Q Exchange
Volatility, uncertainty, complexity & ambiguity + Quality Improvement + Plan Do Study Act
- Idea
- 2020
Meet the team
What is the positive change that has emerged through new collaborations or partnerships during Covid-19 that your project is going to embed?
The Covid-19 pandemic has put the UK health and care workforce under unprecedented pressure. The workforce had been struggling to cope even before the pandemic took hold. Staff stress, absenteeism, turnover and intentions to quit had reached alarmingly high levels in 2019.
The impact of the pandemic on the nursing and midwifery workforce has been unprecedented and will be felt for a long time to come. The crisis has also laid bare and exacerbated longstanding problems faced by nurses and midwives, including inequalities, inadequate working conditions and chronic excessive work pressures.
The health and wellbeing of nurses and midwives are essential to the quality of care they can provide for people and communities.
This situation has been investigated and the following report has been produced:
‘The courage of compassion: Supporting nurses and midwives to deliver high-quality care, The Kings Fund, September 2020’
The positive change: To embed the report recommendations into activities.
What does your project aim to achieve?
This idea is to take the complete set of SOPs in a GP surgery and process map the processes defined within. Process visualizations will then be created for each of the defined processes. An iterative process will be used with Surgery staff to ensure that the process visualizations are representative of everyday practices at the Surgery and that they are compliant with relevant SOP requirements.
The approved process visualizations will then be audited against the report listed above. All areas of each process where improvements to the process could be made to more fully meet the requirements/recommendations of the above report will be listed. The lists will be used to establish QI projects to identify the improvement and once approved, modify the relevant process visualization.
The number of processes treated in this way may need to be limited to fit with the lifetime of this idea.
How will the project be delivered?
A Scrum framework will be used during the design of the process visualizations. See https://www.scrumguides.org/docs/scrumguide/v2017/2017-Scrum-Guide-US.pdf#zoom=100
The design process can be found here: http://www.catmalvern.co.uk/nhs/CreationProcess.html
How is your project going to share learning?
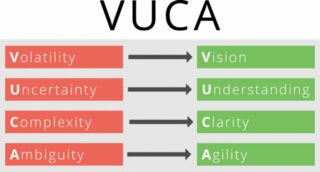
The process mapping techniques use will facilitate moving from a situation of Volatility, uncertainty, complexity & ambiguity to a situation of Vision, Understanding, Clarity and Agility.
How you can contribute
- I'm looking for a GP Surgery to join me in this idea.
Comments
Thomas John Rose 16 Oct 2020
Unfortunately due to tier 2 lockdown Streatham PCN are no longer to take part in this project.
Peter Dudgeon 12 Oct 2020
Hi Tom,
I've taken another look at your idea, now that you've fleshed it out. Looks like you've had some volunteers to work with you, which is great. In terms of process visualisation and standard operating procedures, I was curious as to what method's you would be using. It struck me that there are members of the Lean SIG who might be interested in supporting with best practice ideas in that area (if they haven't already)
Best of luck,
Pete
Thomas John Rose 13 Oct 2020
Peter,
Thank you for your comments. Regarding the methods we will be using I do like to keep things as simple as possible. First work processes are identified. We do have our first process – child immunisation. This process has been complicated due to COVID 19 restrictions and it is important that no patients miss out. Once a process has been identified then a process flow chart will be produced. Traditional process mapping techniques will not be used. I use a technique developed over many years that has proved to be very effective. The process flow chart will identify a series of tasks. Each task will be documented using various visualization techniques i.e. text, short podcasts, images, video clips, screen shots, etc. All files will be linked to the task via a web page on an intranet or the internet.
An iterative process, between the visualization designer (that’s me) and the team of people that undertake the process in their daily work, will define current practice as represented by the visualization. This iterative process will be done via email and through an updated visualization viewed on line.
QI projects can be used to improve the current practice using the process visualization as the agreed baseline with all stakeholders working from the same knowledge of the process. Additionally the requirements of all relevant SOPs can be reviewed to ensure that the process is fully compliant. Any informal ‘work abounds’ can be formally incorporated into the process visualization if authorised.
Using good systems engineering techniques throughout the final process visualization will be a documented and authorized representation of a best practice process that all stakeholders can understand and use as a baseline for future improvement and the incorporation of new technologies and IT systems.
Clearly issues like Lean and sustainability can be incorporated into the process at any time via a QI project.
At this point I’ve had no communication from members of the Lean SIG. It would be really good to have some feedback on the above from any Q member.
Tom
Emma Rowley-Conwy 5 Oct 2020
Yes please send an example so I can understand more. My email is emma.rowley-conwy@nhs.net
Thomas John Rose 5 Oct 2020
The IT applications used to create the process visualizations are standard Microsoft products that can be found on many office PCs.
Thomas John Rose 5 Oct 2020
Emma,
Here is the link http://www.catmalvern.co.uk/nhs/NatSSIPs03.html
This visualization has been designed as a demonstration of the techniques I use in my process visualizations. I've taken a very complicated documented standard and created a visualization with added detail to offer more clarity. Best viewed on a PC rather that a mobile phone. Just click on any box in the visualization for more detail of the task. Visualizations can be designed for viewing on a mobile phone - I've jut not done in this case.
Tom
Emma Rowley-Conwy 4 Oct 2020
i would be interested to understand more. I am pcn cd of 7 practices in south london. Embedding change in a team is really difficult and having SOPs that are visual and easy to understand would be a helpful idea. E.g. we need to write a SOP for managing child immunisations, this is a focus during covid and we have maintained immunisation levels, but they could still be higher, we want to work at scale and have consistent approach across the network (and if this works then can be rolled out pan the borough and even SELCCG) Most of the call and recall work is done by admin staff and getting across the procedures easily would be of benefit. We have done some of this in a project to clean up diary in emis - with a manual that is very visual with lots of screenshots - but i think we could go a lot further - the barrier for us is having the skills and the IT programmes to write a sop in this visual diagrammatic way. Is this what you want to cover in this project?
Thomas John Rose 7 Oct 2020
Via email:
Yes
1. Use to record vaccines given, using a standardised template to ensure correct codes
2. Used to run searches to call and recall patients who need immunisation
Emma
Thomas John Rose 6 Oct 2020
Emma,
Does your managing child immunisation process involve the use of EMIS?
Tom
Thomas John Rose 4 Oct 2020
Emma,
Thank you for your comment and interest in my idea. Your child immunisation SOP is exactly the sort of process that I am keen to visualize using a technique that I have developed over the years. The visualizations are web or intranet based and can include screen shots, images, links to web pages etc. I like to use a very simple flow chart of the process and from that create links to any amount of detail for each task in the basic flow chart. I can send you an example if you like.
Charles Henderson 3 Oct 2020
Tom, Your research sounds to be complementary and synergistic with a piece of research that Malcolm Fisk at DeMontford is contemplating. Given the challenges of recruiting GPs you may find it advantageous to cooperate.
Thomas John Rose 4 Oct 2020
Thanks Charles. I have contacted Malcolm by email.
Regards
Tom
Robert Varnam 3 Oct 2020
This is an intriguing proposal. Can you say more about the purpose? What will be better as a result of having a new set of standardised processes?
Also, one challenge to the proposed methodology is that there's enormous heterogeneity in general practices, which makes standardised processes very difficult to adopt without adaptation elsewhere. It would be helpful to understand how you envisage a standard process developed in one practice being used by other practices.
Thanks, Robert
Thomas John Rose 3 Oct 2020
Robert,
Thank you for your comment and very relevant questions. I will answer your questions one at a time.
The idea is not to have a new set of procedures – the idea is to document, in the format of process visualizations, what is required by relevant SOPs and what is currently done in the practice. The benefit of having a set of documented processes is that it will be clear to all how thing are done across the practice. This will facilitate change and allow change to be managed. All members of the practice will be able to have an informed input into the change. This will be better than current change practices. Change is going to be at the forefront of minds in the NHS and that’s not just as a result of the NHS Long Term Plan.
As an example of the requirement for change we just need to have a look at a selection of documents:
1. National patient safety syllabus 1.0 – Training for all NHS staff, January 2020
2. QUALITY IMPROVEMENT Sustainability in quality improvement: redefining value, SUSTAINABILITY Future Healthcare Journal 2018 Vol 5, No 2: 88–93
3. The courage of compassion: Supporting nurses and midwives to deliver high-quality care, The Kings Fund, September 2020
Further examples: To ensure that the best use is being made of IT systems, e.g. EMIS Health and new forms of communication designed as a result of COVID 19, e.g. remote consultations. Again EMIS Health and others have been doing some great work in this area.
Heterogeneity in general practice is predominately associated with diagnostics and treatment of patients – activities adequately addressed by NICE. These activities will not be covered by the proposed process documentation.
IT systems, including AI, are dependent on data. Any error in the data collection will be reflected in the value of the output. The timeliness and reliability of data collection is becoming increasingly important in the NHS. Here a degree of standardisation is necessary. Process efficiency and effectiveness is also important. In order for all members of the practice to be able to have an input into change (improvement) it is necessary to have Vision, Understanding, Clarity and Agility of processes (what people do day to day) and not Volatility, Uncertainty, Complexity and Ambiguity which of more often than not the current situation.
The challenges currently being faced by general practice (and the rest of the NHS) are the same for all practices. The process visualizations will be designed to be sufficiently generic to accommodate specific circumstances but nevertheless be of sufficient value to justify the documentation effort.
Please comment on the above and I will respond.
Regards
Tom
Iona Lancaster 18 Sep 2020
Hi Tom, I agree this sounds intriguing, looking forward to understanding your thinking in more detail, Iona
Thomas John Rose 4 Oct 2020
Iona,
Thanks for your comment. I'm slowly adding a bit more detail and creating some interest.
Tom
Peter Dudgeon 2 Sep 2020
Hi Tom,
Myself and my colleague Emma Adams (Health Transformation Partnership) are supporting the Health Foundation this year by fostering conversations between Q members and encouraging collaboration. We were Exchange applicants last year, so we’re hoping that our experience will help us to help others, as their ideas take shape.
Your project is intriguing. I know it's early days, and I'm looking forward to hearing more detail. I am presuming that this is linked in to the complexity Special Interest Group? Also from your description, it sounds as though you're aiming to make complex systems merely complicated, and complicated systems simple ones. Have I understood this correctly? Looking forward to helping foster conversation with other members of the Q community as the project idea progresses. All the best, Pete
Thomas John Rose 2 Sep 2020
Peter,
Thank you for you for your comment and interest in my idea. This idea is not currently linked to the Complexity SIG but that is a good suggestion. The aim is to reduce VUCA. Clearly there will be degrees to which this can be achieved so yes you are right in your understanding of the idea. I'm sure that the work done in 'Engineering Better Care' will play a big part in the proposed framework.
Comments are now closed for this post.