Q Exchange
Improving patient experience, communication and care through digital technology – RITA
- Winning idea
- 2022

Meet the team
Also:
- Alison Thayne - Dementia Lead
- Joana Dias - Senior Sister
- Helen Hall - Research & Evaluation Service
- TBC patient representative
What is the challenge your project is going to address and how does it connect to the theme?
Barriers to communication can be linked to a wide variety of factors including: Learning difficulties, Memory impairments, Mental Health issues, Stroke, Intubation and Language barriers and can be distressing for service users and staff alike.
Our project will pilot the introduction of RITA (Reminiscence Interactive Therapy Activities) for inpatients living with dementia. Patients with dementia are at higher risk of falls and pressure ulcers. Hospital admission can trigger distress, confusion and delirium. Contributing to a decline in functioning and a reduced ability to return home to independent living. During hospitalisation patients with dementia fall more frequently than patients without dementia (12 % versus 3 %). Reduced communication could mean the patient may be less able to tell someone that they are in pain or want to move, which can impact pressure ulcers, agitation or restlessness. All of which can have a direct effect on quality and length of the patient’s stay.
What does your project aim to achieve?
Objective
To integrate and evaluate the use of RITA in an identified ward with patients who have dementia and other complex needs.
Anticipated Outcomes
(Quantitative routine data)
- Improved pain control, behavioural scores, nutrition and hydration.
- Fewer pressure sores and falls.
- Leading to overall reduction in length of stay and delayed transfers of care.
(Qualitative data from patients, family and staff.)
- Improved patient experience, engagement – better anticipated patient’s needs.
How will the RITA tool achieve this?
- Greater communication and relationship with health care staff through interaction with RITA.
- Less time in bed during the day through group interactions with the tool. Sleep awake cycles become more regulated.
- Less agitated and more stimulated throughout the day.
- Increased interaction with staff and other patients
How will the project be delivered?
Intervention implementation:
Exploration: A recent service evaluation has identified area requiring improvement. Implementation barriers and facilitators are currently being identified through stakeholder engagement and a capacity to implement assessment has been undertaken. Fidelity and outcome benchmarks are being identified.
Installation: Resources identified, organisation time planned, local governance requirements and training requirements reviewed.
Implementation: Initiate improvement cycles, monitor and manage implementation drivers, achieve fidelity and outcome benchmarks, further improve fidelity and outcomes.
Measuring Impact
Mixed methods evaluation of the intervention and cost benefit analysis will be carried out alongside the implementation to understand patient and staff experiences and acceptability of the intervention and report outcomes such as falls, length of stay and other safety reports compared with baseline data.
A risk assessment will be undertaken to document potential undesired impact of the introduction of the technology.
How is your project going to share learning?
Project outcomes and learning will be shared within the Trust via Leadership Forum, Patient Experience Committee and displayed on the Trust’s Quality Improvement page (and potentially the ICS QI page, once it is set up).
They will also be shared through the Q community, professional networks, conferences and on social media (we will explore journal publication)
How you can contribute
- General sense check
- What areas do we need to develop more
- Suggested Links / networking
Plan timeline
| 1 Jan 2022 | Pre change - Data collection |
|---|---|
| 1 Feb 2022 | Enhanced Supervision and Engagement Service Evaluation |
| 18 May 2022 | Engagement and Identification of Stakeholders. |
| 14 Jun 2022 | Commence training of patient facing staff |
| 14 Jun 2022 | Connect with other project teams utilising the same technology |
| 27 Jun 2022 | Commence implementation of new devices |
| 1 Jul 2022 | Service user and staff evaluation of new devices |
| 7 Jul 2022 | Monitoring progress and sharing learning |
| 18 Jul 2022 | Commence post implementation audits |
| 9 Jan 2023 | Review impact of introducing change idea |
| 10 Jan 2023 | Update and start implementing spread plan |
Project updates
27 Jun 2023
Next Steps and Project promotion
As an organisation, it has been recognised that the use of RITA for all patients within the trust has had positive outcomes and experiences for patients. Our safeguarding team will continue to champion RITA utilisation to further facilitate person-centred care. Fund raising is underway for additional devices to better facilitate trust wide patient-staff engagement. Additional enhanced supervision training to be provided for staff, focusing on providing person-centered care, utilising RITA.
Our Dementia lead took RITA to a Place Safeguarding Conference to promote its benefits, as part of the available tools to support patient care.
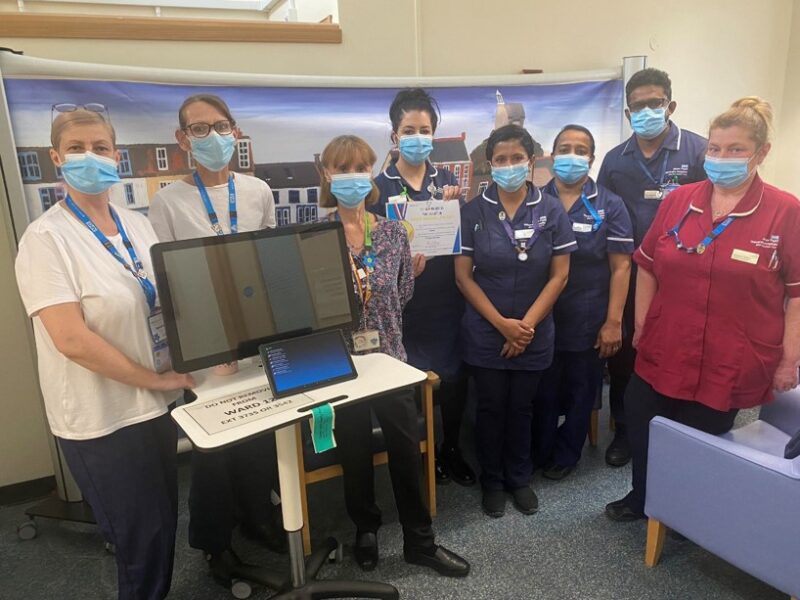
The RITA project team was awarded a Gold Medal as part of the NHSE&I Reconditioning the Nation Programme for contributions to preventing deconditioning and improving patient experience.
A poster has been created for an upcoming UEA Health and Social Care Partners conference, “Collaborate to Innovate: Enabling Citizen-Centred Care” in July 2023.
A journal article is being drafted for publication evaluating the impact and implementation of the RITA devices.
Special thanks to the Health Institute Q Exchange programme for enabling this project to be undertaken.
27 Jun 2023
RITA & a Safeguarding Practitioner (Feb 23- present day)
Following on from our last report it became evident that due to the busy nature of the wards, the devices would require more hands on implementation support.
A Safeguarding Practitioner was recruited (external to original project plan), as part of her role was promoting Positive Behaviour Management and has championed RITA use, Trust wide, including with patients who have post-operative delirium, on detox or have mental health diagnoses. Devices are again being utilised well.
Data collection challenges:
Collecting and analysing meaningful quantitative data proved problematic:
- The Level of Enhanced Supervision data was unreliable as it was reliant on staff manually updating data capture forms, which was complicated by the levels fluctuating during the patients stay.
- Patients being moved from ward to ward skewed our assessment of the impact of the device, once the patient moved they no longer had access to RITA.
- There were small numbers of falls for the patients who met project scope, meaning the results were not statistically significant
- Covid impacted Length of Stay, this was compounded by a national predicament the Adult Social Care and Community Health and Care was facing, with bed shortages causing patients to spend longer in acute care.
Ultimately due to the unreliable nature of the other quantitative data, we concede to focus only on the qualitative evaluation of the introduction of RITA.
Data and Discussion
The data from the surveys, semi-structured interviews, field notes and activity logs were thematically analysed using Braun and Clarks 6 step analysis revealing four themes:
person-centred care
facilitated meaningful activities
improving staff morale
other benefits to patients (including improved nutrition and hydration)
These themes resonates with those in the literature regarding dementia and reminiscence therapy. From the qualitative feedback the positive impacts of RITA were very evident and largely linked to the presence of the RITA champions, who were actively promoting and utilising RITA devices to stimulate conversations, games and sing-a-longs. The champions described how utilising the device as a channel to open discussion and instigate conversation. The ring fenced time provided staff to have “actual conversations” with someone, actively listening, not just part of providing personal care or medication. Facilitators or champions not only guide the patients while using activities, but also support and manage the patients, should there be distressing memories. Staff utilising RITA reported uplifting their own mental wellbeing, through being able to calm patients who had been agitated and on enhanced supervision before. Evidence says that personalised reminiscence focuses on the patient with dementia as an individual and is more likely to enhance their wellbeing. With person-centred engagement and meaningful facilitation the ward took on a different feel. A visiting consultant couldn’t believe the atmosphere on the ward when the champions were there: Patients singing and clapping along to Elvis, patients saying that having the visit from the RITA champion “made their day”.
It was evident that RITA could only have a meaningful impact if it is being utilised as the initial focal point to stimulate reminiscence, which will then lead to conversations and the improved patient experience. However, this is directly linked to the staff members having the dedicated time to provide this person-centred care.
11 Jan 2023
Project Update Summary:
The project implementation commenced at the end of September 2022. Four Health Care Assistants (HCA’s) were identified as RITA Champions to support the roll out of the RITA project on the wards. The plan was for the champions to be in place for the first 3 months of the roll out. Their daily role was to identifying dementia patients from the ward handover and then engage with these patients utilizing the RITA devices. Interactions with patients would be diarize for evaluation of the project. They were also encouraged to cascade train ward staff on how the devices worked.
A 24inch touch screen and a 10inch tablet loaded with the RITA (Reminiscence) software were deployed to the two identified wards. One medical and one orthopedic ward was selected based on the on the number of patients with dementia that historically were admitted to these wards.
Initial feedback from RITA Champions was that the project has been exceptionally well received. With anecdotal reports of patients singing on the ward and “a noticeable difference to the ward atmosphere”.
Qualitative data to date:
Interviews have been undertaken with various stakeholders:
Patient:
“I enjoy everything on there (RITA), wonderful. It picks me up.”
Family Member:
“She’d (RITA Champion) been working with him in the morning…. And as soon as we got there we could see that she was there because he can speak. Yeah. She would come back on that day and say, like, what they’ve been doing throughout the day. That tells me people care… That meant a lot to us.”
RITA champion
“I find it really, really rewarding. And it’s lovely to be able to work with patients and to see that you’ve got through. There’s an impact there. It’s lovely to be able to help the patient to engage with family members that they haven’t previously”
Ward Staff
Nurse: “We had a patient that was on a DOLS. Who was always wandering and trying to escape the ward. The RITA team worked continuously with this patient and had really encouraging results the patient used to sing along to all the songs dancing and chatting to the member of staff. He recognized her every day she come into the ward.”
Ward Manager: “RITA and the Rita’s champions have been fantastic on ward… And I never thought that Rita would have a big impact on the ward, but it made a huge difference. I have noticed a decrease in our patients falls over the months and patients are calmer, and this is helping with our patients that are on enhanced supervision. And furthermore, really helps with our dementia patients. So, thank you to everyone who was involved in starting the project.”
Evaluation observation field notes:
· Discussion with RITA champion: She feels absorbed and even her own mental health has improved.
· Other benefits to patients: When RITA champions are with patients, there has been several times when they have assisted the patients with personal care needs and encouraging nutrition and hydration, which otherwise would have been very challenging when patients are agitated or aggressive.
Quantitative data
The project team is in the process of capturing falls data, length of stay and levels of enhanced supervision for the patients with a diagnosis of dementia on the identified wards. This will be compared to data from before the project was introduced. At this point we do not have data to share.
The RITA devices also captures App usage so we are able to review which Apps are most popular.
Innovative uses of RITA
· RITA used as a translator
Reported by a RC: ‘’There was a patient from a different country. And there was a language barrier. The patient was getting frustrated …the behavioural issues was down to communication and there was an app on the RITA tablet. It’s about communicating and you could set it up as a translator, so you can type in what you want to say and you can have it translated in different languages.’’
· RITA used as a communication board
Reported by a RC: ‘’I worked with a chap who had a stroke and he had speech problems and he was on an enhanced observations because he was very agitated, very abusive.
After working with him for a little while, I came to realise pretty quickly that the reason why his behaviour is because it was a struggle to communicate and the chap was used to one of those picture boards where he had to touch the pictures to communicate and he was getting so, so frustrated with the staff because he was trying to indicate his needs, that they weren’t getting. And so we used the RITA Tablet… (using the App) he just pressed I have a pain in my shoulder, my little finger hurt… we used that so that he could communicate. His behaviour was a lot calmer and you could see that visibly, be able to relax because he’d had his needs communicated and we’d understood them.’’Barriers and challenges
Covid has had an impact on the delivery of the project. Two of the RITA champions were considered high risk which precluded them from attending the wards when there were periodic Covid breakouts. This meant that at times wards did not receive the roll out support initially envisaged.
One of the HCA’s resigned from her post to take on another role in November, which meant we had less champion support on the wards.
The national predicament the NHS, Adult Social Care and Community Health and Care are facing, with patients unfortunately spending longer in acute care than required, is also having an impact on the project metrics. This will inevitably skew the Length of Stay data we are gathering.
The RITA Project impact may be linked to the presence of the RITA champions more that the devices themselves. This should become evident as we enter the second phase of the project as funding for the champions has now ended and it will be up to ward staff to utilise the devices.
Ward and therapists staff have received RITA training, but regularly feedback that due to staffing issues and ward pressures they are unable to dedicate prolonged periods of time to sitting with individual patients and to utilise RITA in the same fashion as the Champions. Once Phase 2 of the project has run its course (RITA on ward with no external support) and the impact has been evaluated we will explore if the hospital volunteers could be encouraged to take up a champion role.
Comments
Chris Shaw 13 Sep 2022
Hello Jonty. We're looking to undertake an evaluation of RITA within South Wales and it would be great if we could collaborate with respect to using the same evaluation tools and processes. Is there any update on your planned timeline please, or any initial findings you can share? Thanks in advance! Chris Shaw.
Chris Shaw 16 Sep 2022
We have a small number of devices which were deployed prior to COVID via some local champions in practice, but we're keen to pick back up on evaluation of those before expanding the roll out. It would be great to stay in touch and see if we can pool our findings into a multi-centre dataset? Are you able to drop me an email direct then we can chat further - christopher (dot) shaw2 (at) wales (dot) nhs (dot) uk.
Jonty Yazbek 14 Sep 2022
Hi Chris,
We are on the verge of launching RITA on the identified wards, so we don't have any data to report back on yet.
We planning on evaluating: Falls, Levels of Enhanced supervision, Length of stay and patient and staff experience. Our Research & Evaluation Associate will be conducting a full evaluation of the project impact which we will publish.
Have you rolled out your RITA yet?
Sarah Mackie 4 May 2022
Really interesting project! The interface reminds me a bit of those touchscreens you sometimes get on long-haul flights with simple games, music channels, films etc - which of course are designed to appeal to as wide a user base as possible, keep us in our seats and not bother the staff too much! Reflecting on that - I wonder how you are going to set things up to encourage (safe) mobilisation around the ward where appropriate? It looks like you have thought about this and have a plan for it, would be interested to hear more detail!
Jonty Yazbek 6 May 2022
Hi Sarah,
Thank you for your message. We are really looking forward to being able to introduce RITA onto our wards to help staff to support patients living with dementia or similar cognitive impairments. I think the principle behind the programme is as you described, a distraction from the situation. However it will also play an integral part of improving patient hospital experience and a method of improving communication with patients, which can be one of the contributing factors as to why patients become distressed; leading to enhanced supervision, increase in length of stay etc.
The project will not distract from the day to day rehabilitation of the patient while they are in hospital, but act as an additional aid to engage and stimulate patients between periods of “prescribed” mobilisation. If patients wanted to mobilise they will still able to, in line with standard mobility assessments to ensure safety. Our Therapies team have developed an education programme, delivered by the ward based therapists, to the ward nurses, healthcare assistants and trainee nurse associates to develop and increase their knowledge and confidence in early mobilisation. Their overall aim is to increase the percentage of patients mobilised from bed in the first three days of admission to the ward. Together these project will work together in synergy.
The delivery of our RITA project will be led by our Dementia Lead. Staff working with the patients will have a robust training programme and will be supported by our Dementia Team. We plan to capture feedback from staff, patients and family members throughout the project in order to make changes as required and gain the best outcomes.
Jonathan Yazbek 16 Mar 2022
Hi Jacqueline, great to hear that the product has been having success elsewhere already. We really hope it will help our patients and staff and in the process improve patient experience.
It would be really good to potentially share some learning if we are successful with our bid and have started our project.
Jacqueline Morton 8 Mar 2022
Jonathon we are great champions for RITA in Southern Trust. We are early in our journey but so impressed with the potential impact on patient safety, quality and experience. It s easy to use, portable and can be made so personal to the patient/client. My colleague Mairead McGahon is leading this QI project with the support of Cailin McKearney, QI Facilitator. I look forward to hearing more about your journey. We would be happy to collaborate with you and share the learning.
Comments are now closed for this post.