Q Exchange
Incontinence: Let’s change the flow
- Proposal
- 2019
What is the challenge your project is going to address and how does it connect to your chosen theme?
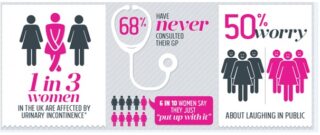
One third of women suffer from urinary incontinence (UI) and up to half of women have pelvic organ prolapse (POP). There is currently a long waiting list into secondary care urogynaecology services for these women. UI and POP are shown to significantly impact: on quality of life, personal finances ,psycho social issues , ability to work , relationships and the health economy.
It is estimated that it can take women 6-9 years to seek help for symptoms of incontinence and when they do, access to expert care is vital. NICE guidelines (2019) state physiotherapy as first line management for stress urinary incontinence.
Once patients have waited to be seen in urogynaecology , many are referred to physiotherapy with a further wait for physiotherapy intervention. In addition, many have been prescribed medication or sent for further investigations. This results in even longer waits for access to appropriate conservative treatment for their condition.
What does your project aim to achieve?
The NHS long-term plan describes the need for outpatient care transformation with care shifting closer to home and states that GP practices will deliver a wider range of specialist care services for patients from a range of health professionals, including physiotherapists.
According to the Health Foundation collaboration between primary and secondary care remains a challenge which can often lead to unnecessary referrals and inappropriate patient pathway adding to patient anxiety.
To improve access to appropriate specialist pelvic health physiotherapy intervention, at first contact for UI and POP, in line with NICE guidance (2019). It is anticipated that most of these patients could be discharged after assessment, without requiring medical follow-up. This would reduce the wait for appropriate treatment for patients, decrease prescription of medication, reduce unnecessary investigations, with an overall cost saving. It would also free up time in GP and urogynacology clinics.
How will the project be delivered?
The project will delivered in primary care by a specialist first contact practitioner (FCP) with close link into specialist secondary care, giving patients access to the most appropriate clinician at the first contact. Patients will self-refer to the clinics using a self-completed proforma developed as part of the pilot.
Should red flags or other concerning features be identified, referral to fast track pathway can be initiated. For those patients who require further management, the FCP will have the expertise to streamline the referral to the correct management pathway.
The project will provide a clinic once per week for six months, followed by a month for dissemination of outcomes. The team have links with local CCG’s following successful MSK FCP projects funded by the Health Foundation and have already expressed interest.
Funding will provide the specialist clinicians described above to deliver clinics and analyse and disseminate the outcomes.
What and how is your project going to share learning throughout?
Feedback will be delivered to GP practices and local CCGs, secondary care and special interest groups locally and nationally.The clinicians involved are experienced in presenting and delivering project information to various medical and health professional teams. Previously winning awards for poster presentations. Specialist interest groups including POGP (pelvic, obstetrics and gynaecology physiotherapy), IUGA (international urogynaecology association) and ICS (international continence society) conferences. The team have published the results of studies in the POGP peer-reviewed journal. The team are members of IUGA and POGP, which has built links to open opportunities to present in the future.
Project aims to:
- Publish results in peer reviewed journal.
- Increase patient awareness regarding management of UI and PO, presenting to patient and community groups and patient forums.
- Increase use social media for specialist interest groups to promote project, including the Q community.
How you can contribute
- Help with access to supportive evidence or experience of similar services.
- Advice regarding sustainability of successful pilots in a challenging financial environment.
- Health Foundation support with expert data analysis and promotion (this was vital in previous HF projects).
- Experience to inform challenges with working across organisational boundaries and advice on overcoming barriers.
- Critical challenges to improve project management.
- Signposting resources and guidance and offers to share previous similar project experiences.
- Highlighting any ongoing funding which may assist with project or potential developments.
- Ideas on next steps or potential to extend project into new areas.
- Help with influencing policymakers eg HEE, STPs, Clinical Senate, PCNs, CEPNs and NHSE
Plan timeline
| 1 Dec 2019 | Appoint project manager from team |
|---|---|
| 1 Dec 2019 | Confirm GP partners |
| 1 Dec 2019 | Confirm appropriate insurance and indemnity arrangements are |
| 1 Dec 2019 | Confirm clinic start dates |
| 1 Dec 2019 | Confirm practice accomodation |
| 1 Dec 2019 | Create clinic initial assessment and outcome forms |
| 1 Dec 2019 | Develop IT solutions/web/referral form/information feedback |
| 1 Dec 2019 | Develop data collection and reportingprocedures |
| 1 Dec 2019 | Negotiate release of Clinicians, plan backfill arrangements |
| 1 Jan 2020 | Present plan to all GP partners |
| 3 Jan 2020 | Develop poster for GP surgery/info for practice web site/ le |
| 6 Jan 2020 | Train GP reception staff/nursing staff in project details |
| 8 Jan 2020 | Confirm clinic time and location |
| 14 Jan 2020 | Ensure all GPs are aware of project and start date |
| 15 Jan 2020 | Confirm IT readiness, availability of sundries etc |
| 28 Feb 2020 | Data analyse and initial results presented to team |
| 17 Mar 2020 | Make any clinic adjustments based on early results-on-going |
| 15 Jul 2020 | Write up project outcomes |
| 22 Jul 2020 | Prepare poster/powerpoint presentation |
| 6 Aug 2020 | Attend appropriate venues/courses/conferences to present |