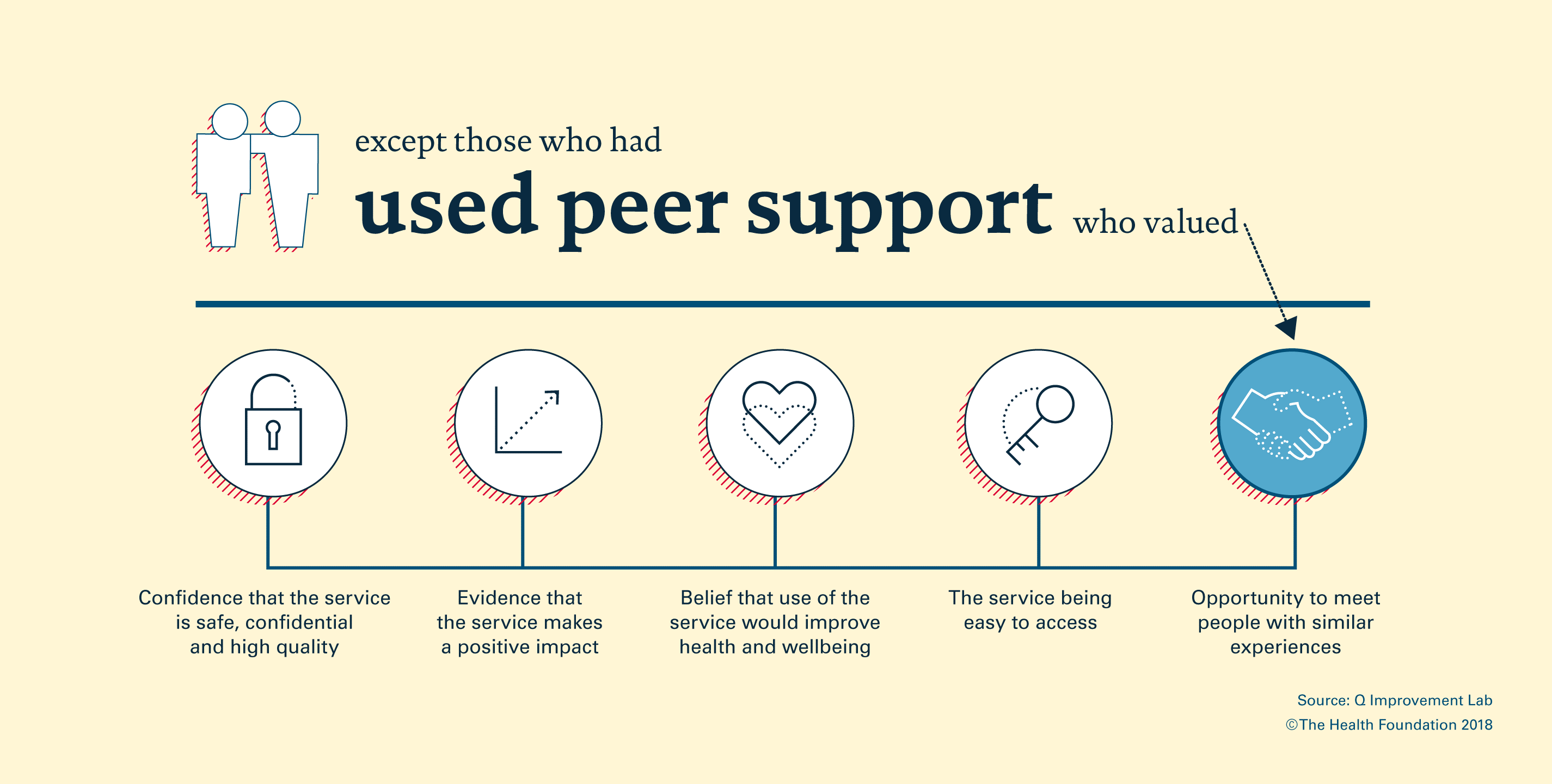
However, for members of the public who had not accessed peer support, the opportunity to meet people with similar experiences was ranked as much less important (9th out of 12), compared to members of the public who had accessed peer support (4th out of 12).
 What is driving this difference?
What is driving this difference?
Is it that it is only once you access peer support that you appreciate the benefit of meeting people with similar experiences? Or is that the people who access peer support are people who already value social connections and are looking for more opportunities to meet people? Understanding this matters – if it’s the former, the question becomes:
- How can we better promote the positive impact of meeting people with similar experiences?
and if it’s the latter, the questions are considerably more complex:
- Is peer support for everybody?
- Would online groups work better for people who are not looking for social interaction?
- Or is a different model of peer support entirely needed, such as regular support emails that do not involve real-time interaction or require a response?
- Is there a natural (relatively low) limit for the proportion of people who will want to access peer support?.
The role of professional endorsement
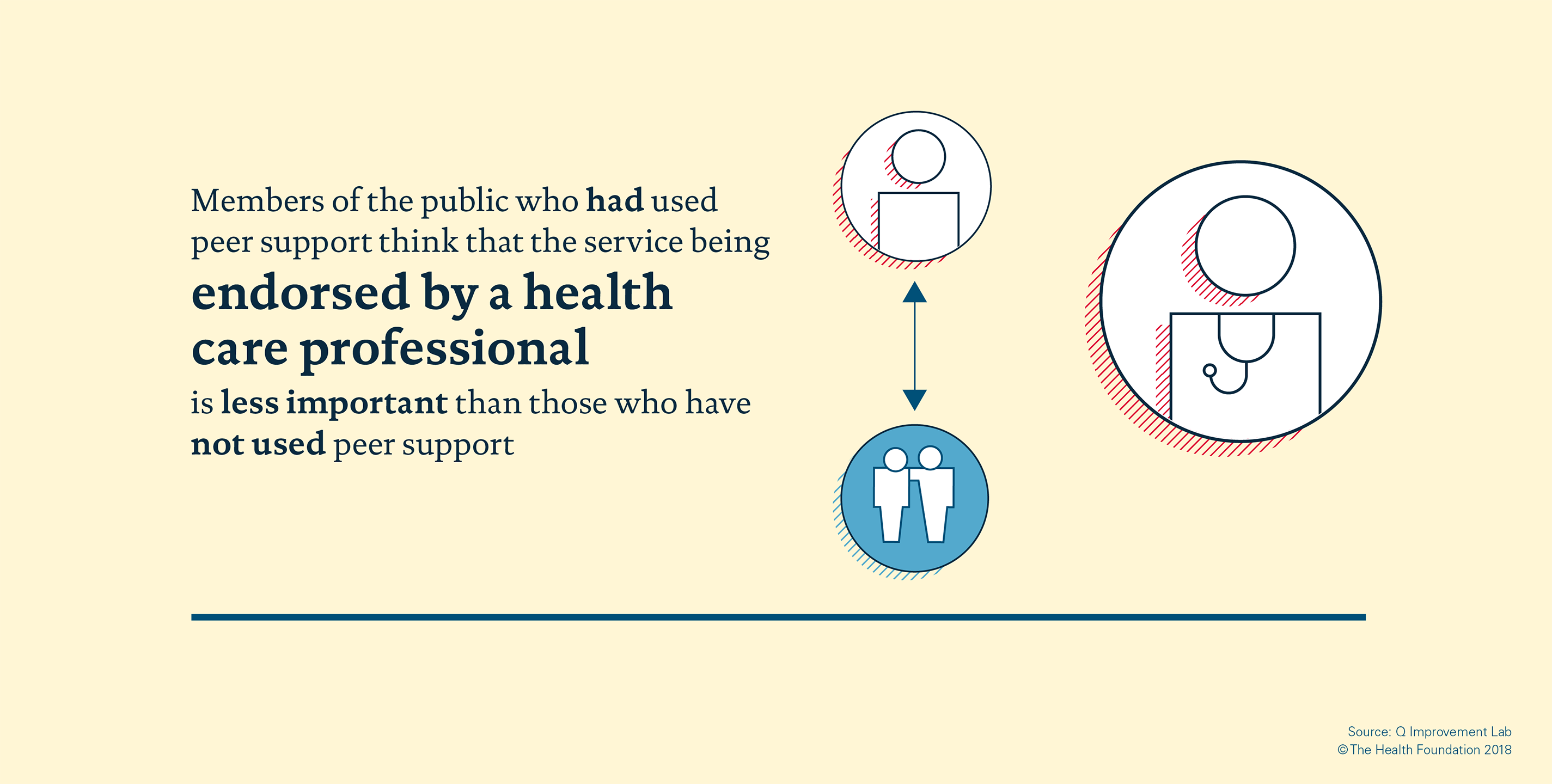
The only other major difference between members of the public who had and had not used peer support was in the role of professional endorsement.
A peer support service being endorsed by a healthcare professional was ranked 11th (out of 12) compared to 5th by those who had and had not accessed peer support respectively.
What is driving this difference?
- If those who have accessed peer support did so precisely because they were seeking personal connections, was professional endorsement irrelevant or unnecessary?
- For people diffident or unsure about peer support, do they need the explicit recommendation from their trusted health provider to take the plunge?
- Or is it that people who have not accessed peer support need professional endorsement to both have confidence that the service is good and to generate belief that it will help them (the top two priorities), whereas for those who have accessed peer support, it is the opportunity to meet people that leads them to believe peer support will help?
Key lessons
While this survey and analysis is focused on peer support services, it’d be interesting to see whether the learning from this survey can be applied to other health care services.
- Is more professional endorsement needed to support people to use more community health and wellbeing services?
- And despite the endorsement, what if the service just isn’t very you?
This piece of work was a great opportunity to delve deep in to why people choose to use or refer to peer support – analysis that other services might benefit from to increase access.
Perhaps the best way forward is for health care professionals, particularly GPs, to recommend peer support services (and other health care services) tailored to the personality and preferences of each individual patient. However, this does require continuity of GP care – beneficial in so many other ways – but hard to guarantee in the current NHS environment.
Q members, it would be great to hear your thoughts – reach out to me through the Q member directory or contact the Lab team at qlabs@health.org.uk.