Q Exchange
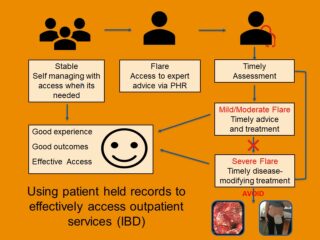
Using patient held records to effectively access outpatient services
- Proposal
- 2019
Meet the team
Also:
- Pete Carpenter, Delivery Director
- Richard Lee Wright, DIrector of Insight
- Azhar Ansari, Consultant Gasteroenterologist
- Mark Watson, STP Digital Lead
What is the challenge your project is going to address and how does it connect to your chosen theme?
Current outpatient models provide a structure for regular clinical review, regardless of clinical need at the time of the review.
Outpatient cancellation and Did Not Attend rates of up to 20% in England are indicative of problems associated with the current system which does not support patients who need urgent attention e.g. during an IBD flare, from timely advise and review in the most appropriate setting. This adversely impacts on the patient’s quality of life, ability to work and functionality and results in higher costs to the wider health care system including primary care, and increases surgical/pharmaceutical intervention.
In addition to sharing information PHRs can also be utilised to improve the flexibility of access and the overall quality of outpatient services; reduce negative consequences to the wider health care system by preventing complications as a result of delays in access to the most appropriate care; and improve the quality of life of patients who live with IBD.
What does your project aim to achieve?
We will evaluate the impact of IBD patients accessing expert healthcare as clinically needed through a PHR, rather than via the current out patient model. We expect this to improve patient experience and outcomes, and more effective use of professional time.
We will deliver this by adopting/adapting an existing PHR IBD out patient model to spread to a new Trust, learning from previous evaluation, and focusing on gaps in evidence.
Working with patients, clinical, and digital teams, we will support a local IBD team transforming their outpatient service using PHR, to optimise local pathway and evaluation opportunities.
To deliver on resource, evaluation will focus on the impact of demand to the service and the effect on staff and patients. We will provide a case study and aim to calculate the value this change has had to service.
This project will contribute towards the body of evidence/toolkit supporting replicability in outpatient transformation for specific patient populations and need.
How will the project be delivered?
Katherine Sykes, Q member, will lead this project working with local clinical and digital teams, patients, the Q community, and KSSAHSN Programme and Analytics support.
The project will be tightly managed with project management through the AHSN, who will hold a live risk register. We know from similar projects that expected risks can include lack of engagement from senior management and pressure on clinical time. We have mitigated against this by allocating funds for clinical backfill as detailed. We will keep senior management cited on all work to ensure we have their full support and any barriers/risks are recognised and mitigated including avoiding any loss/pressure to the system.
We will actively seek Q insights and support especially when looking at techniques to engage stakeholders, and suggestions for focus of evaluation that support the wider objectives of this programme. We will collaborate and share our learning and outcomes with the community.
What and how is your project going to share learning throughout?
A core remit of the AHSN is to disseminate learning. We will use this project to engage stakeholders within our region and across the AHSN network.
During the projects initiation workshop we will map out needs, opportunities, challenges, and barriers for this project, share learning from stakeholders, including patients, and from show casing a local example of this type of model in IBD out patients.
A steering group will meet at least quarterly once the project is established to evaluate progress and address any risk.
We will collaborate and share our learning and outcomes with the Q community as required and at least quarterly on the project.
At the end of the project we will produce a free toolkit to showcase our learning and will host at least one webinar that will be shared with the Q community.
We will also write a case study to illustrate our findings and the impact of transforming access to expert healthcare when needed on this patient population.
How you can contribute
- Critical friends- have we missed a deliverable opportunity in this proposal?
- Fixers- Is the community aware of similar projects in this clinical area and using PHR?
- Collaborations are very welcome, in particular to develop a wider toolkit for out patients models that benefit different patient populations.
- Strategy- are we cited on relevant strategic opportunities, barriers, or challenges?
Plan timeline
| 6 Jan 2020 | Mapping workshop pathway, evaluation, stakeholders |
|---|---|
| 6 Jan 2020 | Mobilisation of Project |
| 6 Apr 2020 | Steering group meeting – progress update, and Q update |
| 1 Jun 2020 | Go live- access via PHR |
| 13 Jul 2020 | Steering group review- implementation review |
| 14 Sep 2020 | Workshop- Evaluation |
| 16 Nov 2020 | Webinar and toolkit development |
| 7 Dec 2020 | Workshop- Dissemination of findings |
| 4 Jan 2021 | Project closure incl. budget |
Comments
Bettina Kluettgens 2 Oct 2019
This is an interesting project. Have you looked at various evidence arising from research into 'Patient Initiated Clinics'?
Have a look at the work done by the South West CLAHRC
https://www.arc-swp.nihr.ac.uk/research/ahsn-penclahrc-project-patient-initiated-clinics-pic-for-people-with-long-term-conditions
Chris Thomas 26 Jul 2019
Could there be an opportunity for your Project to link with/build upon Marianne Williams IBS Webinar Project – Somerset (subsequently NHS Patient Webinars)?
Perhaps there could be a Pathway connection between the current Primary Care benefits from the webinar, and the proposed Outpatient Services for IBS Patients?
That is, a Tool Kit – Sussex, for outpatient services, and the webinar may enhance the Pathway and possibly be applied to other long term conditions.
Chris Thomas 14 Jul 2019
Personal experience of inefficiency in the hospital discharge arena, and the potential of patient empowerment using patient held records lends my support for your idea.
Comments are now closed for this post.