Q Exchange
Reducing Unnecessary Antibiotic Prescribing in the Emergency Department
- Proposal
- 2020
Meet the team
Also:
- Dr James Harrison
- Dr Mariyam Mirfenderesky
- Mr Geoff Benge
- Ms Semra Ali
- Ms Tracey Lee
- Ms Shivani Shah
- Divina Bunoan
What is the positive change that has emerged through new collaborations or partnerships during Covid-19 that your project is going to embed?
Much work has already been performed through national CQUIN initiatives and antibiotic stewardship programmes to reduce unnecessary antimicrobial consumption in Secondary Care. However the Emergency department requires specific interventions more akin to primary care.
The COVID-19 pandemic saw the introduction of novel ways of streaming and cohorting patients through the emergency department. The North Middlesex Hospital, North London, was identified early in the pandemic as the second most COVID-pressured Trust in UK. General practitioners were mobilised to the front door to stream ‘well’ patients with respiratory illness to the Urgent Treatment Centre, avoiding the main department. This improved flow within the department, decreased waiting times, facilitated faster diagnosis, treatment and discharge.
Given this new triage process we wish to enable enhanced models of care within the UTC; improve antimicrobial stewardship, reduce unnecessary antibiotic prescriptions, adverse side effects and decrease antimicrobial resistance as well as realize substantial financial savings.
What does your project aim to achieve?
Antimicrobial resistance is significant global health threat. Respiratory infections are one of the most common reasons for oral antibiotic prescriptions in the NHS, with 50% of all acute respiratory infection visits leading to an antibiotic prescription compared with a warranted 9% if treatment guidelines are used.
Differentiating between bacterial and viral infections is challenging. Coupled with perceived patient wishes, often the fastest and easiest route to discharge from an outpatient setting is to prescribe an antibiotic.
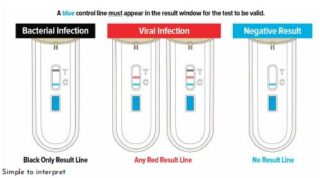
POC measurements of CRP have been shown to reduce antibiotic prescribing in acute respiratory infections in primary care. We wish to trial the NICE endorsed FebriDx test which provides semi-quantitative measurement of C-reactive protein (CRP) and qualitative measurement of myxovirus resistance protein A (MxA) (a protein marker that is raised in the blood in acute viral infection); coupled with a behavioural change education programme and qualitative output metrics to reduce antibiotic prescribing in the emergency department.
How will the project be delivered?
The project wishes to investigate whether tests that improve clinical decision making in antibiotic prescribing at the point- of- care (POC) coupled with behavioural change techniques can support antimicrobial stewardship.
The project will be run from the Urgent Treatment Center at the NMUH emergency department, and will target patients presenting with acute respiratory infections. Algorithms will be developed which take into account the clinical history, examination and results of the POC test. An ED consultant and ED practice development nurse will be responsible for the implementation of the scheme in ED. The pathology manager and point of care lead for the Trust will ensure training, validation and internal quality control of POC test. The effect on defined daily doses of antibiotics, and cost implications will monitored by the ED pharmacist, Trust antimicrobial pharmacist and Trust Antimicrobial Stewardship lead. The overall project will have oversight from the Trust Improvement lead.
How is your project going to share learning?
This project is strategically aligned with the Uk 5-year action plan for antimicrobial resistance ambition to reduce antimicrobial use in humans by 15% by 2024 . Novel strategies are required to drive down antimicrobial prescribing. The ED has specific challenges as other successful primary care initiatives such as delayed scripts and reattendance are not suitable for this setting, and flow remains a primary consideration.
The FebriDx test; the combination of the CRP and the novel MxA protein has not been trialed before in this setting. The results of this project would be wide reaching, with implications for both ED and primary care departments across the country. This project requires large system and behavioural change in one of London’s busiest emergency departments, with a high turn over of staff and unpredictable external pressures.
How you can contribute
- Suggested improvements
- Behavioural change and human factors input
- Achieving system change in dynamic departments
- Collaboration; primary and secondary care, clinical commissioning groups
Plan timeline
| 1 Apr 2021 | Develop a Standard Operating Procedure |
|---|---|
| 1 Apr 2021 | Develop patient education campaign material ; consider behavioural change elements |
| 1 Apr 2021 | Develop systems to monitor and review antibiotic prescribing |
| 1 Apr 2021 | Develop systems to monitor patient re-attendances to ED |
| 1 Apr 2021 | Generate data reports and informatics to identify patient cohort |
| 1 Apr 2021 | Look at systems and flow within the department. |
| 1 Apr 2021 | Procure and validate POC tests. Write training manual |
| 5 Apr 2021 | Develop prescriber educational material; behavioural change |
| 5 Apr 2021 | Develop prescriber questionnaires; qualitative aspects, compliance, satisfaction. Qualitative. |
| 5 Apr 2021 | Monthly tracking of antimicrobial consumption and cost |
| 3 May 2021 | Patient satisfaction surveys; develop. Consider qualitative aspects |
| 3 May 2021 | Training and education of doctors, nurses and HCAs |
| 9 May 2021 | Pilot study; 50 patients |
| 2 Jun 2021 | Project roll out; commencement of main project |
| 3 Jun 2021 | Audit and monitoring; continuous. Weekly PDSA. |
| 3 Jun 2021 | Feedback to prescribers and department; weekly ongoing |
| 20 Jun 2021 | Monthly interim analysis; for x3 |
| 30 Sep 2021 | Project wrap up |
| 29 Oct 2021 | Results analysis |
| 1 Dec 2021 | Presentation of results at national conference or equivalent |
Comments
Prof Cliodna McNulty 19 Oct 2020
this is a very interesting project combining CRP with the MxA protein assay. One of the problems with the CRP is you can get non-specific increases, and also when clinicians get an intermediate result of 20-100 they tend to prescribe antibiotics. so it would be useful to have a second assay alongside it to establish the likelihood of viral infection.
I suggesting starting with a smaller feasibility and/or pilot RCT.
I think finding out how people interpret results - despite test pack guidance will be useful.
size of the instrument is important too - I am assuming this is a point of care test
Victoria Jones 20 Oct 2020
Dear Prof McNulty thank-you for your comments. Yes this is a small POC test. We will indeed start with a small feasibility study before the main project roll out. If we were successful in our bid it would be great to collaborate to further develop the qualitative aspects that you have outlined, and the acceptability of the outcome ( i.e. no antibiotics) to both prescriber and patient. You have national experience of such projects, and such outputs would add much value to our understanding of how the test is used and its overall impact in reducing antibiotic consumption in real world scenarios.
Neil Stone 19 Oct 2020
Innovative idea for antimicrobial stewardship which is only becoming more important as a result of COVID.
Many will be unfamiliar with the MxA protein assay - clearly warrants evaluation however.
Mariyam Mirfenderesky 19 Oct 2020
Many thanks Neil for your comments. Yes you are absolutely right. The most exciting aspect is the novel MxA protein...and does measurement of this combined with clinical algorithms within an ED department reduce antimicrobial consumption and prove safe to use. That is what we wish to find out. The results will be important nationally.
Elizabeth Beech 30 Sep 2020
Effective primary care strategies to optimise antibiotic use in RTI require use of a delayed prescription strategy, and NICE guidelines support this. UK primary care systems that have tried to implement use of CRP POCT to optimise antibiotic use in RTI have failed to do this well mainly due to poor use of delayed prescribing strategies. So my top tip is to really get this into the plan and with an working well - don't need a CRP POCT to do that either, so could get working on that anyway.
Second tip is behavioural - consider unintended consequences that patients may reattend next RTI for the assurance of a test of 'wellness'. Scandi countries have reported transfer of behaviour from 'antibiotic seeking' to 'POC test seeking'
Third tip is check the evidence base - good consultation skills 'conversation' delivered sustained reduction in inappropriate antibiotics c/w CRP POCT at second winter - so consider how measurement beyond one winter fits into the plans. Strongly advise run charts for at least 2 years to identify impact
Children wise - do ask Alicia alicia.demirjian@phe.gov.uk for the learning from the work their ED did testing CRP POCT in children. I recall unintended staff behaviour too - diverted CRP testing requests to the ED POC as it was 'quicker' and so ED staff spent lots of time doing tests that were not part of the plan
Lastly shared learning from ToDipOrNotToDip - reminder to treat the patient not the test
Mariyam Mirfenderesky 19 Oct 2020
Many thanks Elizabeth for your very useful comments here and off line.
Your points particularly re transfer of 'antibiotic seeking behavior' to 'POC seeking' is a relevant point, as well as the use of the test for alternative reasons within the department. It would have to be strictly policed.
I think what is unique here, and what has not been tried in this setting before is the MxA protein and how that changes the dynamics of prescribing when combined with the POC CRP.
I have been in contact with Alicia as you suggested. This has lead me to Dr Cliodna McNulty (Joint Clinical Lead and Head of PHE Primary Care and Interventions Unit & Consultant Medical Microbiologist, National Infection Service, Public Health England, and Honorary Visiting Professor Cardiff University).
She has suggested many useful points, which we would hope to take forward in collaboration if successful in our bid.
Comments are now closed for this post.