Change is happening at such a rapid pace in healthcare right now, maintaining and improving quality of care in this context is a real challenge for all of us.
I felt inspired by the #clapforcarers response to write a blog about team-working; specifically how we can help teams to come together for a common purpose, and how to look out for each other at a very difficult time.
Here are some principles and examples which have helped with team-working in our Acute Medical Unit recently and in the past. They may (or may not!) be useful in other settings, but I think it is important that we try learn from each other at this time.
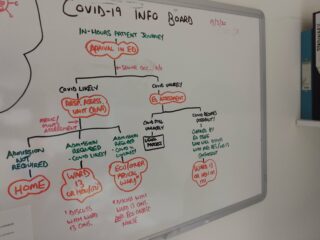
- Apply QI methods: Understanding your own system is vital and QI tools can help. Process mapping is one way of clarifying what your current processes are, and can help identify where improvement work could be focused. For us, process mapping allowed us to identify a weakness in our COVID stream triage process, which we were able to improve with quick PDSA testing. This enabled us to have a colour coded NEWS-based system, allowing for easy identification of unwell patients within our unit.
- Apply Joy in Work framework: We know medical and nursing staff find Acute medical on-calls difficult and stressful. To address this we applied the four-step Joy in Work framework, i.e.:
– Ask staff: “What matters to you?”
– Identify impediments to achieving What Matters “the pebbles in your shoes”
– Commit to improving joy in work
– Use improvement science to test approaches to improving joy in work
Our intervention was daily Staff Wellbeing Safety briefs, lasting 10 minutes with the on-call team; asking six questions to the team to identify issues arising on the day and deal with them at the time.
You can’t deal with everything in a 10-minute meeting but there were lots of quick wins
You can’t deal with everything in a 10 minute meeting but there were lots of quick wins, e.g. finding equipment, balancing workload distribution amongst the team and supporting colleagues with challenging conversations. We learned that 90% of staff felt the meetings were worthwhile, and the percentage of staff reporting having a “good day” increased by over 20% when the wellbeing briefs took place.
In 2019, the two biggest challenges identified by on-call teams were workload and arguments between specialties. Interestingly now, during the COVID-19 pandemic, the causes of stress are very different; different specialties are pulling together much more. The two biggest causes of stress now are:
- Anxiety regarding COVID-19
- Worry about changes to usual processes; staff worrying they will do things “the wrong way.”
Having identified what is causing anxiety, even if it can’t be fixed in a wellbeing safety brief, it is much easier to focus your interventions on things that can reduce that stress and anxiety if you know what is causing it. For example, to address the concerns regarding change to usual processes we introduced in situ simulation training on new resus algorithms during COVID-19, and how to process blood gases from COVID patients.
3. Build Resilience: Resilience Engineering is sometimes called ‘Safety-II’ or “learning from what went well”. We tried applying this to our unit’s morbidity mortality meetings. This involved identifying a real patient’s journey where processes of care have been performed very well, then displaying the anonymous story in our staff room, and then reviewing the case with the multi-disciplinary team. We called it, “Save of the Month”, and it has three main components:
- MDT Review of Case: what happened?
- Establish what went well from each discipline’s perspective – why did it go well this time?
- Agree at least one test following the review, to try to make that desirable ‘thing’ happen more reliably.
How this helps:
- Positive feedback helps staff morale
- The process allows us to identify work as done, rather than work as imagined
- It enables testing of ideas to make processes happen more reliably in the future.
An example from our first case was:
A sticker that we were trialling helped empower the clinical support worker (junior member of staff) to escalate appropriately. This was useful in providing us with meaningful information of the effectiveness of the sticker being tested and demonstrated the importance of having a flat hierarchy, which we subsequently worked on improving.
When it comes to trying to improve teamwork, use a method or framework, be positive and involve the whole multi-disciplinary team
We definitely don’t have perfect team-working in our unit, we have a lot to learn and have a long way to go. However, I thought some of what we have learned might be useful for other teams in a similar situation to us, so thought this was worth sharing. Thank you for reading it!
In summary
When it comes to trying to improve teamwork, use a method or framework, be positive and involve the whole multi-disciplinary team.
I’ll leave you with two quotes that have stuck with me when it comes to thinking about teamwork:
- “You can’t understand most important things from a distance, you have to get close.” Bryan Stevenson
- From the janitor at NASA who replied when asked what his job was, “I’m helping to put a man on the moon.“
We all have an important role to play in the current pandemic. It is hard, but please keep up all the effort you are putting in, wherever you are!
To find out more about Calum’s methods for team-working, drop him an email or reach out on Twitter: @calumamcgregor