Q Exchange
Co-design to improve conversations & shared-decisions for urgent care
- Proposal
- 2019
Meet the team
Also:
- Tony Goring
- Nathalie Delaney
- Jennifer O'Malley
- Gill Brook
- Claire Vasler
What is the challenge your project is going to address and how does it connect to your chosen theme?
Local QI work has demonstrated areas of excellent communication between patients and health care professional about patient preferences in the event of the need for urgent treatment, where the likelihood of improvement is uncertain or low. In these cases agreements about patient’s wishes in relation to realistic treatment options are clear and well documented . However, our QI work has also identified that this is not consistent and there is a need to improve the quality of these conversations and increase confidence in healthcare professionals when they are involved in shared decision-making with patients and families.
We are in the process of implementing ReSPECT (Record Summary Plan of Emergency Care Treatment) in our local health community. Whilst there are training materials (eLearning, videos) which have been produced by national teams, there is little available which involves both patients and staff to improve the quality of conversations and confidence and experience.
What does your project aim to achieve?
By focusing on the experience of the conversations patients and families have with healthcare professionals about preferences for emergency treatment, we will identify where the strengths are and areas for improvement. The aim is to surface change ideas from both staff and patients by using focus groups and then hold co-design events to expand on identified themes from which we can capture ideas for change. We would then use QI methodology to test the ideas and measure impact with patients and clinical teams. Depending on the interventions chosen, we would want to create materials and approaches for training of healthcare teams to improve patient experience of conversations about future emergency care. We would see an improvement in the quality of these conversations with personalised patient preferences being captured.
We would also be keen to explore what information is helpful to make available to the public to create “readiness” and a better experience for these conversations.
How will the project be delivered?
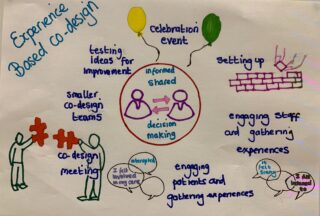
We will be using both Model for Improvement and Experience Based Co-design as a guiding methodology to gather experience of these conversations for patients and for staff. The aim is to host co-design events where touch points are discussed and then plan co-design activities and test ideas. Through these events it will become clearer where we will focus our improvement interventions. We will involve our Patient Leaders in the local area and our Patient Experience team to support selection of staff and patients to participate. We have met with a local Patient Leader who has agreed to put us in touch with the West of England Patient Change Makers with whom we will hold our first focus groups. We have support from colleagues in the West of England Academic Health and Science Network to arrange co-design events and will use their experience to help us. The WEAHSN is leading the regional project for our healthcare communities to move to using the ReSPECT process.
What and how is your project going to share learning throughout?
We plan to share through our Twitter channels, through our local AHSN and through the Patient Experience Q Community SIG. We also have a CCG working group who will be able to support sharing of our work. I am learning (slowly) how to sketch note so will try to update progress using sketches! We will also use networks such as the Bristol Death Cafe and other community groups such as Bristol Older People’s Forum.
How you can contribute
- Can you share examples of EBCD in shared-decision in relation to advance care planning, shared decision-making?
- How best can I find patient participants?
- Anyone else want to join this project from my area?
Plan timeline
| 1 Nov 2019 | Start promoting project to recruit patient participants |
|---|---|
| 1 Nov 2019 | Start promoting project to recruit staff participants |
| 1 Dec 2019 | First focus group interviews patients |
| 1 Dec 2019 | First focus group interviews staff |
| 1 Feb 2020 | Second round focus group interviews |
| 1 Mar 2020 | Thematic analysis |
| 1 Apr 2020 | First co-design event |
| 1 May 2020 | Second co-design event |
| 1 Jun 2020 | Co-design team plan interventions |
| 1 Jun 2020 | Third co-design event |
| 1 Jul 2020 | Testing of ideas and measurement |
| 1 Oct 2020 | Celebration event and video |
Comments
Helen Crimlisk 23 Mar 2023
Hi Seema - i like this approach particularly as it is at the emergency end of the care pathway when there may be less time to make coproduced decisions regarding care. Having anticipatory processes such as ReSPECT will help ensure patient and carer voices are heard and acted upon in a way which makes sense to them.
Emma Adams 25 Jul 2019
Hi Seema. NHS Scotland have been doing a lot of work around anticipatory care planning. Might be worth looking at their work for insights into how they have involved patients. https://www.nhsinform.scot/campaigns/anticipatory-care-planning
Good to see this happening in my region!
Kind regards
Emma
Ruth O’Dowd 3 Jul 2019
Hello Seema
I really like this idea, it links to the "what's important to me" concept and I think is really important area for improvement in our conversations.
Ruth
Seema Srivastava 8 Jul 2019
Thank you Ruth. Yes the "what matters most" aspect is really very important. From my conversations today with a fab Patient Leader local to our area, I think there is also something about understanding the conditions one has as a patient and what the future may bring which can help shape the conversation around preferences
Anna Burhouse 2 Jul 2019
Hi Seema,
great idea. I’d happily help with ideas about the design and it strikes me that a great starting place for patient involvement is People in Health West of England. The support they have given me in the past was wonderful. May be worth a chat.
warm wishes
Anna
Seema Srivastava 8 Jul 2019
Thanks Anna. I have contacted Tony Goring and Nathalie Delaney from WEAHSN and we met a fab local Patient Leader today to learn more from her about how best to develop this project. Thanks so much for your offer of support and will be in touch!
Jo Murray 28 Jun 2019
Hi Seema Great idea.
Identifying patients - I wonder if existing support groups would be a good place to start for example sepsis - if not already linked in to this you can access via https://sepsistrust.org/get-support
Also post ICU support groups via https://icusteps.org/support
This may also be of interest to the current Emergency Laparotomy project work via Patient Safety Collaboratives/AHSNs. I believe Medway are the only ones with a specific support group at present with others looking at establishing these. Contact Sarah Hare via twitter for more info @sarah_hare
Thanks
Jo
Seema Srivastava 8 Jul 2019
Thanks for those helpful suggestions Jo. We met a fab Patient Leader local to us today and explored how we may start inviting specific groups to have initial conversations about ReSPECT and capture themes which we could then suggest for co-designed ideas.
Comments are now closed for this post.