Q Exchange
A text delivered system monitoring anaesthetic patient reported outcome measures
- Idea
- 2022
What is the challenge your project is going to address and how does it connect to the theme?
Anaesthetic departments should have a system in place to facilitate learning and quality improvement in response to feedback from patients. Collecting data relating to the quality of anaesthetic care is notoriously difficult due to the brief interaction that anaesthetists have with their patients postoperatively. A text-delivered system would allow us to:
1) Collect outcome data which could lead to systemic improvements
2) Detect and manage early complications of anaesthesia
3) Allow inter-individual and inter-departmental benchmarking
4) Empower patients to actively participate in their healthcare by using their feedback to direct quality improvement work
5) Ensure that patients receive accurate information relating to their anaesthetic – texts will include links to patient information leaflets
This project has been enabled by a partnership with the UHBFT digital transformation team and has been developed using direct patient feedback.
Initial testing has confirmed questionnaire validity, patient ease of use, and enthusiasm for the project within the anaesthetic cadre.
What does your project aim to achieve?
We aim to develop the text-based PROMS/PREMS system, complete testing and introduce into practice. We hope to use the funding to facilitate data validation, data collection from patients who are not suitable for text-based data collection, and data analysis.
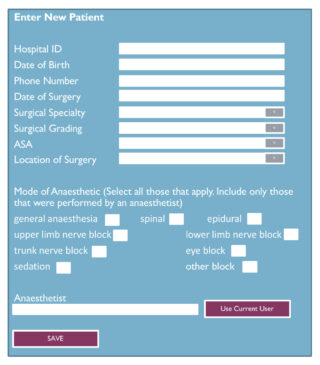
Our aim is to capture data from the full range of patients undergoing surgery with regional or general anaesthesia at UHBFT. We aim to use these data to create dashboards which can be monitored to ensure quality of care, and also to provide individualised feedback to clinicians, allowing them to review their own data against a comparable patient population. We also aim to use these data to allow rapid detection of complications of anaesthesia, such as temporary or permanent neurological injury subsequent to regional or neuraxial anaesthesia, or awareness under general anaesthesia. This will allow us to contact patients who require early assessment and follow up.
How will the project be delivered?
The system will be developed by software developers and informatics experts based within the UHBFT digital transformation team. Readership experts will review the forms before testing on a large patient population and then launching the system through several PDSA cycles. Data will be reviewed daily at first and then with less frequency depending upon the outcome of the PDSA cycles. Pareto charts will be used to ensure that the patient population completing the forms is representative and to identify missed patient groups. Data analysis will be undertaken at regular time points and presented to the department. Data will be used to create digital dashboards and individuals will be able to view their own feedback and quality data. An administrator will review data and contact select patients for specific feedback. They will also collect data on tablets from patient groups who struggle to access the digital platform.
How is your project going to share learning?
The James Lind Alliance has listed in it’s top 10 research priorities for anaesthesia and peri-operative care “What outcomes should we use to measure the ‘success’ of anaesthesia and perioperative care?”. This project will allow us to test the validity of a number of different quality indicators on a large scale. If this project achieves its aim of providing continuous quality indicator data which can be used for service improvement, it could be scaled up to a regional or national level. This would allow inter-departmental benchmarking using validated endpoints.
Individual clinicians will be able to view their data and compare it to departmental data to allow reflective learning and improvement.
All project material will be shared with the Q community.
Project work will be published and presented at international conferences such as the International Forum on Quality and Safety in Healthcare, or the Institute for Healthcare Improvement Forum.
How you can contribute
- What patient reported outcome measures would you suggest that we measure after anaesthesia?
- Should we be collecting these data alongside subjective measures (e.g. pain score in recovery, first temperature in recovery)?
- Have any of you developed anything similar (I know that there is a wealth of experience collecting PROMS data relating to surgical outcomes) and what advice would you offer us?
- We would love to hear your thoughts on the project, and any suggestions that you have to help us make the project better.
Plan timeline
| 1 May 2022 | Identification of stakeholders and engagement phase |
|---|---|
| 5 Jun 2022 | Development of PROMS questionnaires |
| 3 Jul 2022 | Software development phase |
| 2 Oct 2022 | Initial software testing PDSA cycles |
| 4 Dec 2022 | Evaluate and refine platform |
| 8 Jan 2023 | Start of employment date for system administrator - training for use |
| 29 Jan 2023 | Platform launch date |
| 19 Feb 2023 | First data review and analysis time point |
Comments
Robert Colgate 8 Mar 2022
Elise - hi. I think there could be some overlap with the project I am leading (see 'who is afraid of mental health triage?'). I would certainly be interested to see any mental health items that you try out and include, and also those items that you reject.
Jo Scott 23 Feb 2022
Hi Elise
This sounds like an interesting project. Have you spotted this idea? https://q.health.org.uk/idea/2022/open-access-evidence-maps/ I wonder if there might be some useful inspiration and learning you could share related to measuring and exploring patient experience?
It may be worth providing more detail on how you will achieve these two outcomes:
4) Empower patients to actively participate in their healthcare
5) Ensure that patients receive accurate information relating to their anaesthetic
I'm unsure from what's included so far on how this project will enable this?
There may be information and inspiration from NHSEI's digital playbooks that could help strengthen the idea? https://www.nhsx.nhs.uk/key-tools-and-info/digital-playbooks/perioperative-digital-playbook/
Best of luck with the idea!
Jo
Elise Hindle 21 Mar 2022
Hi Jo,
Thanks for the feedback - I have included a bit more information on the points that you have raised.
Elise
Comments are now closed for this post.