Many Q members have found their work radically changed by the Coronavirus (COVID-19) pandemic. As part of our work to support health and care services to learn from the rapid innovation and improvement taking place during this time of unprecedented change, we are sharing brief interviews with members reflecting on their experiences.
If you’d like to share your story, please get in touch.
 What have you been working on in recent months to support COVID-19?
What have you been working on in recent months to support COVID-19?
As a paediatrician I have been working clinically and although children, as a population, have been mildly affected we have seen some severe cases. Despite the small numbers we have had to reconfigure the hospital and completely change how we work. Looking after ourselves, “the adults”, became a major priority in keeping the ship afloat as we were a risk for contracting and spreading the infection. We moved to working in pods to reduce the risk of spread between teams, and just as well as I became infected at the end of March. Thankfully, I had a mild illness, although I now fully appreciate the “brain fog” that has been described as it took a few weeks to start to think straight again.
Since returning to work I have joined several fellow consultants in providing support to our occupational health department as they have been overwhelmed by demand. It’s been a humbling experience to reveal the ‘village’ and all the background work that’s needed to care for a sick child that is sometimes hard to see.
 We’ve seen a big reduction in attendance at the Children’s Emergency Department with little evidence of delayed presentation or other negative effects. To some degree, this is down to the knock on effects of social distancing but we’re also trying to understand what it is highlighting about the needs of patients and families, and how we might improve services.
We’ve seen a big reduction in attendance at the Children’s Emergency Department with little evidence of delayed presentation or other negative effects. To some degree, this is down to the knock on effects of social distancing but we’re also trying to understand what it is highlighting about the needs of patients and families, and how we might improve services.
What positive change or adaption would you most like to keep after COVID-19, in the ‘new normal’?
Half of my job is providing QI education and knowledge support with the National Quality Improvement Team in Ireland. Much of this is done through training programmes in the application of leadership and improvement. Needless to say we have been knocked off course by COVID-19 and have had to radically adapt to the virtual environment with teams and projects that have been disrupted. While I hope we can return to some face to face interaction, the potential of virtual teaching has been revealed and important opportunities have been discovered, especially nationwide. We are finding new ways of engaging and changing the nature of the programmes, trying to develop more peer coaching and encouraging shared discovery.
We are finding new ways of engaging and changing the nature of the programmes, trying to develop more peer coaching and encouraging shared discovery
I became a co-host of a webinar series with the Institute of Leadership at the Royal College of Surgeons in Ireland (RCSI) called “Conversations that matter”. I love the medium of radio and podcasts because the long interview format allows for an in-depth exploration of important topics. We sought to consider the pandemic from the perspective of ethics, quality and compassion which differs from other webinars. We broadcast weekly from April to the end of June covering the impact of COVID-19 on issues such as person-centredness (patient and staff), equity (homelessness and prison care), compassionate leadership and use of the Arts as a way of responding to the crisis. I hope we’ll be back for another series in the autumn.
What have you learned about delivering change at pace?
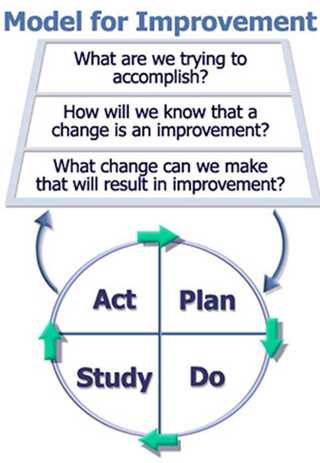
I think there is a belief in healthcare that QI theory and methods need stability and time to be applied. However the thinking is very flexible and can be used in any setting once adapted. In the pandemic the challenge for improvement has been to design better and learn faster without disrupting processes. I put these thoughts on paper at the beginning of the crisis in order to get my thinking straight. I shared it with colleagues who agreed and suggested I submit it; it was published in the International Journal of Quality in Healthcare last month!
How has your Improvement approach proved valuable?
We have taken a QI approach to adapting our teaching programme; collectively generating ideas, testing at small scale, gathering feedback, reflecting and tinkering before the next iteration. It has proven to work well.
What has particularly inspired you?
My colleagues, especially those newly qualified, working in adult care and public health have carried the greatest burden – they’ve been outstandingly courageous. A special appreciation also for Dr Mike Ryan at the WHO; he has remained an unwavering, unflappable, rock of sense through it all.
Is there anything you can share that you’d like to collaborate with other improvers on?
I think the area of teaching QI skills virtually, especially those where we use games or other immersive experiences to enhance learning. For example, using potato head to teach PDSA or measuring a banana to emphasise the importance of operational definitions. I would be interested in a Q collaborative to see how we can teach these concepts and skills online.
Join the Delivering Virtual Training Special Interest Group to join the discussion on how the Q community is taking QI learning online.