Q Exchange
Cancer pathway optimisation though digitisation and automation
- Proposal
- 2022
Meet the team
Also:
- Grant Vallance: Information Manager, Department of Clinical Haematology, Oxford University Hospitals Foundation NHS Trust
- Marcus Baw: GP, ED doctor and clinician-who-codes
- NHSx (NHSE) Innovation Lab
What is the challenge your project is going to address and how does it connect to the theme?
There are between 34 and 87 steps to take a lung cancer patient from referral to treatment. Many of these steps are manual and could be undertaken by automation. We are currently building a proof-of-concept digital pathway to test how this can be undertaken. We want to put all of the salient information that a clinician needs to make an informed decision into a single interface. This will speed up processes and reduce the frustrations associated with having to log into different clincial systems. There is strong data that faster treatment times lead to better prognosis. We currently have two computer science on placement building this proof-of-concept. These have been funded by the SWAG cancer alliance and the local CCG. We will need funding for 2-3 placement students to continue this important work and hence the application to Q Exchange. We will also improve patient understanding via created and curated patient information videos.
What does your project aim to achieve?
This body of work is set to achieve:
- Faster pathways leading to improved patient prognosis. This will be achieved by streamlining the pathway through digitisation and automation of the various steps in the pathway. Faster treatment times have been shown to improve prognosis.
- Reduced staff workload due to the above changes.
- Better patient experience via tailored made patient information videos (PIVs). We will create and curate PIVs, which will be automatically sent out to the patient (via SMS or email) when a test request or referral is sent, to keep the patient fully informed. This will help free up staff time to discuss, by phone or face-to-face, explain matters to those that are less digitally literate.
- Improved staff experience of managing the lung cancer pathway by using a user-centred design approach. We will be using agile methodologies and user-centred design for the digital pathway
How will the project be delivered?
I am working on the lung cancer digital pathway as part of my studies for the NHS Digital Academy Digital leadership PGDip course. I have been engaging with the trust’s digital team and together we are building a new Gloucestershire Clinical Informatics Hub which will house the pathway work. We had a recent stakeholders meeting and we had a lot of positivity about the digital pathway. We are keen to take this work further forward. We want to make this digital pathway modular and open source so that other cancer sites and trusts can benefit and also collaborate on this work. We have been working with the NHSx (NHSE) Innovation Lab to ensure that our work aligns with national digital strategies. We have pre-implementation data available to then compare later. We believe that building this pathway within a trust, rather than contracting out, can save the NHS money.
How is your project going to share learning?
We have already been building the digital pathway in an open format. The code is shared as open source on Github (https://github.com/spiritumduo/spiritumDuo), we are presenting this work at several meetings (the next one is the “Let’s Talk Digital” conference on the 18th of February 2022) and we plan to blog and generally share insights from this build on the Gloucestershire Clinical Informatics Hub web site, when this have been created. We really value the collaborative input we have already had from Glocuestershire University, NHSx (NHSE) Innovation Lab and Oxford Univeristy Hospital. We are also planning on collaborating with the National Clinical Informatics team at Digital Health and Care Wales. We hope to be able to show to others how digital innovation can happen at the front line. There are great benefits from this, including get rapid and strong end-user input on builds and much faster benefits realisation.
How you can contribute
- Building clinical software on the front line is a new endevour for the NHS, at least in Gloucestershire. We need as much help and collaboration as we can get. We need clinical expertise as well as digital expertise. Later we will also need expertise to help us navigate the maze that is MHRA medical devices sign off. Also, as we want to make the digital pathway as modular as possible (whilst being safe and userfriendly), it is important to get input from many different specialities so that the digital pathway can be built to accommodate different diseases and ways of working.
Plan timeline
| 18 Mar 2022 | Conference demo (Let's Talk Digital conference) |
|---|---|
| 1 Jun 2022 | MDT functionality completion |
| 2 Oct 2022 | 1-2 new computer science placement students to start (funding needed) |
Comments
Paul Kennedy 3 May 2022
Congratulations on being shortlisted. This certainly gets my vote. I was quite shocked with the amount of steps needed to progress a patient through the pathway. Any improvement on this is clearly valuable and dare I say it, will help to save lives. With the backlog of patients waiting for treatment this should be front and center of any funding.
Good luck with any further shortlisting and with the work your already doing.
Mark Bailey 3 May 2022
WOW, that is exciting to see that this project may get an injection of funding to help both cancer patients and healthcare professionals. I appreciate your feedback Paul.
Mark Bailey 3 Mar 2022
Hi again Kevin,
Nice you meet you earlier today at the Q community introductions.
That is an interesting question. There is a lot of hype about robotic process automation (RPA) within the NHS and from NHSX (now NHSE). There are issues with RPA though. Although RPA can be built to automate processes by controlling the graphical user interface (GUI) of the different clinical (and non-clinical) digital systems, it is not without its drawbacks. Should an input field, a tick box or message move on the screen, then the RPA solution can fail. There is not always feedback with RPA solutions, but I admit that the commerical ones do have this functionality. I see RPA more of a "patch job". It is connecting together systems that are made for a human to be the "middle man". What you need is for robust APIs (application programming interfaces) in place, that take out the middle man, the GUI and have robust communication methods and error functionality that utilise standardised protocols. These are much safer, faster, and secure. They can even be used over the internet. For you to use an RPA solution, you need either run the RPA program on your own desktop or have a virtual machine running that has the RPA program running on it.
I have already built an RPA solution for our department (github.com/Cotswoldsmaker/QuickSpiritum). It is an open source program built onto of the open source scripting language AutoHotKey. Now AutoHotKey does not have all of the bells and whistles that the commercial programs do, but it does a really good job. I speeds up my workstreams and just makes things easier. It does however now and then error, and it is only as fast as the GUI it is trying to control. If you moved to APIs (which is the plan with the lung cancer work) as much as possible, you gain so many benefits.
That then leaves you at the point of, how do you get the APIs you need to do the tasks you want. That then comes to cultural change and change methodology. It has taken me some time to get the trust to engage with us. However, we are now talking about what APIs there are available, and which ones we need to build. Exciting stuff now that we have the opportunity to make change in our trust. I hope to share these learnings with others and even help other trusts to use this new digital pathway if they are interested.
Kevin Minier 3 Mar 2022
Many thanks Mark.
Kevin Minier 3 Mar 2022
Hi Mark,
A very important project.
If I understand correctly the need is to have all the information/tests in one place? You are already aware of Robotic Process Automation e.g. https://www.sbs.nhs.uk/article/16501/Robotic-Process-Automation-RPA
Why would an RPA solution be insufficient?
Kindest regards,
Kevin Minier
Jo Scott 3 Mar 2022
Hi Mark
It sounds like a much-needed project.
In terms of the work you are hoping to do with Q Exchange funding, for the placement students...how much have you done already, or are hoping to do with this funding, to engage a range of people in the development and testing of the proof of concept (staff from different teams, patients and carers if relevant)? It sounds like it will involve a culture change to implement this successfully...I wonder if other members could provide some insights as to what Q Exchange-funded activities at this point of a project can help to set this work up for long-term success?
Best of luck with the idea
Jo
Mark Bailey 3 Mar 2022
Hi Jo,
Many thanks for your comments. In reply to your questions:
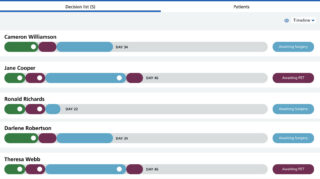
1. We have already raised £36,000 for two placement students, who are working with us from Sept 2021- Sept 2022. This money was kindly rewarded by the SWAG cancer alliance and the Gloucestershire CCG. The students and me have been working on the web app and have a functional proof-of-concept that is connected to fake patient data. We have been using this to demostrate to people the intended functionality of the new didigal pathway. Today, the app can take a (fake) patient from referral to final treatment, allowing the clinician to make requests and referrals and then informing the clinician when the results are back. We are now updating the app to have a NHS user interface format. We will move onto digitising and streamlining the MDT in the next week or two.
2. We have just had a stakeholders meeting to engage with people that are involved with the pathway (patients, doctors, admin staff and digital teams). We are demostrating the app at every opportunity, and will be doing so at the "Let's Talk Digital" conference that we are doing on the 18th of March (https://www.eventbrite.co.uk/e/253064983177). However, there is a huge cultural change needed locally. I have not noticed this so much with the clinical and admin team at my trust, but with getting the digital team to engage and allow this work to progress. This being said, we have progressed far over the last year and a half with the digital team, and we are now looking at how to integrate the work we have done so far with the trust's backend digital infrastructures with input from the digital team.
3. What we hope to acheive over the rest of this year with my current students, and then with any future students we may be lucky enough to have is to build in all of the functionality we need for a digital lung cancer app. This includes streamline requesting, referring, getting test results when they are back, an improved digital MDT, messaging system and a graphical represenation of a patients pathway progression, etc. We are making things internet-first, mobile and open source to get the best from this new digital pathway. This is also in line with NHS digital strategies.
Aklak Choudhury 1 Mar 2022
Thank you. This looks an interesting proposal. I like the thought of automisation for cancer pathways.
There are a number of human elements including patient contact at clinics, MDT discussions, radiological and pathology delays. each of which may have their own processes and IT systems. Not forgetting National cancer registries etc.
1. How will you consider integrating these pathways/processes/other digital IT platforms into one system?
2. Also ultimately people will be responsible for overseeing what data comes in and goes out - How automated can the system be in reality?
3. Is there any guidance from GIRFT to support such initiatives?
Be good to get your thought on this as you develop your idea.
Mark Bailey 1 Mar 2022
Dear Aklak,
Many thanks for your comment. Also, the points you have raised are very interesting. I have been working on digitising this pathway since Sept 2020 and so I have put a lot of thought, time and effort into it.
1. What me and my two computer science students are currently building is a full stack web app. This will link with a trust's systems via the Trust Integration Engine (TIE, most trusts use a TIE). This will then link up with the trust's electronic patient record (EPR), where we plan to house all patient related information. I am having fortnightly meetings with the digital team at my trust to work out the fine detail of all of the above. By doing all the hard work with integrating with the trust's backend programmatically, the hope is to have all of the functionality that a clinician and other healthcare staff need within a single web app. There are however some legacy systems that do not have robust API (programmatic communication interfaces). We might then have to use robotic process automation (RPA) on a virtual machine to then undertake these tasks. Eitherway, we want to hide this complexity from the end-user (the clinical team) and have them only interact with the digital pathway via the web app.
2. All patient information will be stored in the EPR. Of course, the ultimate responsibilty for safety and clinical governance will land on the CCIO and clinical safety officer for a trust. But the work we are doing is being documented and DCB0129 and DCB0160 (clinical risk management tools) will be used to show our workings and how we have designed the systems to be as safe as possible. I do however realise that we need to go through a lot of safety testing to make sure this system is as safe as possible. I hope to also get MHRA sign off for medical devices. In terms of how automated can you go, we are only looking to automate very basic tasks (ordering bloods, prefilling referral letters, chasing scan results). We are not looking at AI and "smarter" options, at least for the time being. But the local university is interested in having MSc and PhD students look at this kind of input.
3. Regarding GIRFT there some very interesting remarks from the lung cancer GIRFT team at https://www.gettingitrightfirsttime.co.uk/girft-starts-work-on-lung-cancer-review/
Dr Paul Becket:
“There is a huge interest nationally to improve outcomes for lung cancer patients, particularly focusing on implementing the National Optimal Pathway. Through our work on the National Lung Cancer Audit, we have highlighted the wide variation in practice and outcomes but have sometimes been frustrated at the inability to implement local service improvement – I’m convinced that the GIRFT methodology will allow us to do just that.
“I’m really looking forward to visiting lung cancer teams up and down the country to hear about their services and to share examples of innovative practice to help them on their improvement journeys.”
I have a proposal paper of the work that I can forward to you as well if you like.
Regards
Mark
Comments are now closed for this post.