The last two years have been an exciting journey for me since I joined the Q community back in January 2018. I work as a GP in Portadown Northern Ireland and as a medical adviser for Health and Social Care Board (HSCB) in the Department of Integrated Care.
As part of the Department for Integrated Care, I have benefitted from working across professional boundaries; linking with commissioners and professionals in business support, pharmacists, dentists, opticians and fellow GPs as well as engaging across specialities in Secondary Care and Department of Health. We have a good team approach and relationships have been positive and supportive between each of these groups, especially when faced with challenging systemic problems. Towards the end of 2017, just as I had applied for Q, I was beginning to consider how I could replicate and transfer the positive collaborative relationships I find working in HSCB to my clinical practice.
Although under one roof, the practices worked in isolation, with no obvious bridging, socialising or support
I joined a large practice in Northern Ireland, in a shared building with six other practices, in 2016. Although under one roof, the practices worked in isolation, with no obvious bridging, socialising or support between practices. This is the same with local pharmacies; the number far exceeds that of practices in the town although they are scattered geographically throughout the town and local area. The siloed practice became even more evident when one of the practices collapsed and a GP colleague commented that they had never met the doctor who had been working on her own for months in an environment with more patients than she could handle following the resignation of her partner. One can only imagine how isolated that GP had felt and I am sure other GPs in similar positions across the UK could empathise.
A casual visitor to the modern premises would presume the building itself lends to more cooperative ways of working, but there is very little shared space and, more critically, there is no natural time for professionals to interact and provide peer support. In addition, I could see no interaction with other professionals outside of General Practice, little visible partnership working with secondary care. Everyone was under extreme pressure to manage the basic health care needs of the local population, with little time to come together creatively and collaboratively. I set about trying to form a Community of Practice (CoP) before fully knowing what a formal CoP actually was.
Building the Community of Practice
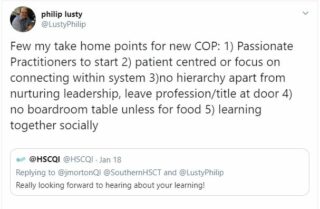
It was on the hottest night of the year, in June 2018, when England was playing Belgium in World Cup qualifier, that our Community of Practice Portadown met for the first time. We had initial participation from three practices and most of the local community pharmacies. The original idea was to meet socially around food (usually pizza), on a weekday evening, five times a year. In the early days I was working intuitively, and it is my natural style to lead democratically, building up a collective leadership for the group. I was aware that, at the start, I was the driving force, but I was keen that the work of leading should not be the sole responsibility of one individual. I found some willing candidates in the form of fellow Q member Jacqueline Morton (QI lead of Southern Trust), Helena Buchannan (Practice Based Pharmacist) and local community Pharmacist Raymond Anderson. We became the core conveners of the group.
 I was delighted in September 2018 to see the first-ever Communities of Practice Leadership Programme was being established in London and was even more delighted that my own leaders in HSCB, Assistant Director and Director of Integrated Care supported my application, alongside fellow convener Jacqueline Morton.
I was delighted in September 2018 to see the first-ever Communities of Practice Leadership Programme was being established in London and was even more delighted that my own leaders in HSCB, Assistant Director and Director of Integrated Care supported my application, alongside fellow convener Jacqueline Morton.
Commencing the programme was new and exciting and I hoped that whatever I learned and experienced would not only benefit me on my own CoP journey but also spill out to my role as Partner in Practice, Medical Adviser and other roles I serve in community and professional settings.
When we met for the first time and heard from Myron Rogers, I began to appreciate the science and psychology of a CoP. I realised that what we had started to create in Portadown was truly reflective of what a COP ought to be; the ownership of improvement needs to sit with the practitioners who are working and implementing on the ground, creating ways to help our local system lead and connect from within.
Sharing insight beyond the community
We have been able to share knowledge gained through this programme with over 40 GP practices as part of QI celebration share event and with fellow QI enthusiasts in RCGP Northern Ireland, at a Northern Ireland Conference and a Southern Trust QI conferences. A highlight this year has been welcoming programme facilitator, Cleo Butterworth, to Northern Ireland, at the WHO Challenge Medicine Without Harm Event and recently for a full day Communities of Practice event, sponsored by Health and Social Quality Improvement (HSCQI).
Whilst we have experienced highs and lows, I am convinced that CoPs are the only way to solve our problems
Whilst we have experienced highs and lows, celebrated our success and shared our concerns together, I am convinced that CoPs are the only way to solve our problems. It’s still a challenge to convince others of the importance of these collaborative networks, including funding and valuing the time of the members of the community. We are dependent on the goodwill of our small ‘coalition of the willing’ who are prepared to give precious time to come along for nothing (free pizza aside).
New bonds have been created between secondary care and primary care colleagues and a strong sense of support between the two. We feel more like ‘one’ with an increased desire to work together for the better of our community and benefit from the expertise from all parts of the system. To quote a senior colleague in Northern Ireland, Mark Taylor; “The system should be collaborative and not competitive.” I see CoPs as one of the few ways to genuinely achieve this.
I am so thankful for the new friends and colleagues I have met along the way and for the experience of getting to try out new tools in a safe environment both in London and back home. I have valued the different inputs from the diverse group of professionals and the fact that we hail from all over the UK. I want to thank Cleo, Sam, Q and the Health Innovation Network teams for organising the leadership training, their preparation, hosting and ongoing coaching/mentoring. I also want to thank the leaders within my own organisation who have supported me to participate in this UK wide programme. Most of all I want to thank the Pharmacists, GPs, Patient representatives and Trust colleagues who have journeyed with me as part of CoP Portadown.