Q Exchange
The Missing Piece of the CKD puzzle
- Idea
- 2018
Meet the team: #teamrenal
Also:
- Tamasin Stevenson Access Sister
- Annette Dodds Renal Matron
Background
In 2015 the number of adult patients starting dialysis in the UK was 7814. Of these the overall rate of late presentation (defined as any patient first seen by renal services within 90 days of starting dialysis) in the UK was 17% with variation between centres from 5% to 35% in patients starting dialysis in 2014 to 2015.
Data collected by the UK Renal Registry, shows these differences have implications for referral pathways with large differences in the percentages starting on Peritoneal Dialysis (PD) and in haemoglobin and eGFR at start with all three of these being lower in late presenters than early presenters.
The NHS Right Care Scenario on Progressive Chronic Kidney Disease also highlights potential improvement opportunities through a fictitious but representative patients story and outlines the dramatic impact the optimal CKD pathway can have on the patient and family life.
The Health Foundation is currently funding a quality improvement initiative “Assist CKD”, utilising a computer programme to flag people with declining kidney function to ensure GPs are aware of the decline and have considered referral to a Nephrologist.
However, the challenge remains with those patients who are completely unknown to the system or those with rapidly progressive CKD, to ensure they have access to a pathway that enables a choice of all appropriate forms of Renal Replacement Therapy.
Local experience
At HGS at UHB in 2017, 148 patients commenced chronic dialysis and of these 35 presented late (24%). Local audit data shows that 19% of the late presenter patients receive home dialysis at 90 days after presentation compared to 60% of the early presenters.
Your Proposal
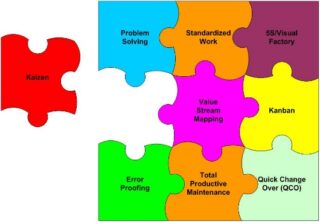
The renal team at HGS at UHB has established a culture of continuous quality improvement and since 2014 has grown the home dialysis population from 8 to 19% of the prevalent dialysis population.
This proposal aims to address the missing piece of the puzzle through challenging current beliefs on how patients requiring RRT, who are late presenters, are managed, through a detailed understanding of the patient pathway Through influencing the thinking and system as well as current performance.
To improve care for late presenters through developing a toolkit of resources to ensure equity of access to all appropriate modalities of Renal Replacement Therapy for patients regardless of when they present.
- Analysis to understand the current pathway for the individual patients within this group – process mapping using simple questions to understand each step in their pathway ;what, where, when, who, how, why
- Staff and patient focus groups
- Testing a range of potential solutions
- Co-production of a good practice toolkit with patients and carers
To share the toolkit as an example of good practice, adaptable for implementation by renal units, regionally and nationally.
What is the benefit you hope to achieve?
- For all patients with end stage kidney disease that require renal replacement therapy to have access to all appropriate modalities of renal replacement therapy regardless of time of presentation.
- To include listing for transplantation and access to home therapies.
- Through enabling shared decision making for all patients regardless of whether or not they are a late presenter as recommended in national guidelines.
- To improve patient experience of shared decision making, currently marked lowest by patients in the PREMs survey by the UKRR in conjunction with Kidney Care UK.
What benefits do you expect for the Q Community?
The toolkit will be made available to all Renal units nationally; it will be designed to enable any unit to adapt it, to meet their local situation and need.
This project builds on previous improvement work eg Enable – CKD (Enhancing Care and Saving Lives of People with CKD), and will link with other projects taking place nationally, including the Kidney Quality Improvement Partnership (KQuIP) to develop, support and share improvement in kidney services to improve people’s health and add value
How you can contribute
- Critique proposal
- Lend expertise in methodology
- Allow for fine tuning of dissemination ideas
Comments
Nicola Thomas 15 Jun 2018
Sounds great. Wonder what sorts of things will be in the toolkit? I understand that the toolkit will be co-produced so you will not know the answer yet, but an outline of possible resources would strengthen your proposal I think.
Oliver Watson 22 May 2018
Sounds good - our Chronic Kidney Disease Health Integration Team for Bristol, North Somerset and South Glos. will be interested to hear more!
www.bristolhealthpartners.org.uk/health-integration-teams/chronic-kidney-disease-hit/
Comments are now closed for this post.