Q Exchange
Measuring social capital – do relationships create efficiencies?
- Idea
- 2018
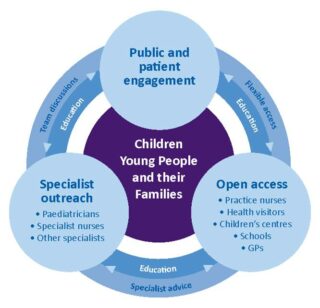
Connecting Care for Children (CC4C) is a Paediatric care programme that operates whole systems change across North West London. One of the core elements of CC4C are the Child Health Hubs that run in GP practices once a month, they bring professionals together to discuss clinical cases: the multi-disciplinary team (MDT) meetings are attended by GPs, Paediatric consultants, Health Visitors, School Nurses, CAHMs, Dietitians and Social workers. An exciting consequence of this is a wealth of interprofessional learning and the efficiencies that it creates within the healthcare system, be that immediate or), in the longer-term due to changes in clinicians future behaviour. The Child Health GP Hubs have developed networks of relationships among professionals, enabling them to function efficiently: this is often described as social capital.
Professionals working within the CC4C model anecdotally describe the positive effect that it has on patient care and professional learning. However, currently there is no validated method that demonstrates the increased value(financial or by patient outcomes), that social capital has on our healthcare system.
CC4C would like to design, develop and test a tool for measuring and promoting learning at each Child Health Hub. We would work with experts in design and systems change to formalise this process. At the moment any learning that happens is recorded by one junior doctor, which is then sent to the consultant for review and then disseminated to those that attended the MDT. There is no feedback loop or way of identifying the impact this has had on healthcare professionals and their clinical practice.
The clinics and MDTs were evaluated when the service was being established. Although the figures are small, and taken from one GP Child Health Hub, they are very positive: 15 professionals attended the MDT and discussed 154 cases; 59% of patients were managed through supportive advice and the care reminded with community professionals. 75% of the patients that were seen in the clinic had no paediatric follow up; in one hub 39% of new hospital appointments were avoided. The CC4C model now has 7 GP Child Health Hubs, consisting of 26 GP practices in North West London and we would predict that the outcomes for the new and existing Hubs would reflect the previous evaluation. However, to date there is no validated tool that evaluates the impact on the capability and confidence gained in those attending the MDT. Furthermore, the CC4C model design principles are now being used by other clinicians across the country, this provides oppotunity for us to understand impact of social capital on patients and healthcare professionals across the UK.
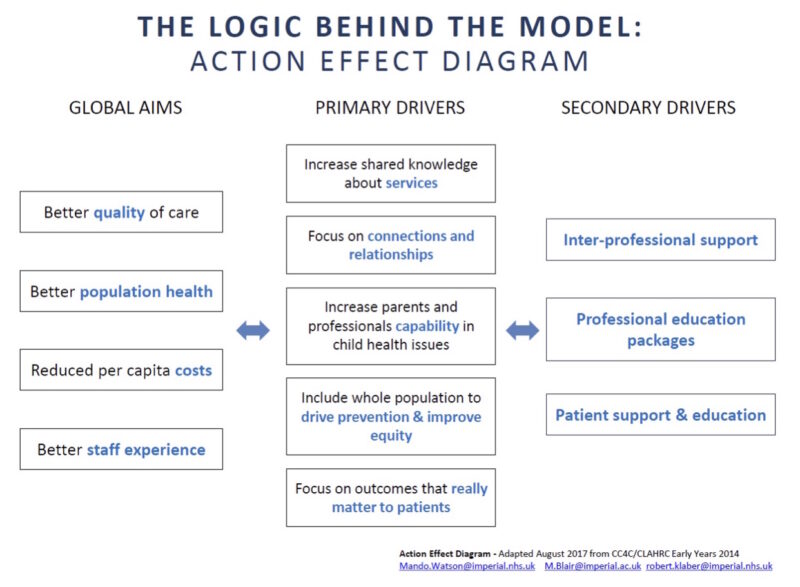
Our proposal is to develop a tool for measuring learning at the MDT meeting. This would build onto the logic models primary drivers of increased shared knowledge about services (signposting), increased capability, focus on relationships and outcomes that really matter to patients (patient centred care). This data would be captured and continuously tested using quality improvement (QI) methodologies. A stakeholder map would ensure that it is co-designed well and developed to a high standard. This funding would be used for the following:
• A designer
• Kit/equipment
• Workshop
• Clinician/MDT time
There are some minor variances between the Hubs therefore a SWOT analysis would help inform how the tool should be designed and how flexible it would need to be. Once the tools have been designed and developed we will test it using continuous PDSA cycles. The tool is likely to focus on confidence and knowledge; to do this accurately we would identify a learning framework and then map the data collected by the tool against this framework in the GP Hubs.
One of the three core elements of the CC4C model is ‘Open Access’ through a telephone and email hotline for GPs to quickly access specialist paediatric advice. This is outside of the MDT but it is another source of learning and interprofessional development, which is also not measured. Once the tool is developed for the MDT there is a desire for it to be used for other areas of communication.
The tool, once developed, would be tested in different settings, for example the Connecting Care for Adults MDT service, with the aim of creating a tool of universal applicability. At the moment we can’t predict what the tool will look like, or how it will work. However, once we begin to measure these anecdotal improvements, we can show the additional value of the MDT, and demonstrate the need for new models of integrated care with a focus on and investment in interprofessional support and multidisciplinary relationships.
How you can contribute
- Expertise in ethnography
- Systems change expertise
- Analytics