Q Exchange
Improving recognition and care for children at the risk of deterioration and sepsis: A national community of practice approach
- Shortlisted idea
- 2018
Meet the team: Sepsis in Children #SepsisInChildren
Also:
- Equally important contributors are:
- Rahail Ahmed - Paediatric Emergency Doctor - Barts Health
- Enitan Carrol - Professor for Clinical Infection, Microbiology and Immunology - University of Liverpool/ Alder Hey Children's NHS Foundation Trust
- Akash Deep - Consultant Paediatrician and Paediatric Intensivist - King's College Hospital
- Sarah Eisen - Consultant Paediatrician - University College London Hospitals UCLH
- Tim Fooks - General Paractitioner - Pulborough West Sussex
- David Inwald - Paediatric Emergency and Intensive Care Consultant - Imperial College Healthcare
- Nelly Ninis - Paediatric Consultant - Imperial College Healthcare
- Joseph Piper - Paediatric St3 - Barts Health
- Alexandra Pledge - Paediatric Consultant - Barts Health
- Helen Rutkowska - Consultant Paediatrician - University Hospital Southampton
- Shye Wong - Consultant Paediatrician - Royal Free London
Sepsis in sick children is often difficult to recognise1. The consequences can be devastating to the children and their families and of course those providing the care2. Therefore, the more people are involved in addressing challenges associated with deterioration and sepsis in children and driving improvements the better.
Background
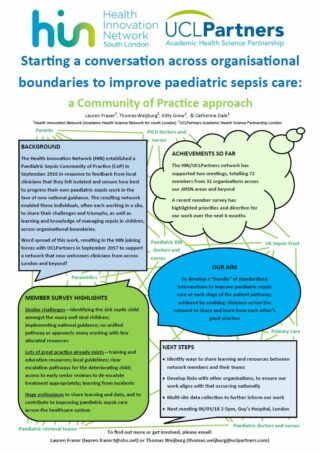
UCLPartners Academic Health Science Partnership and Health Innovation Network South London have been running a joint community of practice for paediatric sepsis since September 2017. So far more than 100 individuals from across the three London academic health sciences networks (AHSNs) and patient safety collaboratives representing more than 30 hospital trusts and other healthcare providers came together to explore challenges and solutions to improving paediatric sepsis.
The interdisciplinary community consisting of doctors and nurses of different grades, researchers and other allied healthcare professionals with an interest in paediatric sepsis, continuously identified multiple key challenges, which include:
– Variation of paediatric sepsis screening tools
– Sensitivity of paediatric sepsis screening tools
– Variation of paediatric early warning scores
– Variation in patient safety netting and parental advice
– The differentiation between those children unwell with a virus and those developing sepsis at an early stage
– The need for a national dialogue to improve sepsis and deterioration care in sepsis
One of the outcomes from the pan-London community to date – next to sharing learnings and inspiring improvements for paediatric sepsis education, safety netting, screening and care escalation and de-escalation – was the idea to bring together paediatric and paediatric emergency experts from across England, who have been driving paediatric sepsis and deterioration improvements in their regions.
Aim and ambitions
The aim is to accelerate and share learnings across England and beyond to eventually work together with national stakeholders to address the gaps in paediatric sepsis and deteriorating care. The understanding is that a national “Improving recognition and care for children at the risk of deterioration and sepsis” community of practice or network, would help to accelerate learning and develop the momentum to:
– Learn from others and adopt improvements to improve care locally
– Share learnings, improvements and innovations to allow others to learn from these
– Bring together experts from nursing, medicine, research and policy to together shape and inform improvements that may have a regional and national impact
– Share and spread learnings and improvements through talks, posters and publications.
The community will act as pool of peers and patient representatives to discuss local, regional and national challenges related to paediatric sepsis and deterioration. It will provide a springboard for interdisciplinary collaboration to identify strategies and approaches to drive improvements and spread learnings within care providers, across regions and health systems.
Activities
In order to achieve this, we propose to hold a series of four quarterly community of practice meetings distributed across England over the period of a year with a capacity of 60-80 attendees each. The learnings and outcomes from each meeting would be shared via one webinar following the event, which will help spread the learnings and stimulate debates beyond the community itself.
Furthermore, the development of conference posters would be encouraged and supported as well as a final programme publication that summarises and discusses the development and achievements of the paediatric sepsis and deterioration community. The community would also be brought alive with a series of brief video interviews of participants sharing their story, motivation and ambition about improving care for children at the risk of sepsis and deterioration. Webinars and videos would also be shared through the Q community platform.
Multiple participants of the pan-London Paediatric Sepsis: Improving Recognition and Care were directly involved in the creation of public resources such as educational sepsis videos produced by the Health Innovation Network South London and ASK Sniff, as well as Health Education England. The community would further build on these and help raise the awareness of and the ability to spot sick children at the risk of sepsis and deterioration among the public and clinicians, whilst identifying and addressing areas with scope for improvement.
A shared platform would be set up to record and report changes, learnings and improvements that were inspired by the community. These may range from improvement projects to parent and patient involvement, policy changes, educational programmes, pathway redesign, care bundles, audits, and other local, regional activities and national activities.
References:
(1) Adrienne G Randolph & Russell J McCulloh (2013) Pediatric sepsis: Important considerations for diagnosing and managing severe infections in infants, children, and adolescents. Virulence Volume 5, 2014 – Issue 1, pp 179-189
(2) Scott L. Weiss et al (2015) Global Epidemiology of Pediatric Severe Sepsis: The Sepsis Prevalence, Outcomes, and Therapies Study. Am J Respir Crit Care Med Vol 191, Iss 10, pp 1147–1157
How you can contribute
- Expertise in deterioration and sepsis in children
- Patient and parent involvement
- Hosting events
- Facilitation of events
- Networking
- Cross-system leadership
Further information
UCLPartners_HIN_Paediatric_Sepsis_Poster_UKSepsisTrust_2018 (PDF, 770KB)
Reviewer feedback
This is a great project because…
This project looks has the potential to use the UK scale of Q to help expand progress made within London. Nice opportunity to link with other work underway in paediatrics and sepsis.
By the time of the event we encourage the project team to think more about…
How this could link with the Q infrastructure and offer learning for others within Q not working on this particular issue. We know networks take careful design to really thrive, so worth thinking how this can work best if expanded across the UK.
Comments
Clare Smith 19 May 2022
Hello team, just in addition to my comment yesterday, I have shared your project with our children's outreach, assessment and support team (a group of community children's nurses who work in collaboration with primary care and acute care to support families of children with urgent, short term health needs). They are really interested in your project and would be very keen to get involved if at all possible. Please do get in touch with me if this would be of interest to you.
Clare Smith 18 May 2022
This would be really valuable for our community outreach nursing team working with our acute partners, so I'd be really interested in finding out more about your project as it develops.
Matthew Inada-kim 9 Nov 2018
Thomas
going forwards, deriving an outcome metric will be crucial.
Do email me, as I have some ideas that might enable some future capture of paediatric infection mortality using the SOS dashboard from ICHP.
Matt
Nichola Crust 9 Nov 2018
Dear Thomas,
Would it be possible for me to arrange a conversation with you? I work for the Healthcare Safety Investigation Branch. My contact number is 07753417453
Many thanks
Nikki
Thomas Weijburg 18 Sep 2018
Trying again without all the gibberish:
This is a great point. Getting primary and community care involved would be fantastic. I can absolutely see this being part of the programme and it would be great to have a conversation about how to work on this together. This is something that would also be very interesting for the community in London. I hope to meet you tomorrow where we can then talk about this a little more. Also, Damian Roland may have some thoughts regarding early identification sepsis or risk of sepsis in children in the community.
Kamal Patel 8 Aug 2018
The breadth of collaboration is impressive & I'm particularly interested in where the outputs of ASK Sniff have got to, which sounds a really exciting project.
How much does the success of this depend on being able to impact on staff working more collaboratively across the current primary/secondary care boundaries?
Thomas Weijburg 18 Sep 2018
Normal
0
false
false
false
EN-GB
X-NONE
X-NONE
/* Style Definitions */
table.MsoNormalTable
{mso-style-name:"Table Normal";
mso-tstyle-rowband-size:0;
mso-tstyle-colband-size:0;
mso-style-noshow:yes;
mso-style-priority:99;
mso-style-parent:"";
mso-padding-alt:0cm 5.4pt 0cm 5.4pt;
mso-para-margin-top:0cm;
mso-para-margin-right:0cm;
mso-para-margin-bottom:8.0pt;
mso-para-margin-left:0cm;
line-height:107%;
mso-pagination:widow-orphan;
font-size:11.0pt;
font-family:"Calibri",sans-serif;
mso-ascii-font-family:Calibri;
mso-ascii-theme-font:minor-latin;
mso-hansi-font-family:Calibri;
mso-hansi-theme-font:minor-latin;
mso-bidi-font-family:"Times New Roman";
mso-bidi-theme-font:minor-bidi;
mso-fareast-language:EN-US;}
This is a great point. Getting primary and community care involved would be fantastic. I can absolutely see this being part of the programme and it would be great to have a conversation about how to work on this together. This is something that would also be very interesting for the community in London. I hope to meet you tomorrow where we can then talk about this a little more. Also, Damian Roland may have some thoughts regarding early identification sepsis or risk of sepsis in children in the community.
Anne Maloney 17 Sep 2018
Very late comment, sorry. It would be very helpful to have a validated tool for identifying early sepsis or risk of sepsis in children in the community. I am leading a study in the management of emergencies and deteriorating patients in General Practice using in situ simulation in the Thames Valley. We will be doing hands-on training in the use of national early warning scores within this program and we could add a paed scoring system to this training.
Thomas Weijburg 5 Sep 2018
Dear Kamal, Thank you very much for your encouraging response. The success of the collaborative depends really on the input and support from the paediatrics communities across England. Increasing the input from primary care and and bridinging the gap between primary and secondary care effectively would defeintely add value to this network.
If you feel you (and anyone else) are able to help bridging the primary and secondary care gap, we'd love to hear from you.
Jo Murray 20 Jul 2018
Well done for getting shortlisted. Will continue to share information from our project that is on the reserve list!
Thomas Weijburg 5 Sep 2018
Hi Jo,
Thank you - yes, that's fantatsic news. You must have been disappointed and I hope you'll get a chance to proceed.
Thomas Weijburg 20 Jun 2018
Thank you for everyones support and comments in setting up and developing this project! Your thoughs and feedback provided through Q, Twitter, email and conversations have been hugely helpful and inspiring. Excited to see where this will take us :-)
Matthew Mezey 20 Jun 2018
Hi Thomas - if you (or others) plan to join this Communities of Practice call, make sure you register before, to get the login details you'll need.
Matthew Mezey 19 Jun 2018
If you’re interested in NHS Communities of Practice (CoPs), please join Q’s CoPs special interest group’s Zoom call on 13 July (1pm) to hear about the evaluation of the Health Innovation Network’s CoPs – their challenges and their journey.
** More info/to register: https://q.health.org.uk/event/the-sustainability-and-impact-of-nhs-communities-of-practice-lessons-from-a-rand-europe-evaluation/ **
The call will be an opportunity to glean advice and insights to help this project too.
Thomas Weijburg 20 Jun 2018
Hi Matthew - thank you for bringing this to our attention! This will be very interesting.
Hein leRoux 10 Jun 2018
Anything that can be done to better identify and prioritise the deteriorating child would, as you say, be welcomed by everyone. At the West of England AHSN we have done a lot of work on sepsis and NEWS in adults and I think if you could do something similar for children then that would be fantastic. I know it is complex, but will be worth the effort.
Thomas Weijburg 11 Jun 2018
Hello Hein, achieving this outcome would be fantastic. We are learning more from day to day and it seems views on how to reliably identify deterioration in children vary across the board. If there is anything you can share or contribute, you'd be more than welcome to.
Thomas Weijburg 5 Jun 2018
We would love to hear your thoughts about our apporach! Any ideas to deliver this more effectively are very welcome.
NIcola Davey 5 Jun 2018
Great to see so much collaboration - looking forward to seeing this come to fruition - would love to contribute too.
Thomas Weijburg 5 Jun 2018
Hi Nicola, thank you! Your comments are very much appreciated. Fingers crossed! Why not mark yourself as a supporter?
Matthew Inada-kim 26 May 2018
This is an absolute must do. I am really excited to see this collaborative forming, and can't wait to start seeing some of the outputs. Very well done to all concerned- what a team!
Thomas Weijburg 29 May 2018
Thank you, Matt! This means a lot to us. There is so much to learn from other regions and so much to achieve when all of us pull together
Jo Murray 21 May 2018
Hi All. Great idea to collaborate on this topic. Acute trusts across Wessex and Oxford PSCs/AHSNs have adopted the attached Paediatric Sepsis Pathway, developed by Thames Valley and Wessex Paediatric Critical Care Operational Delivery Network, with screening and paediatric sepsis six criteria https://www.patientsafetyoxford.org/wp-content/uploads/2017/02/TVW-Paediatric-sepsis-screening-tool-Aug-2016-with-FiSH.pdf
Thomas Weijburg 29 May 2018
Hi Jo, maybe we can have a chat some time soon. Interested to hear your point of view
Thomas Weijburg 21 May 2018
Thank you, Jo. I know a number of trusts that are looking at this approach. Interesting times ahead :-)
Comments are now closed for this post.